
Priya Vakharia
As a medical student at Jefferson University in Philadelphia, I wasn’t expecting to become a retina specialist. That all changed for me during the retina training in my ophthalmology rotation, when I saw just how scared and vulnerable these patients are and how incredibly vital vision is to people's lives. I realized that, as a retina specialist, I would be in a position to truly make their lives better. It’s hard to overstate how central vision is to all of our lives. One report found that patients with advanced age-related macular degeneration (AMD) said that they would trade an average of 60 percent of their remaining life expectancy to return to normal vision (1).
Retina practices are increasingly busy, as we are fortunate to have not only standard-of-care anti-VEGF treatments with ever-improving durability and promising new agents in FDA clinical trials, but also, for the first time, approved treatments for our geographic atrophy (GA) patients too. However, in this fast-paced environment, it is easy to get caught on a hamster wheel of going from room to room, looking for fluid on OCT to decide whether or not to inject, instead of refining our techniques and treatment approach.
As a specialty, it is critical that we stay up to date on imaging advances and nuanced findings as this is what helps to prognosticate our patients and guide our treatments. OCT might show disorganization of the retinal inner layers (DRIL), for example, that can explain poor vision (Figure 1). Sun et al were the first to define DRIL and demonstrate a correlation between it and visual acuity in patients with diabetic macular edema, and its presence has been reported in various other retinal pathologies (2).
Outer retinal tubulation or ORT is a feature of photoreceptor rearrangement that can be a marker for disease progression (Figure 2). ORT is seen in a variety of degenerative retinal disorders, most commonly neovascular AMD (3). Their presence indicates disorganized outer retinal layers, irreversible photoreceptor damage, and a worse visual prognosis. We are still learning how other features, such as banded and stippling patterns, relate to faster progression (Figure 3).
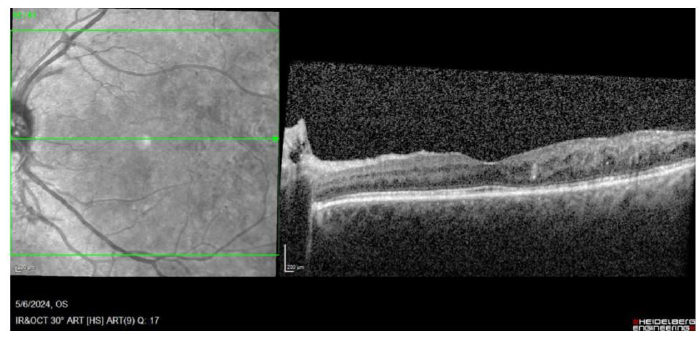
Figure 1. OCT of DRIL. Image courtesy of the author.
Commit to learning
The better that we are as a community at identifying signs of retinal disease earlier, the more effective we can be with targeted treatment. This requires a concentrated effort trying to stay on top of literature and research to understand where the field is headed. For example, there is an effort to move away from saying “choroidal neovascularization,” and instead referring to type 1, type 2, or type 3 macular neovascularization, as a way to help determine how aggressive we are with treatments (4). The more up to date we are, the better the care we can provide to patients.
Making time for education requires planning and prioritization. I like to listen to podcasts in the car and watch videos in my office on a break or during downtime in the OR. In eye care, there are a wide variety of options for getting information both online and by attending meetings in person. I find roundtable discussions to be particularly engaging, and I also like to run cases by my partners. Having that collaboration and exchange of ideas is a great way to stay on top of practice patterns.
Make your time count
As alluded to earlier, the biggest challenge we all have is time. I often say if I could have a superpower, it would be to control time. Sadly, I cannot control time, but I can optimize the time I do have. One way I do this is to make patients feel as if I have connected with them even if I am not giving them a lot of time. It might be as simple as putting a note in their chart about their children or pets and asking about them by name at follow-up visits. This small exchange makes patients feel like you know them and care about them.
Making sure to connect on a personal level with my patients also helps me stay engaged. It can be a challenge to be present with patients when you are going into the room, injecting them, and then quickly leaving for the next appointment. My patients are important to me, so I want them to feel that way.
Retina patients are "high touch" and require a lot of time for education – GA patients in particular. Often I will send them home with information and have them come back with their family. If I have to continue a conversation, I may call them on my commute home. For me, that's additional time that I can give to go over their questions or allay their concerns.
Outsource what you can
Outsourcing as many responsibilities as you feel comfortable with is a key way to handle time constraints and high volume. My staff, for example, talks to patients about treatment options, gives them the post-injection instructions, and makes sure they are using appropriate artificial tears.
Having staff that you trust and who are all working toward the same goal is a cornerstone of our ability to instill confidence in our patients. If you take good care of your patients and they are happy, your staff is also happy. My staff feel like they are making a contribution. For example, when patients come back from a retinal detachment repair and they are doing great, they want to express their thanks to the staff for helping them with the process of getting to the OR, and our staff appreciates that engagement.
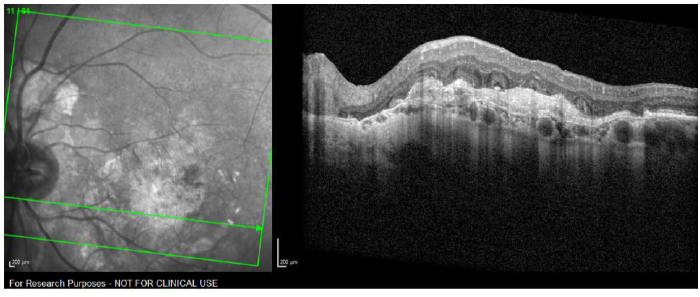
Figure 2. OCT of ORT. Image courtesy of Rosa Dolz-Marco, MD, Valencia, Spain.
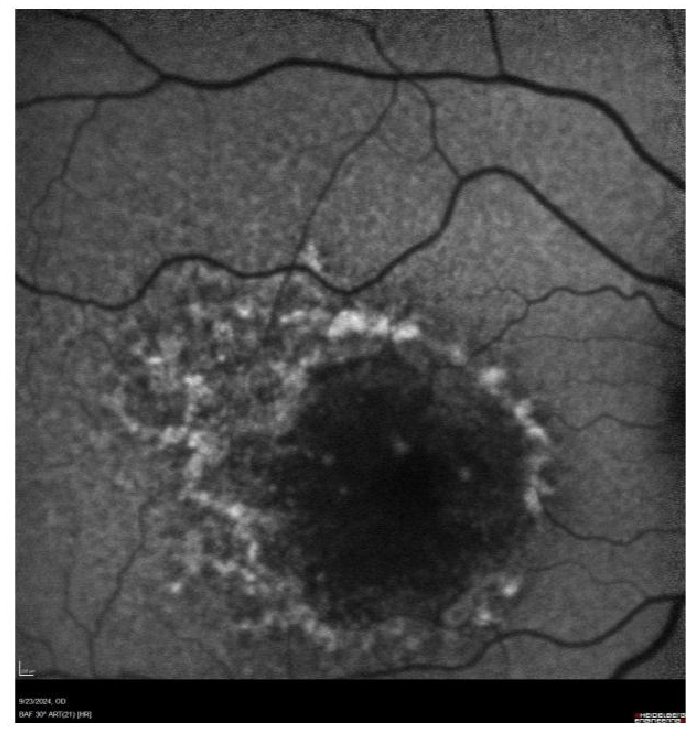
Figure 3. BAF - banded stippling. Image courtesy of the author.
Technology for efficiency
When going from room to room, studying OCTs looking for fluid, we may need a reminder as to what exactly has been going on with each patient. I use the Heidelberg Engineering SPECTRALIS OCT, which has a Progression Report feature that allows me to preview or print all of a patient's past OCTs. I can quickly understand their fluid over the past six months, for example, without having to wait for each individual image to load. I can have my staff tee it up for me when I walk in. That has been really helpful for me to decide therapeutic strategy.
Along with OCT, EMR is essential for helping us track disease over time and contributes to day-to-day efficiency. Backend workflows assist in managing things like drug inventory and prior authorization which have helped our staff streamline their workflow. They can plan for the week ahead and ensure we are as prepared as possible.
Keeping it real at home
For all of us, this notion of work-life balance is something we strive to achieve in a way that works for each of us. I have two small kids, so for me, some days are better than others! Some days, I am able to go home and just spend quality time with them, and on others, I'm pulled in competing directions. It doesn’t always work perfectly, but when I am with them, I put my phone away to just be with them. Ultimately, nothing is more important than our mental health and our families.
Someone once told me that your kids will never remember that great talk you gave or that extra patient you saw or that complex surgery you did. But they are going to remember if you showed up to their baseball game. That thought really resonated with me, so I try to stay present for them. It's not easy, but we cannot hesitate to prioritize the things that are important in our lives, including ourselves.
References
- 1. MM Brown et al., “The burden of age-related macular degeneration: a value-based analysis,” Curr Opin Ophthalmol., 17, 257 (2006). PMID: 17057801.
- 2. JK Sun et al., “Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema,” JAMA Ophthalmol., 132, 1309 (2014). PMID: 25058813.
- 3. A Arrigo et al., “Outer retinal tubulation formation and clinical course of advanced age-related macular degeneration,” Sci Rep, 11, 14735 (2021). PMID: 25635579.
- 4. RF Spaide et al for the Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group, “Consensus nomenclature for reporting neovascular age-related macular degeneration data,” Ophthalmology, 127, 616 (2020). PMID: 31864668.
