
Faisal Ahmed (Credit: All images supplied by the author)
Glaucoma remains the leading cause of irreversible blindness in adults worldwide. Traditionally, glaucoma drainage devices (GDDs) have been the mainstay treatments for managing intraocular pressure (IOP) in patients with advanced glaucoma and in those for whom other treatments have been unsuccessful. However, GDD procedures are often associated with significant risks and complications.
The advent of Rheon Medical’s eyePlate-300, and the development of a novel technique known as minimally invasive tube surgery (MITS), offer a less traumatic and potentially more effective solution. The eyePlate was originally designed to be used with the eyeWatch system, an adjustable glaucoma drainage implant that allows surgeons to modify IOP noninvasively following the implantation of a nonvalved tube shunt. Made from silicone, the eyePlate is available in two sizes, the eyePlate-200 and the larger eyePlate-300. The tube has the same internal and external diameter as a standard Baerveldt or Ahmed FP7 GDD. The plate is almost square in shape, meaning it can still have a relatively large surface area with a smaller width, allowing it to fit just between the recti muscles,with the width of the eyePlate-300 being almost nearly half the width (18.5mm) of the Baerveldt 350 at 32 mm. This negates the need for a large peritomy and recti muscle slinging, which is more tissue-traumatic. The plate is thinner than the Baerveldt or Ahmed FP7, which should lead to lower bleb heights and thin bleb walls, associated with lower IOP. Additionally, the plate's flexibility means it sits flush with the sclera when sutured and can also be folded.
Surface area and bleb height
One of the critical factors influencing the success of GDDs is the surface area of the plate and the height of the bleb formed post-surgery. The larger the surface area and the lower the bleb height, the more effective a GDD is. The eyePlate-300 boasts a substantial surface area of 300 mm,² making it one of the largest available on the market, second only to the Baerveldt 350. This large surface area is crucial as it provides a more extensive interface for aqueous humor drainage, thereby enhancing the device's ability to lower IOP effectively. The almost square shape of the eyePlate-300 allows it to fit snugly between the recti muscles, while still maintaining a large surface area. Surgically, this means that the recti muscles do not need to be slung, unlike in conventional GDD surgery.
Bleb height is another critical factor in the long-term success of GDDs. Taller blebs are often associated with thicker fibrous walls and higher IOPs, whereas flatter blebs tend to have thinner walls and lower IOPs. The eyePlate-300 is designed to promote a flatter bleb profile. Its thinner plate (0.8 mm) compared to the Baerveldt (0.9 mm) and Ahmed FP7 (1.0 mm) allows it to sit more snugly against the sclera, resulting in a lower bleb height.
I was part of a group that published the first ever paper on the eyePlate 300 as a standalone GDD using the traditional limbal peritomy technique (1). The study showed promising results; 16 eyes were included, in which mean eye pressure was reduced from 31.5 mmHg to 10.7 mmHg. The mean number of drops reduced from 3.1 to 0.7; the results also showed that nearly 50 percent of patients did not require glaucoma drops at one year. No further surgery was required for lowering eye pressures at one year.
MITS: A novel surgical technique
Traditional GDD implantation techniques often require large conjunctival incisions and extensive manipulation of ocular tissues, leading to significant post-operative discomfort and longer recovery times. The MITS technique is less invasive. The eyePlate-300 is implanted through a smaller, less traumatic incision – the eye is retracted inferonasally to expose the superotemporal quadrant. A subconjunctival injection of bupivacaine with adrenaline is administered to ensure adequate exposure and induce hemostasis. A vertical radial incision is made 5 mm behind the corneal limbus, extending approximately 8–10 mm posteriorly. The eyePlate-300 is folded in half “taco style” (with a folded width of approximately 9 mm) and inserted through the small conjunctival pocket. Care is taken to unfold the plate under the tenons, ensuring it sits between the lateral and superior rectus muscles. The eyePlate-300 is then sutured to the sclera using a 9/0 prolene suture or a Gore-Tex suture. The tube is trimmed to a bevel and inserted into the anterior chamber via a sclerostomy made 2 mm from the limbus. A 3/0 prolene stenting suture is placed in the tube to also prevent post op hypotony and is removed in the clinic no earlier than 2 months post surgery. An occluding 7/0 VICRYL suture is tied around the tube to prevent early hypotony. A double layer of Tutoplast Allograft tissue is glued with Tisseel fibrin sealant, and the smaller radial peritomy is closed with Tisseel fibrin sealant glue and a 10/0 nylon suture. A subconjunctival steroid and antibiotic are administered to complete the surgery.

Figure 1. eyePlate-300.
Advantages of MITS
The MITS technique offers several advantages over traditional GDD implantation methods:
- Reduced tissue trauma. The smaller conjunctival incision preserves corneal limbal anatomy and reduces tissue trauma, potentially leading to faster recovery times and improved post-operative comfort.
- Minimized risk of diplopia. The narrow profile of the EyePlate-300 allows it to fit between the recti muscles, reducing the risk of post-operative diplopia.
- Improved cosmesis. The limbal architecture remains unaffected, improving post-operative cosmesis.
- Simplified procedure, The radial wound used in MITS is easier to close, requiring fewer sutures and reducing the risk of post-operative leaks.
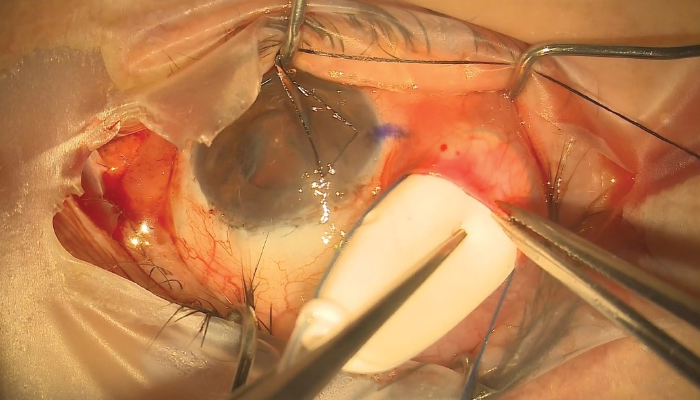
Figure 2. Insertion of folded eyePlate.
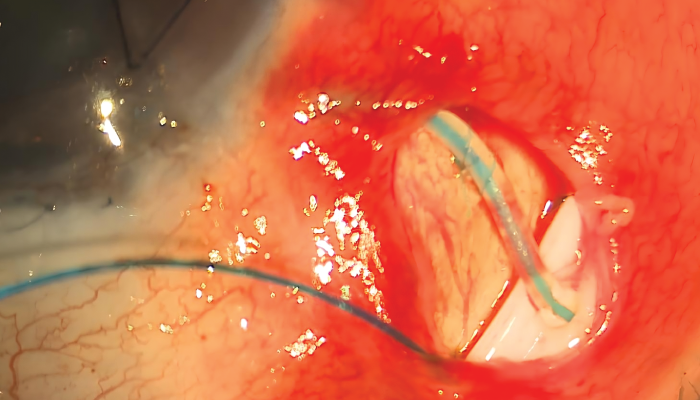
Figure 3. eyePlate sutured to sclera showing conjunctival opening.
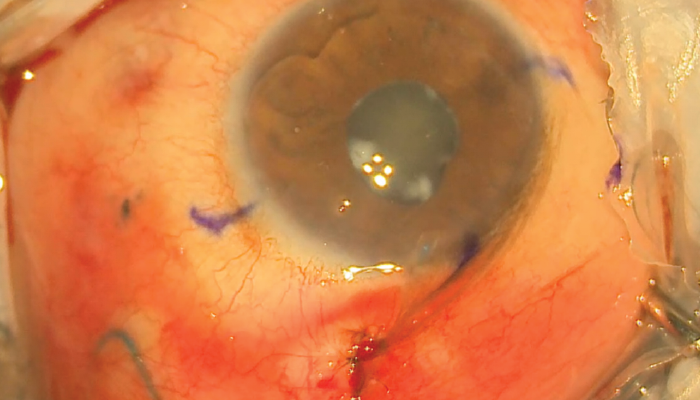
Figure 4. Closed linear wound.
MITS clinical outcomes
A retrospective analysis of 13 eyes implanted with the eyePlate-300 using the MITS technique showed promising results without the use of adjunctive Mitomycin-C (2). The primary outcome was successful, defined as achieving an IOP > 5 mmHg and < 21 mmHg without the need for eye drops. Secondary outcomes included best-corrected visual acuity at 12 months, complications, reduction in the number of drops, and the need for further pressure-lowering surgery.
Twelve eyes (92 percent) achieved a lower IOP. The mean pre-operative IOP was 35.69 mmHg, which was reduced to 11.08 mmHg post-operatively (p < 0.001). The mean pre-operative drops were 3.462, reducing to 0.85 at 12 months (p < 0.001). With nine of the 12 requiring no more than one IOP lowering drop at 1 year. There was no significant change in mean best-corrected visual acuity.
No intraoperative complications were recorded, and no further IOP-lowering surgeries were required during the 12-month follow-up period.
Conclusion
The eyePlate-300 and the MITS technique offer a new, less traumatic approach to glaucoma drainage device implantation. By reducing tissue trauma and improving post-operative outcomes, this method has the potential to significantly enhance the quality of life for patients with advanced glaucoma. Of note, Mitomycin-C was not used in any of the surgeries as a surgical adjunct. Further research and clinical trials will help solidify its place in the future of glaucoma management.
While the author is listed on Rheon Medical’s website as the first surgeon to use the eyePlate-300, he has no financial interest in the product or the company.
References
- F Ahmed et al., “Evaluating the Safety and Efficacy of a Novel Glaucoma Drainage Device in High-Risk Adult Glaucoma Patients: A One-Year Pilot Study,” J Clin Med., 13, 4996 (2024). PMID: 39274211.
- B Singh et al., “Minimally Invasive Tube Surgery (MITS) – A Novel Method in Glaucoma Drainage Device Implantation,” J Clin Med., 13, 6590 (2024). PMID: 39518729.
