Long considered to be an extension of the central nervous system, we now have the technology to fully explore the retina’s role in predicting or diagnosing devastating neurodegenerative disorders.
As neuro-ophthalmologists, we are in pursuit of answers for our patients with unexplained visual loss and neurological dysfunction. Over the years, that search has expanded beyond traditional boundaries. Once thought to begin at the optic nerve and move backward to the brain, neuro-ophthalmology is now understood as part of a broader, integrated system that starts in the retina and encompasses the entire eye-brain axis as a bidirectional neuro-retinal continuum. This paradigm shift is not just academic; it is transforming how we diagnose, monitor, and ultimately treat some of the most devastating neurodegenerative diseases of our time.
Window to the brain
For centuries, physicians have referred to the eye as a “window into the brain.” Today, advances in imaging technology are opening that window wider and allowing us to see more clearly than ever before. At Thomas Jefferson University's Annesley EyeBrain Center, our work is focused on leveraging this connection to better understand and manage conditions such as Parkinson’s disease, Alzheimer’s disease, multiple sclerosis, and stroke.
Historically, the dogma was that a pale optic nerve indicated atrophy from a process that began in the nerve or brain. Clinical experience and emerging evidence, however, have shown that many disease processes begin in the retina, or else leave subtle clues there long before they manifest in other locations. Patients often arrive at my clinic after exhaustive evaluations elsewhere, with normal fundoscopic exams and inconclusive optical coherence tomography (OCT), often due to lower-resolution devices or a lack of attention to the outer retina. As neuro-ophthalmologists, we are often the referral destination for complex or unresolved patient cases, and it is our responsibility to look deeper.
Beyond structure: functional imaging with FLIO
Traditional imaging modalities - such as fundus photography, OCT, and even high-resolution magnetic resonance imaging (MRI) - have provided invaluable structural information. But structure alone is not enough. In radiology, for example, the leap from computerized tomography (CT) and MRI to positron emission tomography scanning represented a shift from anatomy to function. In ophthalmology, we are now making a similar leap with fluorescence lifetime imaging ophthalmoscopy (FLIO).*
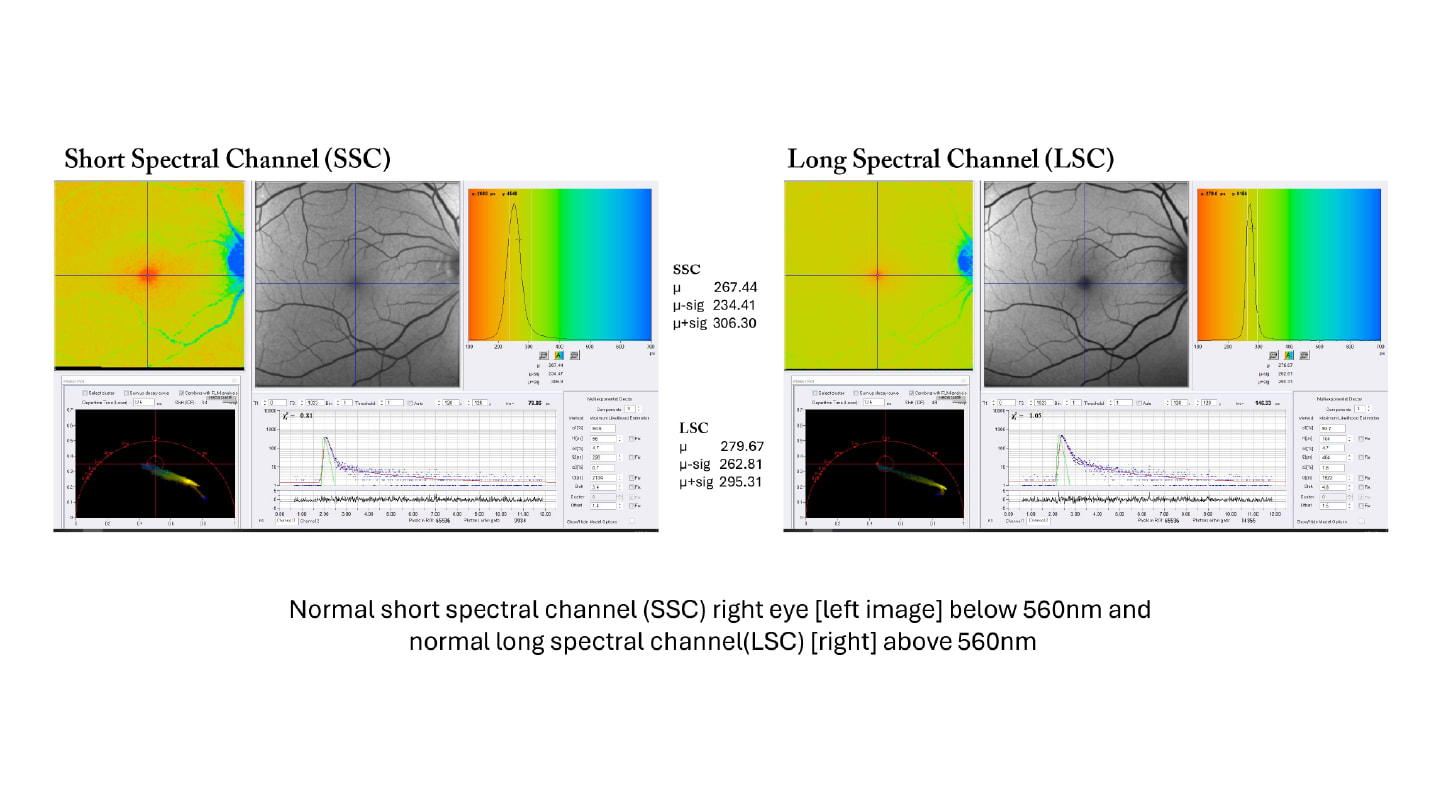
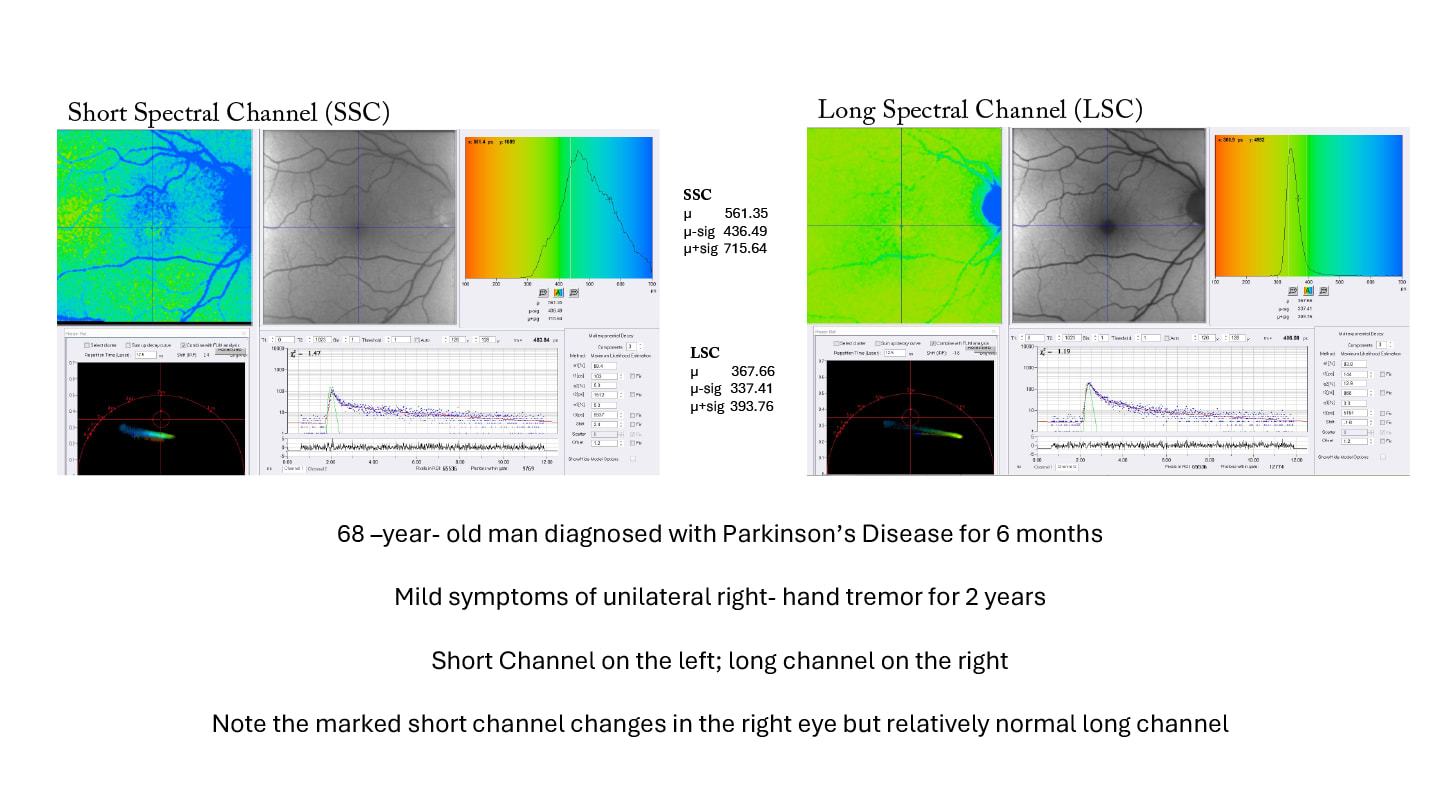
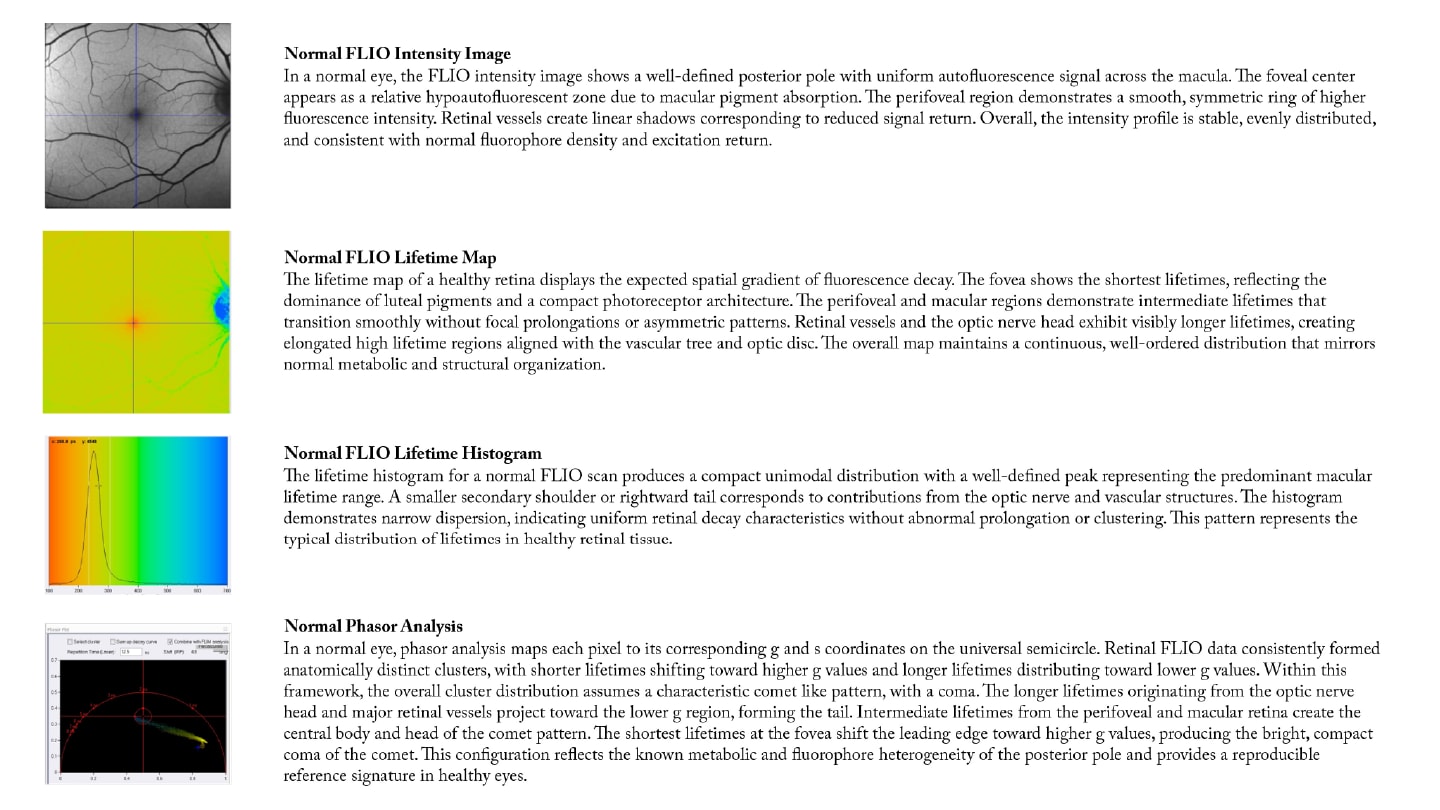
FLIO, developed on the basis of the SPECTRALIS platform by Heidelberg Engineering, allows us to move beyond structural imaging and begin to interrogate retinal function at the molecular level. FLIO measures the decay time of naturally occurring retinal fluorophores, providing a functional “fingerprint” of retinal metabolism. This is particularly relevant in neurodegenerative diseases, where early metabolic changes may precede structural loss.
Our work with FLIO is complemented by high-resolution OCT and advanced MRI, creating a multimodal approach that links retinal findings with brain pathology. This convergence is not unique to our center. Colleagues such as Paul Bernstein and Lydia Sauer at the University of Utah's John A. Moran Eye Center, Christine Curcio at the University of Alabama in Birmingham, Chantal Dysli, Sebastian Wolf, and Martin Zinkernagel in Bern, Switzerland, and Martin Hammer in Jena, Germany, are also advancing the field. The collective goal is to make the invisible visible, empowering clinicians to detect disease earlier, monitor progression more precisely, and ultimately guide therapy.

Translational research: From patient to lab and back again
One of the most exciting developments in our field is the integration of clinical imaging with basic science. Through collaboration with experts like mitochondrial biologists Gyorgy Hajnoczky and Raphael Rubin at Thomas Jefferson University, we are merging FLIO data with findings from electron microscopy and fluorescent lifetime imaging microscopy (FLIM). FLIM, the precursor to FLIO, has long been used to study mitochondrial function in vitro. Now, we are bringing these insights to the clinic.
A particularly promising avenue is the use of induced pluripotent stem cells (iPSCs). By isolating stem cells from a patient’s blood or urine, we are reprogramming these cells into retinal and brain organoids in Professor Hajnoczky’s laboratory, led by Julius Roenkke, his post-doctoral fellow from the University of Helsinki. These organoids will then be studied with FLIM and correlated with in vivo FLIO and OCT findings. This “bidirectional research”, moving from patient to lab and back, holds the promise of personalized medicine. We can identify molecular pathways of disease in a patient’s own cells, test potential therapies, and then translate those findings back to the clinic.
As we move toward clinical application, regulatory agencies such as the FDA, EMA, and others are increasingly demanding objective, quantifiable endpoints for clinical trials. Our HighRes OCT investigational device and FLIO, both from Heidelberg Engineering, provide precisely this: non-invasive, reproducible biomarkers that can track disease progression and therapeutic response. The accessibility of the eye makes it an ideal site for such measurements, offering a unique advantage over other organ systems. While FLIO is still a research device, the data we are generating is laying the groundwork for future clinical trials and, ultimately, new therapies.
The molecular frontier
Mitochondrial dysfunction is the heart of many neurodegenerative diseases. Mitochondria, the energy factories of the cell, are intimately involved in processes ranging from Parkinson and Alzheimer diseases to amyotrophic lateral sclerosis and Charcot-Marie-Tooth. FLIO provides a window into mitochondrial health in vivo, while FLIM and electron microscopy allow us to study these organelles in unprecedented detail. Recent discoveries have shown that mitochondria are not static cylinders but dynamic networks that branch, tunnel, and communicate with neurons and other mitochondria. Understanding these interactions at the molecular level is key to unraveling the pathogenesis of neurodegeneration and developing targeted therapies.
Collaboration in action
Progress in medicine has always been tied to advances in imaging and technology. From X-rays and CT scans to MRI and now FLIO, each leap has also required collaboration between clinicians, scientists, industry, and, crucially, patients and donors. Working closely with regulatory agencies and industry partners ensures that our research is both scientifically rigorous and clinically relevant.
As neuro-ophthalmologists, we must recognize that the status quo no longer meets the needs of our patients. Too often, our role has been limited to diagnosis and referral. With the advent of advanced imaging and translational research, we have the tools to be more active participants in clinical trials and therapeutic development. It is time to redefine our subspecialty — not just as diagnosticians, but as innovators and leaders in the fight against neurodegenerative disease.
I encourage my colleagues to embrace this new era. We need to attend interdisciplinary meetings, collaborate with basic scientists, and engage with industry partners who share our commitment to excellence. The future of neuro-ophthalmology lies in the convergence of technologies, disciplines, and ideas.
We stand at the threshold of a new era in neuro-ophthalmology. By integrating advanced imaging, molecular biology, and translational research, we are making the invisible visible, and bringing hope to patients with previously untreatable diseases. Let us not be content with the status quo. Together, we can redefine what is possible for our patients and our profession.
* FLIO is an investigational device in the US and not currently available for commercial or clinical use.
