Contemporary LASIK is not a single-system procedure. It incorporates three separate technologies – an excimer laser, a femtosecond laser and a wavefront aberrometer – all of which have undergone many innovations over the past 20 years. Explaining to patients how these advanced technologies combine to provide excellent results can be a challenge.
While all excimer lasers deliver very precise 193-nm laser pulses, the pulse delivery algorithms and the sophistication of the aberrometry systems that measure the eye and inform the laser are a major component of how we differentiate our results today. Another significant factor is the way in which the flap is designed. I coined the term EAGLE Vision to more intuitively convey to my patients what the iLASIK Technology Suite (Johnson & Johnson Vision), can now deliver for patients. EAGLE Vision stands for Elliptical-flap, Aberrometry-Guided, Laser-Enhanced Vision.
Measurement innovations
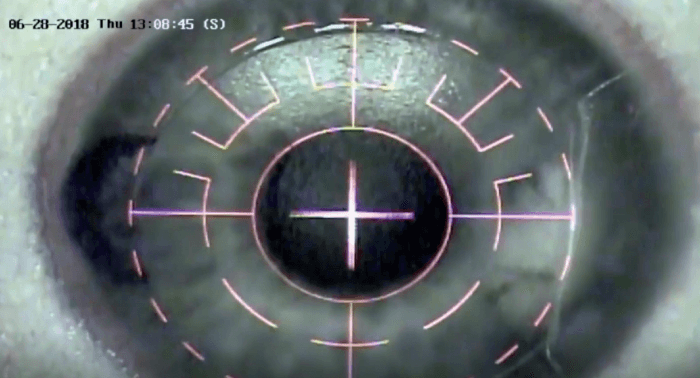
We now have the ability to measure the entire ocular micro-zonal refraction with exquisite detail and accuracy, to inform the eximer laser and precisely guide the laser pulse delivery onto a predetermined stromal grid. The wavefront sensor within the iDesign Refractive Studio, has a fivefold greater number of lenslets than its predecessor (the WaveScan) did, capturing more than 1,200 spots over a 7.0-mm pupil. When talking to patients about this improvement, I use the analogy of a high-definition television with more pixels on the same screen. They understand how that improves the image the device is capturing of their eye and translates that level of precision onto their cornea.
In addition to wavefront aberrometry, the iDesign also integrates five other simultaneous measurements, including full-gradient topography, autorefraction, keratometry, corneal diameter and pupillometry. Because all of these are captured on the same fixation axis, they are spatially registered to one another. The addition of topography data in particular helps to reconstruct an exact mathematical representation of the corneal surface. The additional measurements also enable me to further refine the flap shape and diameter customization (see Flap innovations below).
With this device, we can measure scotopic pupils as small as 4.0 mm, and our treatment indications have been expanded to include wavefront-guided PRK, monovision treatments, and a broader range of astigmatism correction than before. I also explain to patients that as the diagnostic elements of the treatment have improved, we are not only able to improve the ablation pattern but to more consistently rule out patients who have a higher risk of ectasia and should not have Lasik and may instead benefit from PRK, collagen cross linking, or observation. Better measurement means better selection, better treatment and better results.
Flap innovations
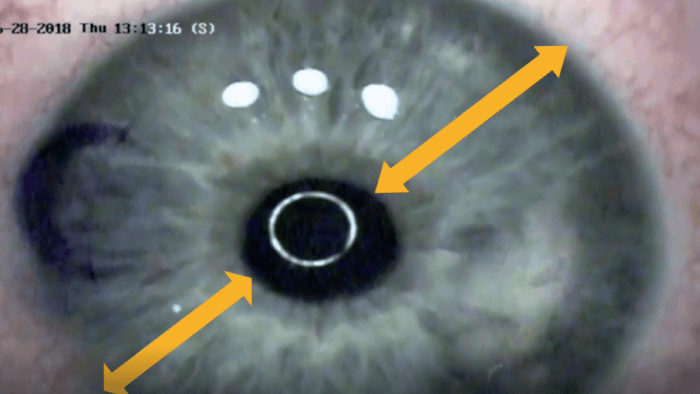
Coupled with the gains in treatment planning, I also consider it very important that this platform allows us to customize flap parameters – including hinge location/width, and flap diameter, shape and thickness – further aiding in achieving optimal outcomes. Because the temporal corneal quadrant is by far the most expansive, it enables many ensuing flap design changes (1). Here are the changes in flap architecture I have worked with over the years and believe to have made a big difference in my personal outcomes:
1. Temporal hinged, elliptical shape
Elliptical flaps, first developed in collaboration with IntraLase, are 4 to 10 percent longer in the horizontal than the vertical axis, honoring the inherent corneal shape. Elliptical shaped flaps can easily be accommodated by rotating the hinge to the most expansive (temporal) corneal quadrant. Because the pupil is always superonasal, a temporal quadrant-based hinge positions the hinge as far from the pupil center as possible. This spacing ensures a large exposed surface area so that the flap hinge does not interfere with the large-diameter optical zone ablation patterns required for wavefront-guided, topography-refined treatments.
In addition to better visual acuity outcomes, we have also observed fewer complaints of early postoperative dysphotopsias since developing these flap patterns. The elliptical flap, coupled with a temporal hinge, also keeps any opaque bubble layer (OBL) farther away from the pupil, preserves more of the temporal long ciliary nerves (especially when the “pocket” is also deleted), and provides for greater protection in collaboration with the facial bones – since the temporal quadrant is the only one without a surrounding bony prominence – in the unlikely event of perioperative blunt trauma.
2. Wide hinge
With the temporal hinge adoption, I have also gone from a 45° hinge angle to a much wider 65°-70° angle, which I believe diminishes dry eye (by preserving more of the ciliary nerve fibers) and also leads to a more tectonically stable flap. My personal experience has been that a more broadly anchored – widely-hinged – flap reduces the incidence of epithelial ingrowth, microstriae and slipped flaps, as it more securely fits back onto the bed with less misalignment that could result in early flap striae. Subtle misalignment could also compromise the benefits of the highly refined ablation pattern.
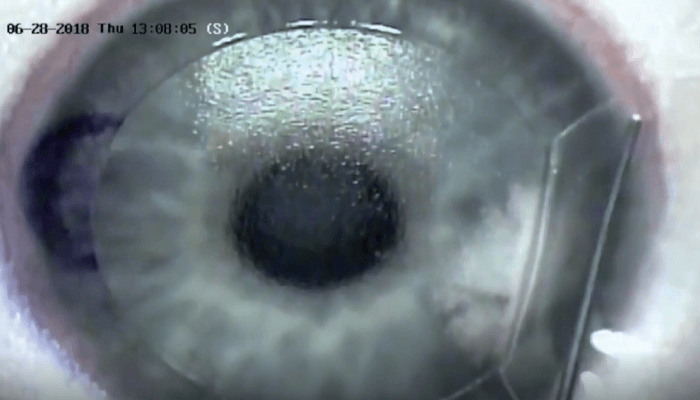
In adopting such an approach, the flap in many cases doesn’t even need to be fully reflected to the hinge margin in order to deliver the entire ablation to the exposed stromal bed (due to its horizontal elongation). In such cases, the effective hinge angle becomes even wider than 70°. In our experience, these much wider-hinged flaps have also diminished our observed incidence of dry eye, both subjective (patient-related experience) and objective (reduced epithelial superficial punctate staining or SPK).
3. Thinner flaps
Because there is less risk of flap slippage with a wide hinge, surgeons can also feel more comfortable making thinner femtosecond laser flaps. I routinely make a 95- to 100-µm flap, and believe that in time, with ever more refinement of femtosecond lasers, we may even challenge the widely held view that 95 µm is the thinnest desirable flap limit. Thin flaps, if devoid of microstriae, may augment the visual benefits accompanying highly refined ablation patterns, whereas a thick flap can dampen the surface transmission of the exquisitely precise sculpting profile. A thin flap also ensures a thicker residual stromal bed, preserving corneal tectonic stability, reducing ectasia risk and increasing the likelihood of future enhancement candidacy.
Headed in the right direction
Better measurement capabilities and greater flap customization have combined to improve our patient experience. Increasingly, we are seeing patients achieve vision that is close to their true retinal potential. For example, I recently received a message from a Wimbledon champion/patient, exclaiming that his son (also a patient and a rising athlete), was tested at the National Health Center in Holland and observed to now have uncorrected acuity of 20/10 OD, 20/8 OS and 20/8 binocularly following his recent LASIK procedure. Not every patient will achieve 20/8 – or appreciate the titratable impact of vision on performance the way professional athletes do – but cases like this one highlight that we are finally delivering on a promise that for many years was aspirational.
Multiple studies have now shown that custom, wavefront-guided LASIK can frequently achieve even better uncorrected visual acuity after surgery than the best pair of glasses. In my practice, nearly 50 percent of patients are achieving uncorrected acuity after surgery that is better than their best corrected visual acuity before surgery.
The entire industry may be starting to move in this direction. While the iDesign is still the only system with individualized wavefront analysis and data further refined by corneal surface topography, there are now other systems that inform the laser beyond simple refraction. While these others are primarily using corneal surface topography, some are adding limited population-averaged spherical aberration refinement. The trend for “smarter” lasers looks set to continue.
We also have new procedures such as small-incision lenticule extraction (SMILE). I’m optimistic about SMILE’s potential, especially once the lenticules can be made thinner, more superficial and with shaping patterns for correcting all forms of refractive error – not just myopic astigmatism.
I am encouraged that corneal refractive surgery continues to evolve in new and exciting ways that increase the precision and sophistication of what we can offer patients. When new technologies come along, we are tempted to judge our results by our successes. Experienced surgeons, however, learn to judge their results based upon their failures. At present, LASIK as I’ve described it here is the only way to reliably reach the goal to which I aspire for my patients – not just to throw away their glasses and experience fast visual recovery, but to see significantly better following surgery than they could prior.
For more information click here Kerry Assil
References
- K Assil and T McCall, “Temporal hinge laser in situ keratomileusis: Maximizing treatable stromal bed area”, J Cataract Refract Surg, 31, 1139-44 (2005). PMID: 16039487.
