
Making the Subjective Objective
So much of premium IOL selection comes down to chair time and questionnaires. But what if it didn’t?
At a Glance
- When selecting or recommending an IOL to a patient, surgeons try to get to know the patient through chair time and questionnaires
- Subjective assessments are not the best approach because patients can forget or misrepresent their visual requirements
- Truly and objectively assessing how patients use their vision day-to-day would allow surgeons to select the best IOL for their needs
- I overview the Visual Behavior Monitor, and how it can make the subjective objective
Woe betide the surgeon with an unhappy patient – especially if that patient has spent a hefty sum of money on elective surgery to get there. Cataract and refractive surgeons describe such patients not as just ruining their day, but ruining their whole month.
One big challenge in refractive surgery is understanding what the patient wants – and then selecting the best course of action to meet that objective. Determining the correct target refraction (see Box 1) is critical, but there’s more to it than that. For example, certain multifocal IOLs perform better in patients with small pupils and mesopic conditions than others; both toric multifocal and small-aperture optic IOLs can correct presbyopia and some amount of astigmatism. The problem is that no simple nomogram exists that can lead a surgeon to the best choice for the patient. It’s why these surgeons spend a considerable amount of time discussing their patients’ lifestyles – hobbies, work, whether they read the news on a newspaper or a phone screen, and even what time of day they drive – all to try to determine which option might be best for their patient. And that’s before they start to make a call on a patient’s personality type…
Box 1. Current methods of determining target refraction
Cataract Surgery
- Axial length (ocular biometry)
- Corneal refractive power (keratometry)
- IOL lens position prediction (regression formula)
- Subjective evaluated self-reported target refraction
Refractive surgery
- Subjective refraction
- Nomograms
- Subjective evaluated self-reported target refraction
The problem is that most of the methods listed above are inherently imprecise, which leads to deviation from the intended target refraction.
But there’s a clear problem: it’s all subjective. A patient might say they do no close work, but then complain that they used to enjoy doing crossword puzzles or building 1:200 model airplanes after the surgery. They can be forgetful. They can be distracted. They might just be having a bad day when they are in the chair. Even if the surgeon knows the defocus curves of all IOLs on the market as well as the predicted refractive effects of all the surgical interventions at their disposal – and be experienced with them all – there’s still a lot of guesswork. Surgeons are acutely aware of this and often decide to “play it safe” by offering a monofocal IOL rather than a premium lens. Why risk having a disgruntled patient and the financial and reputational risks they bring? On the flipside, many patients who could benefit from a premium lens or other refractive procedure do not, which is a missed opportunity for surgeon and patient alike. Wouldn’t it be nice to remove the subjective element from the process?
Smart objectivity
When you use a smartphone, you’ll notice that the screen dims when you hold the device to your ear to make a call. Why? An infrared proximity sensor. If you open your phone’s built-in health app, you’ll find that it has measured the number of steps you’ve taken that day. How has your phone become a pedometer? Your phone contains an accelerometer, gyroscope and magnetometer – it knows its orientation in all three dimensions at all times, and can detect the characteristic movement of each step. Finally, most smartphones can adjust their screen brightness to a level that’s appropriate for the ambient lighting conditions – it dims in dark environments, and gets brighter when the surrounding area is well-lit. But the combination of proximity, orientation, movement and ambient light sensors can be used to achieve something else – something that helps bring some objective metrics to the premium cataract surgeon’s subjective dilemma.

Figure 1. The Visual Behavior Monitor (Vivior AG, Zürich, Switzerland); a small device with distance, ambient light and orientation and motion sensors that clips onto a pair of spectacles.

Figure 2. Illustration of a typical office working distance distribution map generated by the Visual Behavior Monitor.
It turns out that if you combine those three sensors on a small device that clips to a prospective patient’s spectacles (Figure 1 – Vivior’s Visual Behavior Monitor), you can mine the data that’s recorded – and that includes the distance, duration, ambient lighting conditions, and even the angle of the patient’s head – while the patient interacts with objects, people or performs tasks throughout their day (Figure 2; (1)(2)(3)).
The patient’s activities can be determined automatically through machine learning algorithms and this gives the surgeon the necessary information about the patient’s lifestyle. Crucially, such a device provides objective information on the patient’s lifestyle and visual needs that help the surgeon to choose the best treatment solutions (Figure 3). The objective device supersedes the subjective questionnaires and chair time.
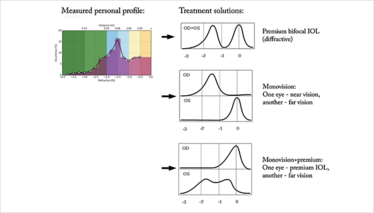
Figure 3. How the Visual Behavior Monitor data can be used to suggest treatment options for the patient based on their own activities.
A great deal of that chair time in cataract/refractive surgery involves patient education, because the decision on which surgical approach and product to use is a joint one. And so, devices like Vivor’s Visual Behavior Monitor should also prove useful in helping patients understand their daily vision needs – and, in doing so, increase their awareness and understanding of appropriate treatment options. Ultimately (or hopefully), patients will have more realistic expectations of what their personalized vision solution can achieve.
The move from subjective measures to objective metrics goes beyond aiding the selection of the optimal refractive solution based on patients’ needs – it could also help mitigate the legal risks involved with missed refractions and disgruntled patients.
Finally, the automated collection of objective data could feed into big data; the more data that’s collected, the more refined the automated predictions of activity become – and the more confident the surgeon can be with the predictions made by the system. If such automated solutions can expand the number of patients who can successfully undergo premium cataract/refractive surgery – and be happy with the outcome – it’s a win for everyone; the surgeon, the practice, the product manufacturers and, of course, the spectacle-free patient.
- A Cummings et al., “Patient Refractive Needs Assessed with Objective Measurements”, Presentation at the American Society of Cataract and Refractive Surgery (ASCRS), May 2017. Available at: bit.ly/vbmarthur.
- M Mrochen, et al., “Objective evaluation of patients’ visual behavioural pattern for cataract surgery planning”, Presentation at the European Society of Cataract & Refractive Surgeons (ESCRS) October 2017. Available at: bit.ly/vbmmich.
- M Mrochen et al., “Planning the individual refractive correction for cataract patients based on objectively measured refraction profile”, Presentation at the European Society of Cataract & Refractive Surgeons (ESCRS) October 2017. Available at: bit.ly/vmbtop.
I spent seven years as a medical writer, writing primary and review manuscripts, congress presentations and marketing materials for numerous – and mostly German – pharmaceutical companies. Prior to my adventures in medical communications, I was a Wellcome Trust PhD student at the University of Edinburgh.













