Probing the Limits
Intraocular distance sensor + surgical robot = better outcomes, safer procedures and speedier surgery
Tremor. It’s the surgeon’s scourge. You spend years training in medical school, years training after medical school, then you spend years in the operating theater honing your skills… And then age kicks in! Even the most experienced and gifted surgeons out there have to hang up their surgical hats once their hands start to shake – even very slightly. But even the best surgeon’s hands aren’t perfectly still, which makes certain procedures, such as dealing with friable retinal tissue or injecting a bolus of retinal gene therapy over an extended period, very challenging – and almost impossible for the human hand. The Ophthalmologist has already covered the rise of the robots (1)(2)(3)(4) – how they can filter tremor from the human hand, bring with it features like scaling of movements and micrometer precision, and how they can not only extend the careers of veteran surgeons, but also extend the ability to deal with the most challenging cases from the ‘rock star’ surgeons to everyone.
Famously, Preceyes B.V. (Eindhoven, the Netherlands) produced the first surgical robot to be used intraocularly in a live human patient – Oxford University’s Professor of Ophthalmology, Robert MacLaren used it to successfully perform an ILM peel (2; Figure 1). But, even at the time of the procedure, the company’s Medical Director, Marc de Smet, was considering an improvement: intraocular distance sensing. The robot now has that feature.

Figure 1. Robert MacLaren using the Preceyes robot for the first time in a live patient to perform an ILM peel.
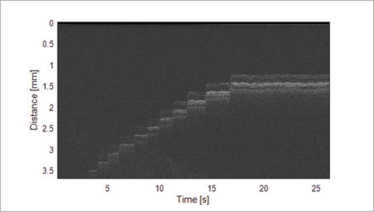
Figure 2. OCT A-scans, measured while the instrument approaches the retina in 200 μm steps. Movements due to heartbeat are visible (period ~1 s, amplitude ~40 μm), especially during periods where the instrument is at a standstill.
“Our new OCT-based intraocular distance sensor tells us the size of the retina”, explains de Smet. “For the moment, we are taking the images it generates and the distances it measures (Figure 2) to place a limit on how far the sensor goes in the direction of the retina. I believe we could use this to make injections into the subretinal space so much safer and more precise. Once we incorporate this in to different instruments, we will make them safer and be able to automate steps.”
The new distance sensor was successfully used in a clinical validation study at Rotterdam Eye Hospital (REH). What did the surgeons think? Lead investigator at REH, Koorosh Faridpooya, said that the “robot brings vitreoretinal surgery to the next level by maximizing the surgeon’s precision and control. Using this revolutionary sensor in the eye enables us to operate with enhanced vision and it supports the surgeon to improve surgery.” Matteo Cereda, a senior retinal surgeon at Rotterdam’s Sacco Hospital Eye Clinic, added, “Using the robot definitely makes me a better surgeon. I felt really safe using it and all movements of the surgeon become really precise. In combination with the sensor, accidental trauma to the retina can now be avoided. A robot with this sensor paves the way to new scenarios in eye surgery and new therapeutic approaches.”
Just how much of an advance is this, and what difference will it make? According to de Smet, “This sensor represents a highly significant milestone. It promises to enhance the surgical skills of retinal surgeons at all levels of training and experience. The robot-sensor combination promises to improve the safety, the outcomes and speed of everyday surgical procedures. Analysis of the data generated and stored during surgery will allow us to optimize surgical steps by providing training and evaluating surgical performance.”
- M de Smet, “Eye, Robot”, The Ophthalmologist, 15, 18–25 (2015).
- M Hillen, “Forging Iron Man”, The Ophthalmologist, 34, 18–29 (2016).
- R Steer, “The Bot that Busts Clots”, 38, 11 (2017).
- R Steer, “Micro Machines”, 36, 12 (2016).
I spent seven years as a medical writer, writing primary and review manuscripts, congress presentations and marketing materials for numerous – and mostly German – pharmaceutical companies. Prior to my adventures in medical communications, I was a Wellcome Trust PhD student at the University of Edinburgh.