To watch the video interview with Gilad Litvin, click here or scroll down.
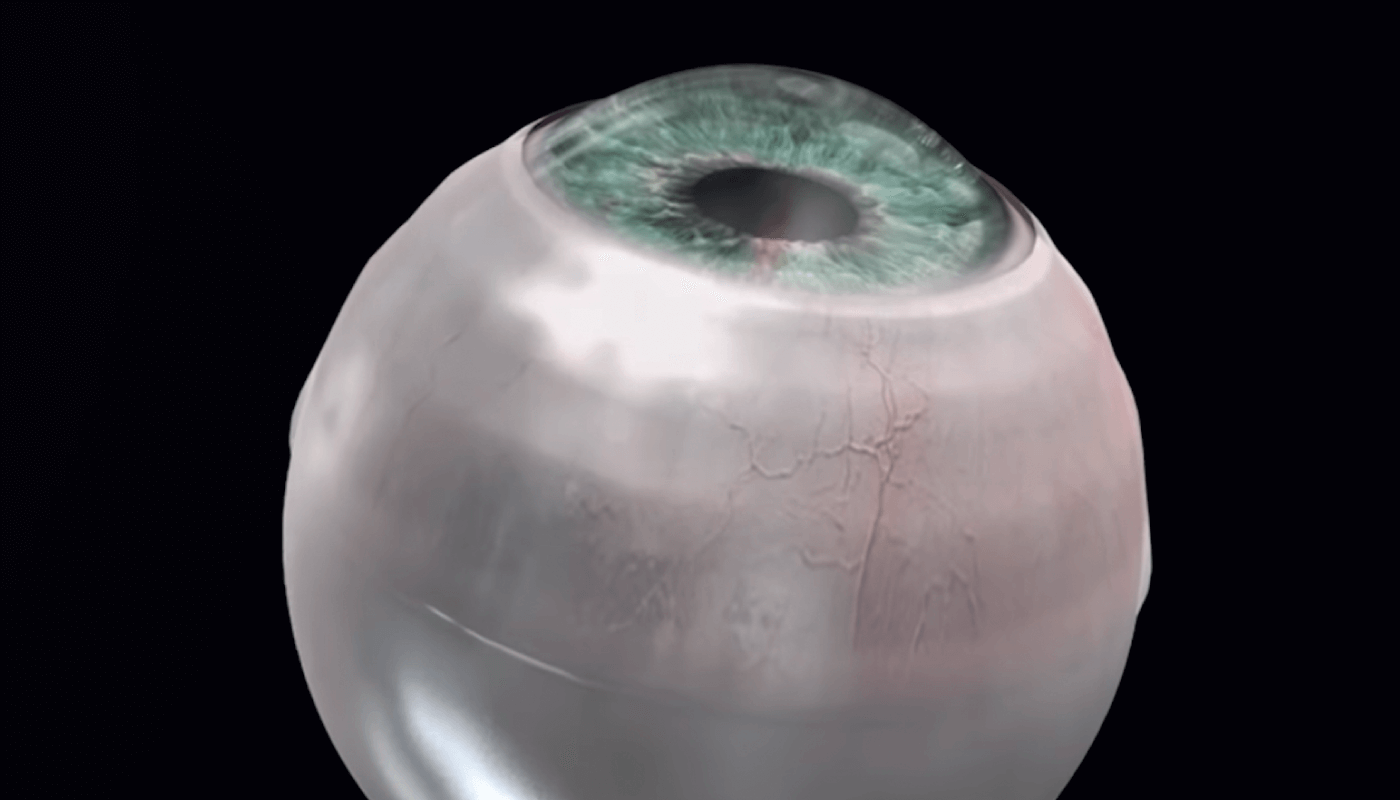
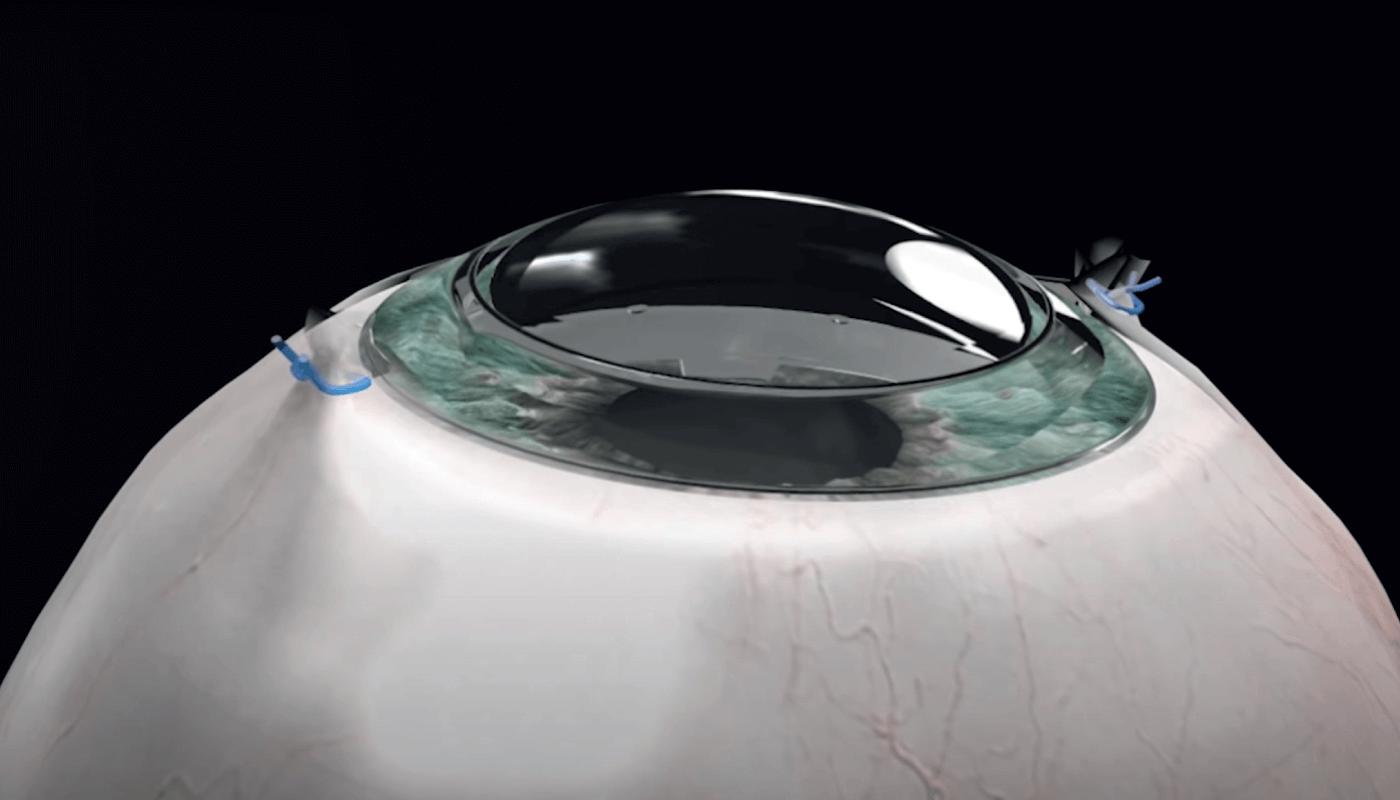
Corneal transplants are currently limited by multiple factors; one of them is the fact that 50 percent of the world’s population doesn’t have access to corneal tissue, another is that 20 percent of patients are not suited for a transplant due to medical reasons. A completely synthetic alternative that can be stored on the shelf and implanted in a simple procedure when needed can solve this issue. This is where the CorNeat KPro artificial corneal implant I invented enters the fray. As the implant is fully synthetic, it does not require sourcing of corneal tissue harvested from either humans or animals, and has the potential to enhance accessibility of corneal transplants. A hurdle to success when implanting an artificial corneal implant into the body is to fool the cells into accepting the synthetic materials as part of the native tissue – so a biomimetic material that stimulates cellular proliferation, leading to tissue integration, is needed.
This is like when a child buys an ant farm. When they introduce ants to the farm, the ants don’t know that they’re not in the wild, so they carry on farming and making their home as good as ants will – the cells are similarly fooled and grow into the synthetic matrix we’ve provided by embedding the CorNeat KPro into the body.
How it started… and how it’s going
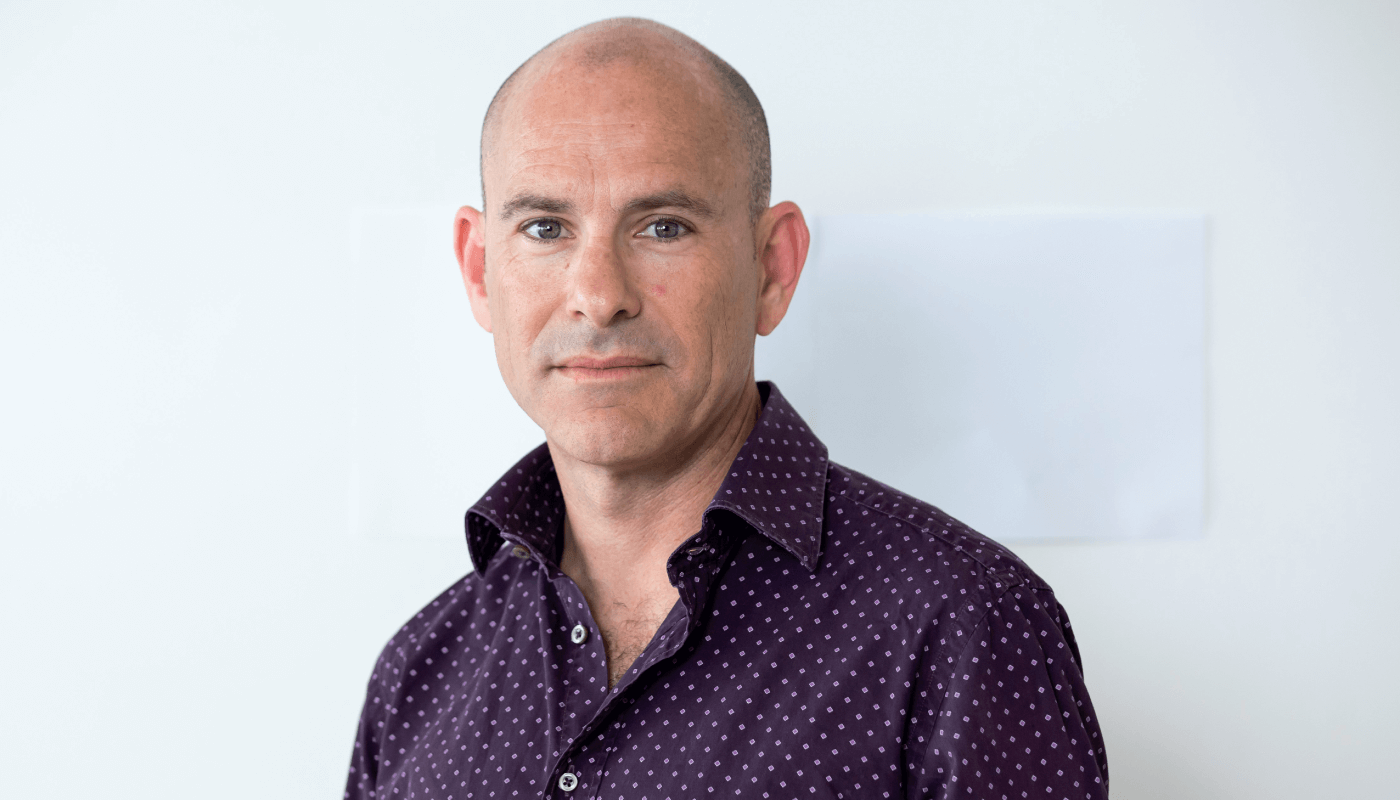
Following my residency and subspecialty training in retina, I followed a career in developing medical devices, and drafted my first patent during my last years working for the public healthcare system. Since then, I’ve devoted most of my time to developing these devices, and much less to practicing ophthalmology. Currently, I see patients and perform surgical procedures one day a week, with the rest of my time spent on innovating.
I drafted the patent for the CorNeat KPro around 2015. It then took five years, using my experience in chemical engineering and biology, to create this synthetic cornea that integrates into and is biocompatible with the eye wall – with no signs of inflammation or infection. It is now in clinical trials and has already been successful in restoring the sight of a 78-year-old man who had been legally blind for a decade. This patient has had stable visual acuity for over three months now. This has allowed him to see his grandchildren for the first time, use the dials on his phone, and make his own coffee among other things – which may seem small, but make a huge difference to his quality of life and independence.

The success of this surgical procedure may be due to the engineering perspective used, with the implant being integrated into the vascularized white part of the eye. All previous attempts at corneal transplants have focused solely on the transparent, non-vascular, and mostly acellular cornea, but implanting in that location can reduce the ability for the new tissue to integrate with the eye as a whole organ. CorNeat KPro benefits from being implanted into the vascularized white part of the eye, where even small inflammation can be seen due to the blood vessels’ presence, and the result is long-term and robust integration.
Apart from filling the gap of inaccessibility to corneal transplants, CorNeat KPro also showed immediate improvements on the outcomes of patient vision when compared to current standards. The synthetic nature of the implant means that it can be tailored to the specifications of the eye, whereas when using human or animal corneal tissue, the sutures must be made precisely and there are always optical distortions.
First in human
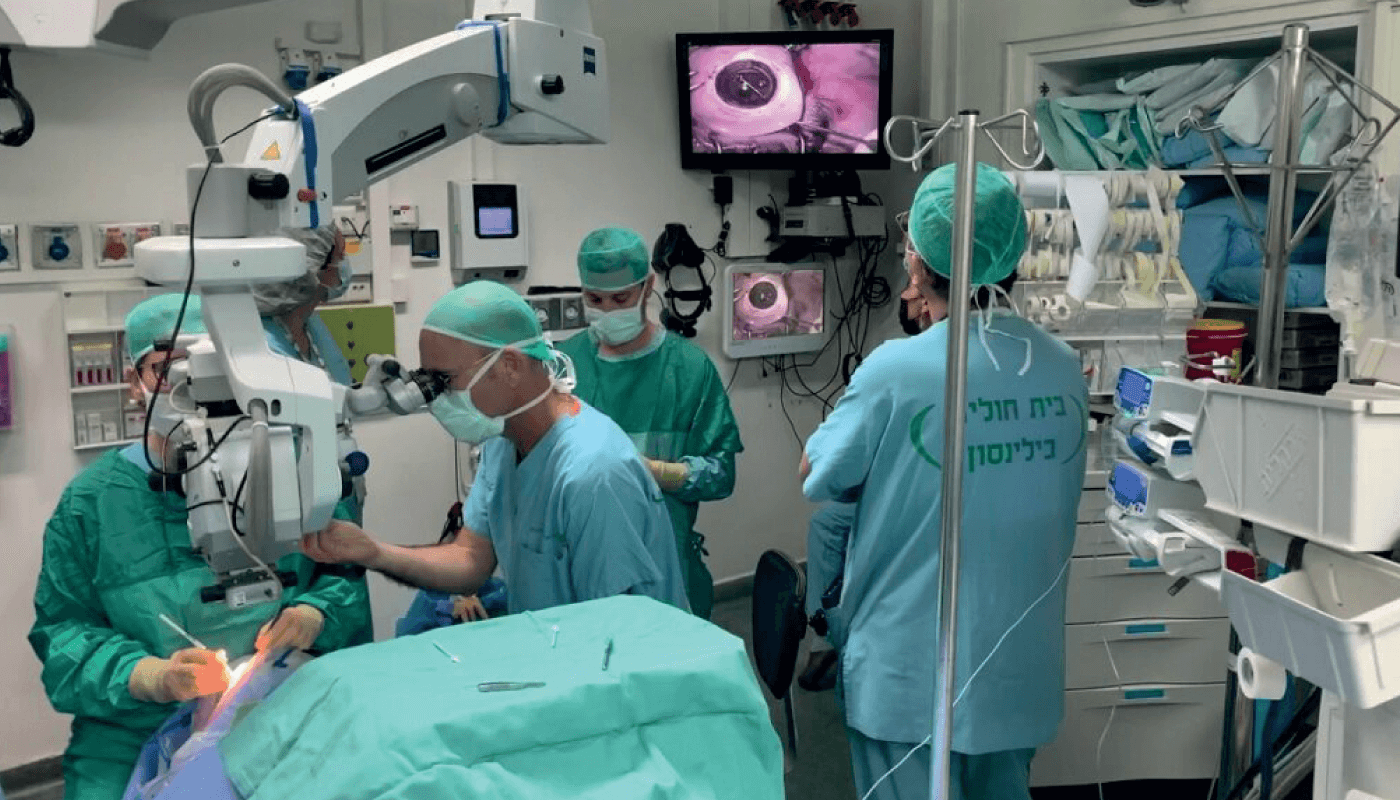
Renowned corneal surgeon Irit Bahar, Clinical Professor of Ophthalmology at Tel Aviv University and Chief Physician of the Department of Adult and Pediatric Ophthalmology at the Rabin Medical Center in Petah Tikva, Israel, is the principal investigator for the Phase I clinical trial, and she’s been heavily involved in patient selection and recruitment. This collaborative involvement has been very important to arranging the best selection criteria possible – as any disagreements led to discussion, which in turn led to establishing the final protocol. Bahar and an experienced assistant trained with me a couple of times prior to the surgery, and I was granted special disposition by the Ministry of Health to attend and advise during the surgery to ensure the technique was implemented correctly – I looked down the microscope every few minutes to check how it was going. In the end, it was a very straightforward, hour-long surgery. The next day, the patient told us he slept well and had no pain. He compared it with his previous experiences of corneal implantation, which were very painful for him. We hadn’t planned for our method to be less painful, but it turned out to be an additional advantage.
The moment when the patient’s bandages were removed was very moving, with a mixture of anxiety and excitement. It was a culmination of five years of hard work on an ambitious project. The realization that our previously blind patient could now read digits on a board brought tears to our eyes, and it seemed like the patient was the calmest one in the room – in reality he was quite shocked and it actually took him a couple of hours to fully grasp what had happened. When I talked to him later, he was very excited.

Looking ahead
We have received approval in Canada for CorNeat KPro, and we are starting trials at centers in Vancouver and Toronto. These trials are being led by local professors, all of whom are worldwide leaders in the field. We have further implantations planned in Israel. We have submitted requests for approval in The Netherlands, France, and with the FDA in the US. Altogether, we have submitted applications for implantations in 50 patients. Once we have completed 30 of them, the plan is to stop the trial, follow the patients up for a year, and submit the final request for FDA approval.
Once approved, the primary indications will be in patients whose previous corneal transplantations failed or who are not suitable for them, before we can fully test safety and efficacy in a larger trial.
CorNeat KPro is only one of many patents for medical devices that I have developed over the years, and there are more projects on the way. One of them is using advanced chemical engineering, similar to the CorNeat KPro, to try and imitate the natural drainage pathways in the eye using fully synthetic means. This also involves tricking the body into believing the synthetic component is biological so that it can be accepted and integrated into the tissue. The glaucoma drainage device imitates the apparatus and physiological pressure of the eye to make this possible.
The concept of using biocompatible and fully synthetic devices has also enabled our expansion into other areas of medicine. For example, there are initial steps to use them in periodontology for gingival recession, and we’ve been approached by orthopedic surgeons and gynecologists, among others. This has been our core competency, enabled by the creation of an artificial extracellular matrix, or micro-tissue skeleton, which – when placed within the body – fools the cells into growing and regenerating the tissue like they would normally, just like ants make their home in an artificial ant farm.
Watch The Ophthalmologist's interview with Gilad Litvin
