To Peel or Not to Peel?
Does peeling the ILM when removing the ERM lead to better outcomes? That is the question
If a patient presents with an epiretinal membrane (ERM), it’s likely that they’ll eventually undergo vitrectomy and an ERM peel as treatment. In recent years, an increasing proportion of surgeons have added in another step: staining and peeling of the internal limiting membrane (ILM) (1). The belief is that removing the ILM helps reduce the chances of an ERM recurrence, as this removes any residual ERM cells that might have been left on the surface of the ILM, and that the ILM can act as a scaffold for their proliferation. On the other hand, ILM peeling is known to cause mechanical trauma to the retinal nerve fiber layer, but the effects are transient, and don’t appear to affect visual outcome. But most studies assessing the pros and cons of peeling are retrospective – and inconclusive.
A team of researchers from Thessaloniki and Athens in Greece, and Moorfields Eye Hospital in the UK decided to try to obtain a more definite answer to the question “to peel or not to peel?” They performed a randomized controlled trial that compared the functional and anatomical outcomes of eyes (n=102) of patients (n=102) that underwent an ERM peel, with (n=50) or without (n=52) ILM peeling (2). All patients were aged ≥18 years, with an OCT-confirmed idiopathic ERM, binocular distortion, BCVA of ≤90 ETDRS letters, and intraocular pressures of ≤23 mmHg.
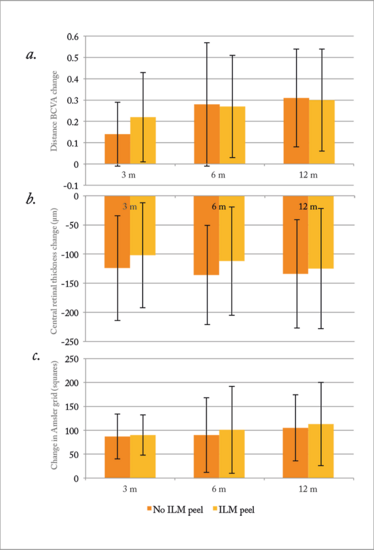
Figure 1. Change from baseline values at post-operative months 3, 6 and 12 for (a) BCVA, (b) central retinal thickness, and (c) Amsler grid squares. BCVA, best-corrected visual acuity; ILM, internal limiting membrane. Error bars: standard deviation.
At 12 months after surgery, the mean change in distance BCVA was 0.30 ± 0.24 LogMAR (15 ETDRS letters) in the ILM peel group, and 0.31 ± 0.23 LogMAR (14 ETDRS letters) in the non-peel group
(Figure 1a). The differences in distance BCVA, central retinal thickness and metamorphopsia between the two patient groups were not found to be statistically significant (Figure 1b, c) – suggesting that ILM peeling provides no additional benefits to patients undergoing an ERM peel. No ERM recurrence was seen in either group, although the length of follow up (12 months) may not be enough to rule out of the possibility of recurrence in some patients. However, a greater proportion of patients experienced anatomical disturbances (the formation or persistence of intraretinal cysts) in the ILM peel group, but this did not appear to affect visual outcomes.
The study authors concluded that ILM peeling doesn’t result in better outcomes following ERM removal, and that ILM removal may have some downsides too.
- S Chang et al., “Double peeling during vitrectomy for macular pucker: the Charles L. Schepens Lecture”, JAMA Ophthalmol, 131, 525–530 (2013). PMID: 23579603.
- P Tranos et al., “The role of internal limiting membrane peeling in epiretinal membrane surgery: a randomized controlled trial”, Br J Ophthalmol, [ePub ahead of print] (2016).
I have an extensive academic background in the life sciences, having studied forensic biology and human medical genetics in my time at Strathclyde and Glasgow Universities. My research, data presentation and bioinformatics skills plus my ‘wet lab’ experience have been a superb grounding for my role as a deputy editor at Texere Publishing. The job allows me to utilize my hard-learned academic skills and experience in my current position within an exciting and contemporary publishing company.













