Enlightening Images
Increasing clinical confidence through personalized assessment – with the SPECTRALIS
sponsored by Heidelberg Engineering
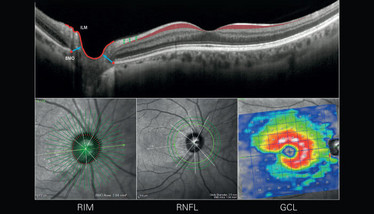
The SPECTRALIS® multimodal platform takes a holistic approach to glaucoma diagnosis and management. The Glaucoma Module Premium Edition (GMPE) detects the anatomical landmarks of each individual eye to provide accurate and precise measurements of the neuroretinal rim, RNFL, macular ganglion cell layer, as well as macular intra- and inter-eye asymmetry. The unique scan patterns are tailored to the anatomy of interest and powered with dual-beam live eye tracking, reliably supporting the clinician’s ability to distinguish glaucoma from other optic neuropathies and physiologic cupping.
How does it work?
Rim: GMPE takes each eye’s individual anatomy into account to provide an objective measure of the neuroretinal rim. It identifies the minimum distance between the internal limiting membrane and Bruch’s membrane opening (anatomic disc margin) around the optic nerve: Bruch’s membrane opening-minimum rim width (BMO-MRW). This objective rim assessment is sensitive and specific to detecting glaucoma across the entire disease spectrum. The BMO-MRW parameter is also a useful aid in the diagnosis and management of optic neuropathies beyond glaucoma.
RNFL: A dedicated 3.5 mm circle scan with 768 A-scans provides a reliable assessment of circumpapillary RNFL (cpRNFL) thickness. Clear and detailed views of the RNFL tissue in the OCT B-scan image allow for confirmation and adjustment of segmentation boundaries, delivering a high degree of confidence in the thickness measurements. In cases where abnormalities, such as parapapillary atrophy, protrude and confound the 3.5 mm cpRFNL results, the 4.1 mm and/or 4.7 mm high-resolution circle scans results can be used.
GCL: A full 10-layer segmentation of the retina provides an assessment of each individual layer within the macula. To complete the evaluation, SPECTRALIS isolates and evaluates the ganglion cell layer (GCL) independently from the retinal nerve fiber layer and the inner plexiform layer to confirm early patterns of glaucomatous damage that may present at only one of these layers. By assessing the GCL in isolation, clinicians can have confidence discriminating glaucomatous damage from that caused by other diseases.
Follow-ups: In cases where diagnosis remains uncertain – even after a holistic evaluation with OCT – close monitoring is key to identifying glaucomatous progression. Dual-beam live eye tracking delivers 1-micron precision, allowing clinicians to reliably detect even the smallest changes in disease progress.
Case Study: High-resolution imaging in glaucoma diagnostics
These images, provided by Donald Hood (Columbia University, New York) and Robert Ritch (New York Eye and Ear Infirmary, New York), were recently published in a Heidelberg Engineering Academy book: “Glaucoma Imaging Atlas”. They illustrate the advantage of seeing the retinal tissue in high-resolution with the correct segmentation – as well as the importance of pattern recognition.
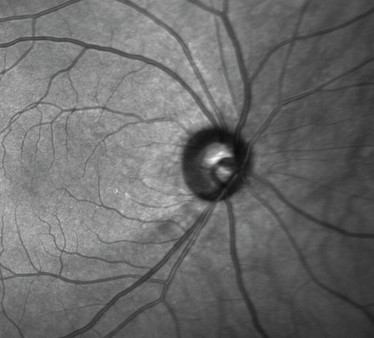
Figure 1: Confocal optics and infrared scanning laser show a TI RNFL wedge defect. This infrared image is obtained simultaneously with the OCT scan.
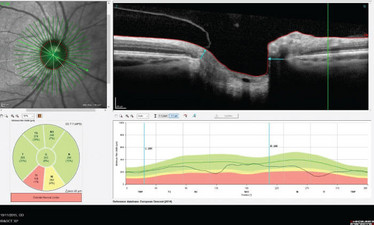
Figure 2: Rim assessment with BMO-MRW indicates neuroretinal rim thinning in the TI and NI sectors.
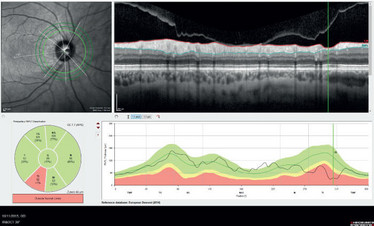
Figure 3: An RNFL wedge defect is seen on the B-scan and the RNFL profile. This is also confirmed in the sector analysis.
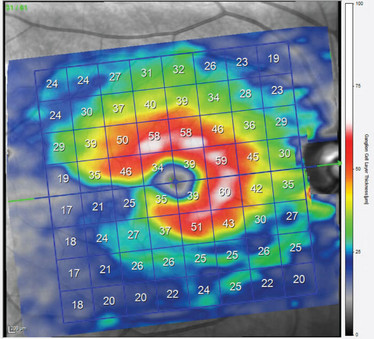
Figure 4: The GCL thickness color map shows classic ganglion cell notching and asymmetry across the horizontal mid-line (‘snail shell’ effect) that directly corresponds to the structural and functional findings.













