Adding Another String to Your Bow
How and why I started offering laser vitreolysis at my practice
At a Glance
- Laser vitreolysis-based floater treatment has existed for years, but a number of issues – principally, suboptimal visualization of the vitreous – limited both their success and adoption rates
- Today’s multimodal Nd:YAG lasers allow the entire vitreous to be clearly visualized and can pull “double duty” – standard procedures (like Nd:YAG capsulotomies) and laser vitreolysis too
- If you scratch the surface, there is a considerable volume of patients that want to have their floaters dealt with
- I share the story of how I added modern laser vitreolysis to my practice, and the lessons I learned along the way
Around 30 percent of the general population have symptomatic floaters, yet the impact of this common visual phenomenon on patient quality of life remains grossly underestimated (1). Few cataract patients presenting with visual dysfunction, such as glare and poor night vision, are expected to tolerate and grow accustomed to their symptoms, yet this remains the standard response to patients with floaters who present with a similar level of debilitating visual impairment. This “wait and see” approach does not stem from a lack of effort from ophthalmic professionals – for most the treatment options really are wait-and-see or vitrectomy – and the latter procedure isn’t without risk either (2). But there is a third option: laser vitreolysis. This procedure has been around for years, but perception was that the risks mostly outweighed the benefit of the procedure, and this rendered it a very niche offering. However, in recent years, significant technologic strides have taken laser vitreolysis from a potentially risky treatment option for floaters to a potentially very beneficial one instead.
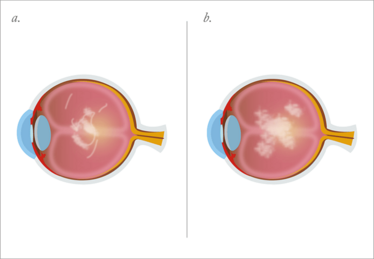
Figure 1. Schematic diagrams depicting a Weiss ring (a) and an amorphous clump (b).
Selecting the right patient
While almost everyone will be affected by floaters throughout their lifetime, in clinical practice, the focus is always on those with disabling floaters.
The type of floater that patients – both phakic and pseudophakic – present with most frequently is the Weiss ring (Figure 1a; Figure 2). As these are often located in the middle or posterior vitreous, they are easy to see and typically straightforward to treat, regardless of lens status – and eliminating them results in very satisfied patients even after a single treatment. I have found in my practice that younger patients – in their 30s, 40s and 50s – and postoperative cataract surgery patients more commonly present with amorphous clumps (Figure 1b). As large masses, these types of floaters have a significant impact on patients’ daily lives, especially in patients who may rely on high levels of visual function to do their job. It is not entirely clear why postoperative cataract patients often complain of floaters, but it has been suggested that these patients may have a lower tolerance for floaters due to an expectation of perfect vision after surgery, or because they have a clearer media after lens replacement.
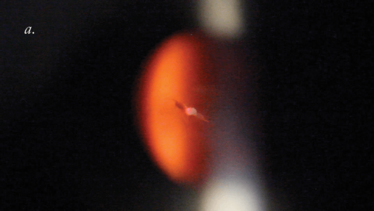
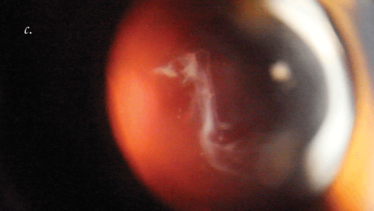
Figure 2. Weiss ring floaters viewed on axis (a, b) and a large floater viewed on partial axis (c). Credit: Inder Paul Singh.
When considering laser vitreolysis for floater removal, I have found it essential to select the right patients – and there are three components to this. Firstly, I never treat a patient who doesn’t have any visual complaints from their floaters. Secondly, I only perform the procedure on patients who have had symptoms without resolution for at least 4–6 months. Thirdly, I only treat floaters that I can clearly see, so it’s important that the location, size and density of the floater can be visualized. If it’s located close to the nerve, retina or phakic lens, and it doesn’t move after asking the patient to look up, down, right and left, I tell the patient it’s not safe to do the procedure. Instead, we wait until a future date to see if the floater has moved.
I also think it is essential to manage the patient’s expectations of the procedure. An analysis carried out by my practice has shown that one laser session adequately dissolves a single Weiss ring in more than 90 percent of patients (3), but when the floater is a large amorphous clump that is very dense, it can take 2–3 sessions to achieve near 100 percent patient satisfaction. This is simply because the laser creates a small plasma reaction rather than a large explosion, so the 400–600 shots delivered in a single session may only get rid of 50 or 60 percent of a very large dense clump. Alternatively it may break the large floater into smaller pieces that become troublesome a few months down the line. It is therefore important to advise all patients with a large amorphous clump on preoperative examination that they are likely to need a second or third treatment session.
Also key to setting patient expectations is “painting a clear picture” of how the procedure is performed. Many patients hear the words “laser treatment” and envisage a long, painful procedure with a convoluted aftercare regime. I make sure all of my patients understand that floater removal is an in-office procedure that takes on average less than 10 minutes, and has no post-operative recovery period, pain, patches or eye drops. I have found that explaining the procedure to my patients helps them realize it really is a minimally invasive procedure that lets them go about their daily life straight away, and this decreases their apprehension and makes them feel more comfortable.
Targeting floaters
To date, I’ve performed over 1,400 laser vitreolysis procedures and have found clear retinal visualization imperative for safe and successful floater removal, as a surgeon needs to be able to see where the retina is to obtain much-needed spatial context. In my practice, I use a multi-modal Nd:YAG laser (Figure 3), and although this works just like a standard Nd:YAG laser, it is more suitable for safe and effective floater destruction because the aiming beam, laser and light source in the slit lamp visualization tower are all coaxial – something that ensures its user can view floaters in the middle of the vitreous and posterior segment, all the way to the retina. In comparison, standard Nd:YAG lasers may only visualize vitreous behind the posterior capsule, meaning they cannot effectively target floaters (as these mostly reside between the middle and posterior vitreous). Other benefits of a multimodal Nd:YAG laser for vitreolysis include the ability to visualize anterior floaters (which is crucial in phakic patients to ensure that the lens is not “hit”) and improved safety over standard Nd:YAG lasers. This is because standard Nd:YAG lasers have energy beam profiles that follow a Gaussian curve, whereas the newer laser that I use has a truncated 3 ns energy beam, which improves efficiency by decreasing the amount of energy dispersion in the eye, meaning lower energy laser beams can be used to vaporize floaters. The nonlinear relationship between energy on the laser and amount of energy dispersed in the eye also means that we can increase the energy level of the laser and not worry about too much energy in the eye – for instance, a change in energy level from 1 mJ to 5 mJ only increases the convergence zone from 110 to 115 µm.
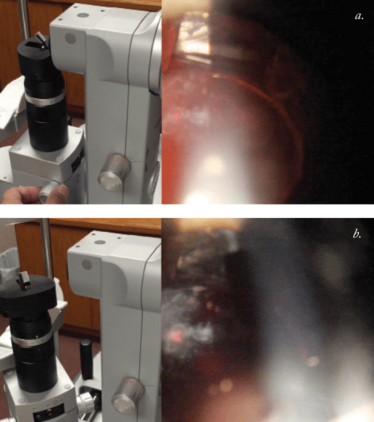
Figure 3. The Nd:YAG multimodal laser in use and the view through vitreolysis lens showing the laser targeting of floaters in a patient’s eye.
Performing laser vitreolysis with a multimodal Nd:YAG laser is very similar to performing laser peripheral iridotomies and capsulotomies with a standard laser, where a lens, viscoelastic agent, topical anesthetic and preoperative dilation are all required. The only real difference between the conventional procedures and laser vitreolysis is understanding the visualization through the laser and lens, and this can involve a little acclimatization. The most effective way of getting used to this type of visualization (just as with any other procedure) is simply to practice. It can take up to 20 cases to feel really comfortable with going up to higher energies and visualizing the floaters. My advice to those who are new to the procedure is that it all begins with the retina. If you view the vitreous and notice that both the floater and the retina are in focus, you’re too close to the retina. If the floater is in focus but the retina isn’t, you can feel confident that you have enough spatial context to fire the laser without damaging the retina. Viewing the floater through the vitreolysis lens during the preoperative exam can also allow the surgeon to get used to what it looks like before beginning the procedure. Another tip for visualizing floaters is to use a higher level of magnification. While I use around 10x magnification for capsulotomies, I go up to 16x magnification with vitreolysis lenses because this provides the best view of both the retina and the floater, and ensures sufficient spatial context to confidently and safely vaporize the floater.
Growing your practice with a multiuse laser
Introducing a multimodal Nd:YAG laser into my ophthalmology practice three years ago has proven immensely beneficial, not only in terms of profitability, but also for staff morale, patient satisfaction and the overall reputation of the practice. As a single device that can be used for all Nd:YAG laser-based eye procedures, as well as laser vitreolysis, it has provided a new stream of patients and revenue to our practice. While several sources for obtaining this new stream of patients exist, local optometrists and ophthalmologists are an invaluable source, particularly when you are just starting out.
Using a multi-pronged approach is ideal for maximizing the impression your clinic makes on such referrers. When I treat a patient who also sees an optometrist, I always encourage them to go back and let their optometrist know how happy they are with their results and how easy they found the process. I do the same thing for primary care physicians. Happy patients are the best testament of the efficacy of the procedure and if they return to their optometrists and ophthalmologists full of praise for laser vitreolysis, that puts a practice in a great position to receive future referrals from these local sources.
Secondly, when I first started to offer the procedure I held a few seminars to help educate local optometrists on floater removal with laser vitreolysis. These were structured as continuing education (CE) credit lectures, in which I shared procedure videos, patient testimonials, and addressed questions and misconceptions about the procedure. This was in addition to sending out email-based newsletters and distributing pamphlets to the area’s optometrists to further educate. Adopting these types of strategies as well as encouraging patients to be vocal about their results and satisfaction have proven to be really effective at driving referrals. We also wrote articles for local newspapers informing the public of this procedure that were also published online.
It is also important to realize that a sizeable amount of target patients may already exist within your patient database. I relied on educating my own staff to generate those first few patients because I realized a lot of the patients who stood to benefit from floater removal were already in our practice. However, as these patients with disabling floaters had spent years being told that nothing could be done about their floaters, they had conditioned themselves to never tell their eye doctor about them. It was therefore important to encourage my staff to start letting existing patients know that something could now be done for them, and for me to do the same. Indeed, the first 100–200 patients I treated were from my own practice database. If I spotted floaters during an examination, I simply started asking patients if the floaters bothered them. I was amazed at how often their eyes lit up and they said: “You mean you can remove them? Really? Let’s go for it!”
Destined for great things
I truly believe that laser vitreolysis with multimodal Nd:YAG lasers is set to become a popular procedure within ophthalmology practices. The key thing to understand is that today’s laser vitreolysis is not the same procedure as that of the past. Some doctors may be apprehensive because they’ve heard about low success rates, but this relates to old technology. It’s analogous to cataract surgery: the outcomes achieved by cataract surgery from 30 years ago quite simply do not compare what is achieved, as a matter of routine, today. The difference in efficacy and safety is staggering, and that’s because of the advances in the technology used. It’s the same principle with laser vitreolysis, in that multimodal Nd:YAG lasers deliver results that are worlds apart from those achieved years ago, and evidence of this can be seen by the number of satisfied patients who receive the procedure. A retrospective observational study performed within my practice involved 296 eyes of 198 patients with floaters (aged 38–89 years) and revealed a 93 percent satisfaction rate following laser vitreolysis (3).
It is clear to me that laser vitreolysis is set to become a popular procedure in ophthalmology practices and given the impact of symptomatic floaters on daily life, I am confident this change is one that will be greatly welcomed by affected patients.
Inder Paul Singh is President of The Eye Centers of Racine & Kenosha, Wisconsin, USA.
- BF Webb BF et al., “Prevalence of vitreous floaters in a community sample of smartphone users”, Int J Ophthalmol, 6, 402–405 (2013). PMID: 23826541.
- KF De Nie et al., “Pars plana vitrectomy for disturbing primary vitreous floaters: clinical outcome and patient satisfaction”, Graefes Arch Clin Exp Ophthalmol, 251, 1373–1382 (2013). PMID: 23250478.
- IP Singh. “Vitreous floaters - an under-appreciated and under treated problem: patient satisfaction and complications of YAG vitreolysis”. Presented at American Society of Cataract and Refractive Surgery Annual Meeting; April 17-21, 2015; San Diego.
Inder Paul Singh is President of The Eye Centers of Racine & Kenosha, Wisconsin, USA.













