The Efficacy You Expect for Your Glaucoma Patients
Glaucoma specialists discuss the efficacy of VYZULTA®, as proven in clinical trials – and the difference it is making to the outcomes of their patients
sponsored by Bausch + Lomb
Download article pdf
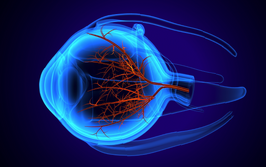
VYZULTA® (latanoprostene bunod ophthalmic solution) 0.024% is indicated for the reduction of intraocular pressure in patients with open-angle glaucoma or ocular hypertension.
Meet the experts
Quang Nguyen, MD, glaucoma and cataract surgeon, La Jolla, CA, USA
Gagan Sawhney, MD, cataract and glaucoma specialist, Eye Surgery Center of Georgia, Woodstock, GA, USA
Janet B. Serle, MD, Professor of Ophthalmology, Director of Glaucoma Clinical and Research Fellowships, Mount Sinai School of Medicine, New York, NY, USA
What is the current state of play in glaucoma – and how does VYZULTA fit into this picture?
Gagan Sawhney: Traditionally, when you think about aqueous fluid in the eye, most flows out through the trabecular meshwork, which becomes restricted in glaucoma. Unfortunately, the majority of drops primarily focus on the uveoscleral pathway. In VYZULTA, we have a drug that both acts on the uveoscleral pathway and promotes flow through diseased tissue.
What’s your experience with VYZULTA?
Quang Nguyen: From what I have seen, both during the APOLLO Study (1) and since then, the drug is effective and well tolerated. My usual strategy for glaucoma patients is monotherapy: choosing one drug to lower the patient’s IOP and continue to control it, and keeping them on it for as long as I can. VYZULTA fits this objective really well and most of my patients exceed their target pressure goals.
Gagan Sawhney: My experiences with VYZULTA have been fantastic. I regularly achieve IOP reductions of eight or nine points. The dual mechanism of action of VYZULTA not only promotes outflow, it also acts on the uveoscleral pathway and diseased tissue in the trabecular meshwork. When patients are not achieving their target on their current prostaglandin analog (PGA), we switch them to VYZULTA – it is now my goto medication. For me, success is defined by the answers to four questions: Is the IOP coming down? Are patients tolerating the drops? Are the drops affordable? Is the patient compliant? In my practice, VYZULTA results in a positive response to all four questions for most of my patients.
Which key outcomes have been particularly interesting to you?
Janet Serle: I have to say that it’s the efficacy; the two Phase III clinical trials, APOLLO and LUNAR (1,2) – in which VYZULTA, administered just once daily, was compared with twice daily timolol 0.5 percent – clearly evidenced efficacy. In these two studies, IOP was measured at nine time points during the first three months of dosing, at 8am, noon and 4pm during weeks two, six and 12 of dosing. The IOP reductions at these nine time points in the VYZULTA-treated group ranged from 7.5 up to as high as 9.1 mmHg – a greater reduction than in the timololtreated group. Additionally, reductions with VYZULTA ranged from 30 to 32 percent across all time points at month 3, which is a range we often set as a target for our glaucoma patients.
The patients enrolled in both these studies entered an open-label extension, for an additional three months (a total of six months) in the LUNAR study, and for an additional nine months (a total of 12 months) in the APOLLO study. During the open-label extension, IOP reductions remained stable over 12 months of dosing with VYZULTA, which showed long-term efficacy with chronic dosing.
Quang Nguyan, Gagan Sawhney and Janet Serle are consultants of Bausch + Lomb.
IMPORTANT SAFETY INFORMATION
- Increased pigmentation of the iris and periorbital tissue (eyelid) can occur. Iris pigmentation is likely to be permanent
- Gradual changes to eyelashes, including increased length, increased thickness, and number of eyelashes, may occur. These changes are usually reversible upon treatment discontinuation
- Use with caution in patients with a history of intraocular inflammation (iritis/uveitis). VYZULTA should generally not be used in patients with active intraocular inflammation
- Macular edema, including cystoid macular edema, has been reported during treatment with prostaglandin analogs. Use with caution in aphakic patients, in pseudophakic patients with a torn posterior lens capsule, or in patients with known risk factors for macular edema
- There have been reports of bacterial keratitis associated with the use of multiple-dose containers of topical ophthalmic products that were inadvertently contaminated by patients
- Contact lenses should be removed prior to the administration of VYZULTA and may be reinserted 15 minutes after administration
- Most common ocular adverse reactions with incidence ≥2% are conjunctival hyperemia (6%), eye irritation (4%), eye pain (3%), and instillation site pain (2%)
Click here for full Prescribing Information
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088
Find out more: https://www.vyzultahcp.com/

VYZULTA and the V design are trademarks of Bausch & Lomb Incorporated or its affiliates
©2020 Bausch & Lomb Incorporated or its affiliates. All rights reserved – VYZ.0156.USA.20 – Date of preparation: December 2020
Click here for Making a Difference with VYZULTA®
- RN Weinreb et al., “Latanoprostene bunod 0.024% versus timolol maleate 0.5% in subjects with open-angle glaucoma or ocular hypertension: the APOLLO study,” Ophthalmology, 123, 965 (2016). PMID: 26875002.
- FA Medeiros et al., “Comparison of latanoprostene bunod 0.024% and timolol maleate 0.5% in open-angle glaucoma or ocular hypertension: the LUNAR study,” Am J Ophthalmol, 168, 250 (2016). PMID: 27210275.