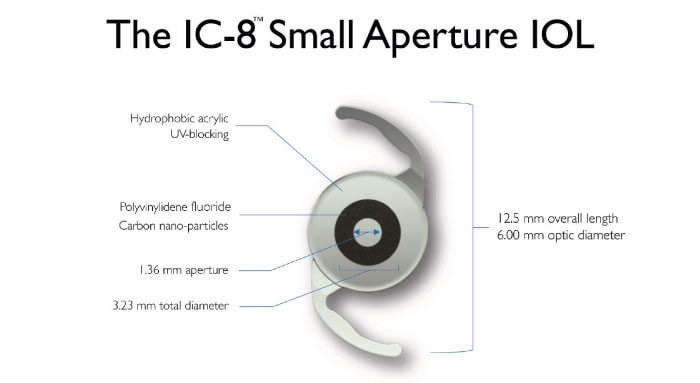
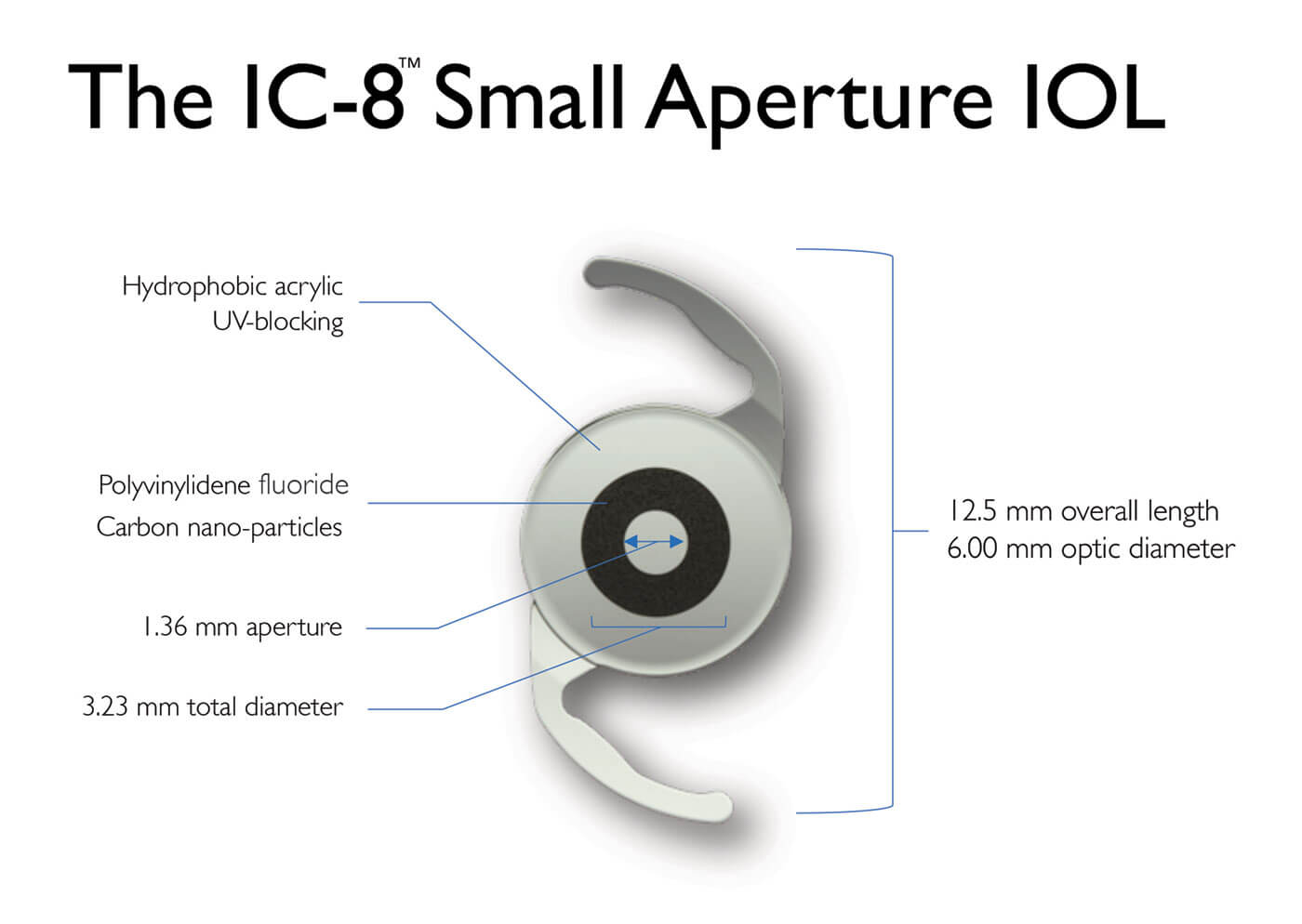
The AcuFocus IC-8 intraocular lens extends depth of focus by combining small aperture technology with a monofocal lens. This innovative design – incorporating an opaque mini ring with a central aperture – provides cataract patients with excellent quality of vision over a broad range of distances.
Expert panel of ophthalmic surgeons
• Boon Ham (Australia): General/pediatric ophthalmologist with interest in cataract/glaucoma surgery. He began implanting the IC-8 IOL in 2016.
• Brendan Vote (Australia): General ophthalmologist with interests in cataract and retina; performs 750-1,000 cataract procedures per year. Has implanted the IC-8 IOL in ~80 patients since 2016.
• Christopher Chan (Australia): General/refractive ophthalmologist treating primarily glaucoma, AMD, DR, dry eye and cataracts. Has implanted the IC-8 IOL in over 100 cataract patients including those presenting with irregular astigmatism, and significant nocturnal glare. He has also evaluated use of the IC-8 IOL in combination with other EDOF lenses – Symfony/Symfony toric.
• Gerd Auffarth (Germany): Treats a complete spectrum of eye diseases; since 2015, has implanted the IC-8 IOL in a broad range of patients including cataract, refractive lens exchange, compromised corneas, and traumatic iris defects. He has also implanted the IC-8 lens in combination with the Oculentis MF 20 lens.
• Jacqueline Beltz (Australia): Focuses on cornea, cataract, and refractive patients; recently completed a comparison of the IC-8 IOL versus moderate monovision with monofocal IOLs in 40 patients.
• Michael Shiu (Australia): Mainly treats cataract, glaucoma, and lens exchange patients; some AMD. Has implanted ~70 IC-8 IOLs, including bilateral IC-8 IOL implantation in irregular cornea patients, since 2018.
• Sathish Srinivasan (UK): Primarily treats cornea, cataract, and refractive patients. Has implanted ~50 IC-8 IOLs since 2016, including in post-laser vision correction patients, postkeratotomy patients, refractive lens exchange and cataract patients.
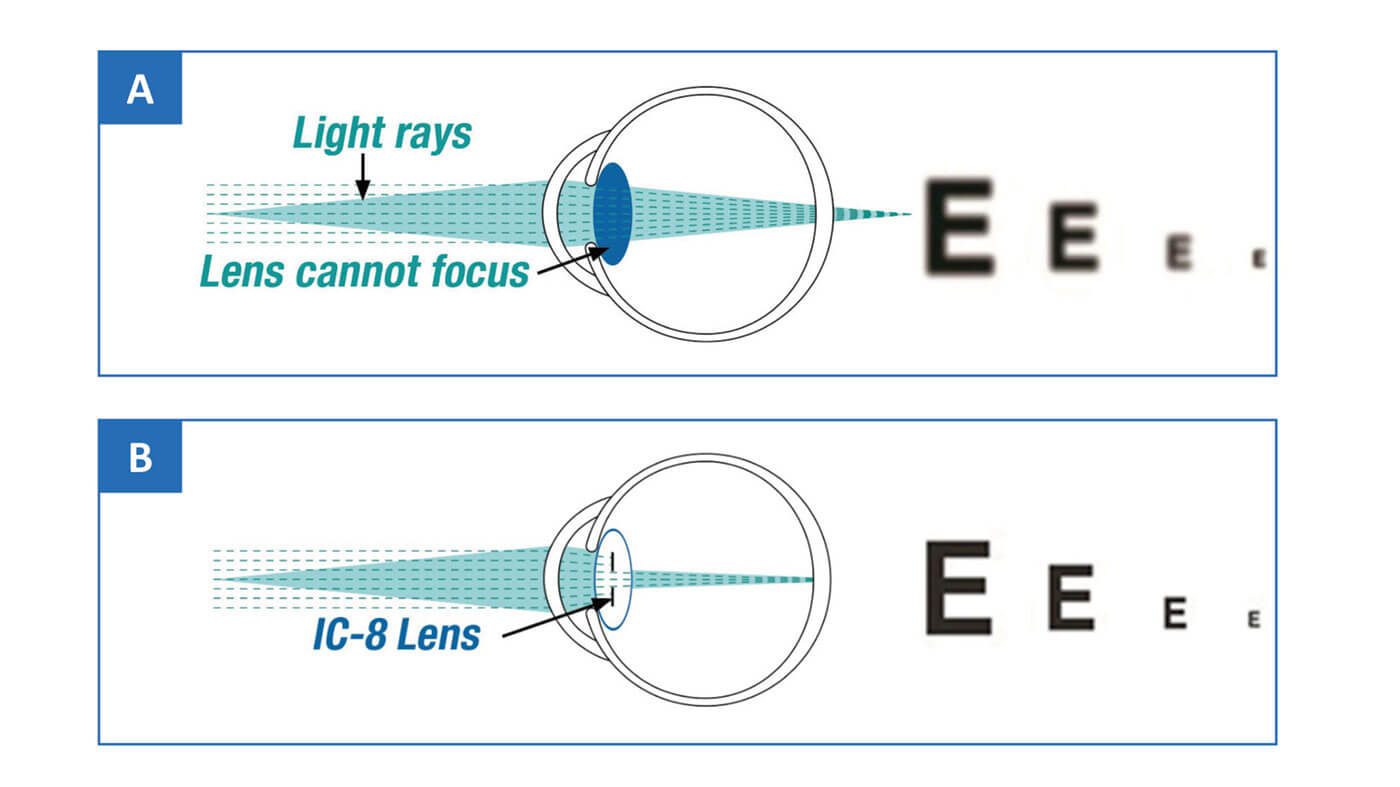
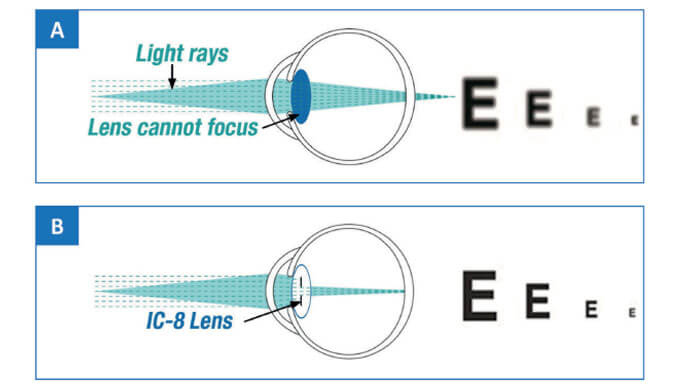
The IC-8 one-piece hydrophobic acrylic IOL is designed to compensate for the focal consequences of peripheral defocused light, thereby enabling correction of presbyopia with a broad, continuous range of focus (Figure 1). We asked a panel of surgeons (see sidebar) to share their knowledge and experience of the IC-8 IOL.
Extended range of benefits
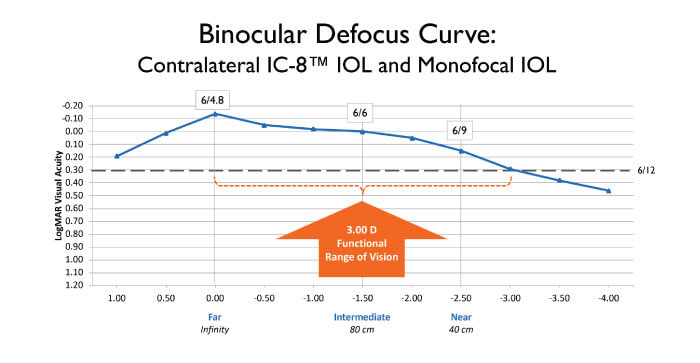
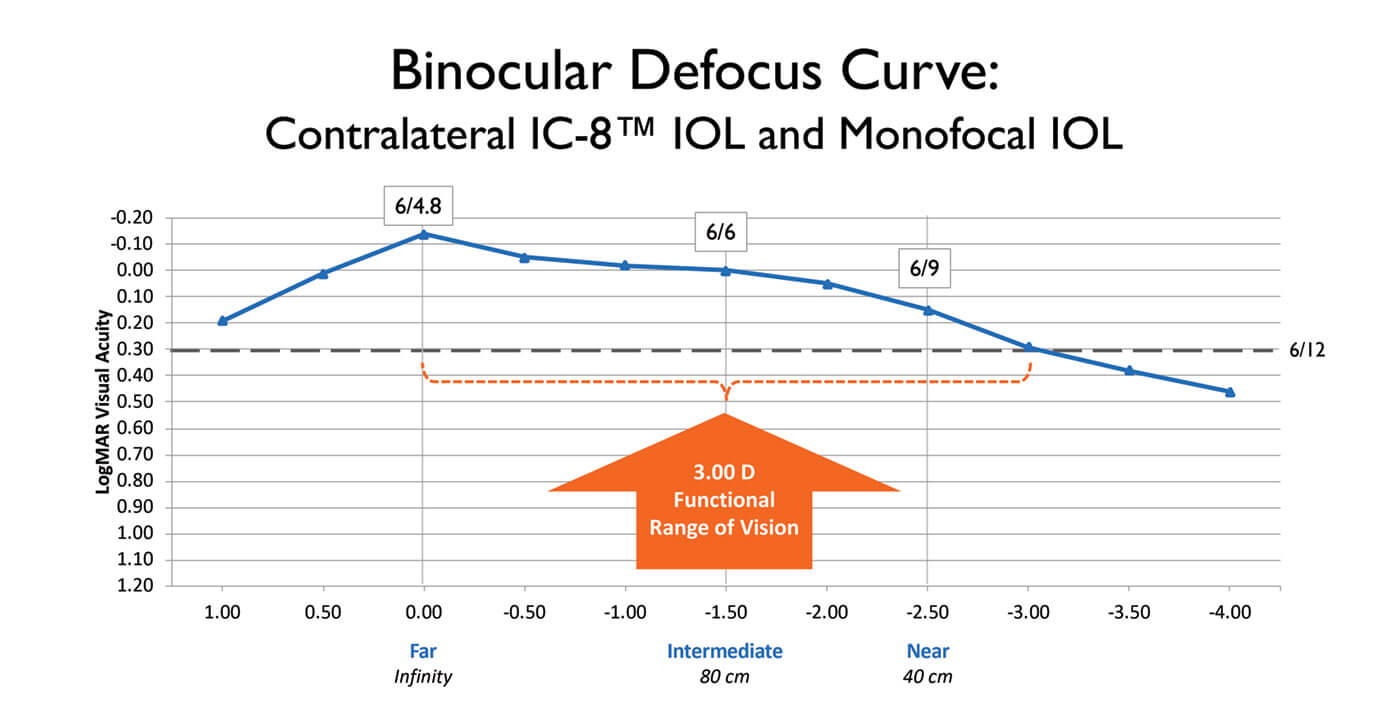
The design of the IC-8 IOL enables it to provide 3.00 D of extended depth of focus (EDOF), tolerate up to 1.00 D deviation from the target manifest refraction spherical equivalent, and accommodate as much as 1.50 D of corneal astigmatism (1-4). In addition, this unique IOL can reduce the effects of both lower and higher order aberrations (HOA), including corneal HOAs such as coma, based on the small aperture effect. How does the IC-8 IOL provide this range of benefits?
The fundamental feature of the IC-8 lens, as Christopher Chan points out, is the opaque annular mask, which blocks scattered, defocused and aberrated peripheral light, but allows the passage of paraxial, central light rays (Figure 2). Chan says, “This flattens the defocus curve on the myopic/hyperopic side, resulting
in EDOF.” Gerd Auffarth elaborates: “Essentially, the IC-8 IOL uses the pinhole effect to exclude peripheral defocused light – which compromises image quality – and permits only central, focused light to reach the retina.”
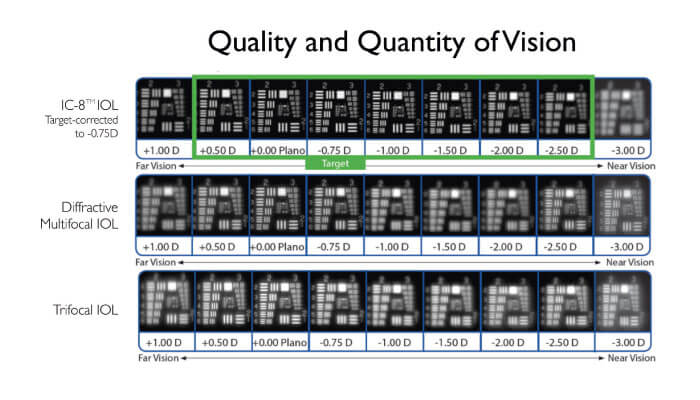
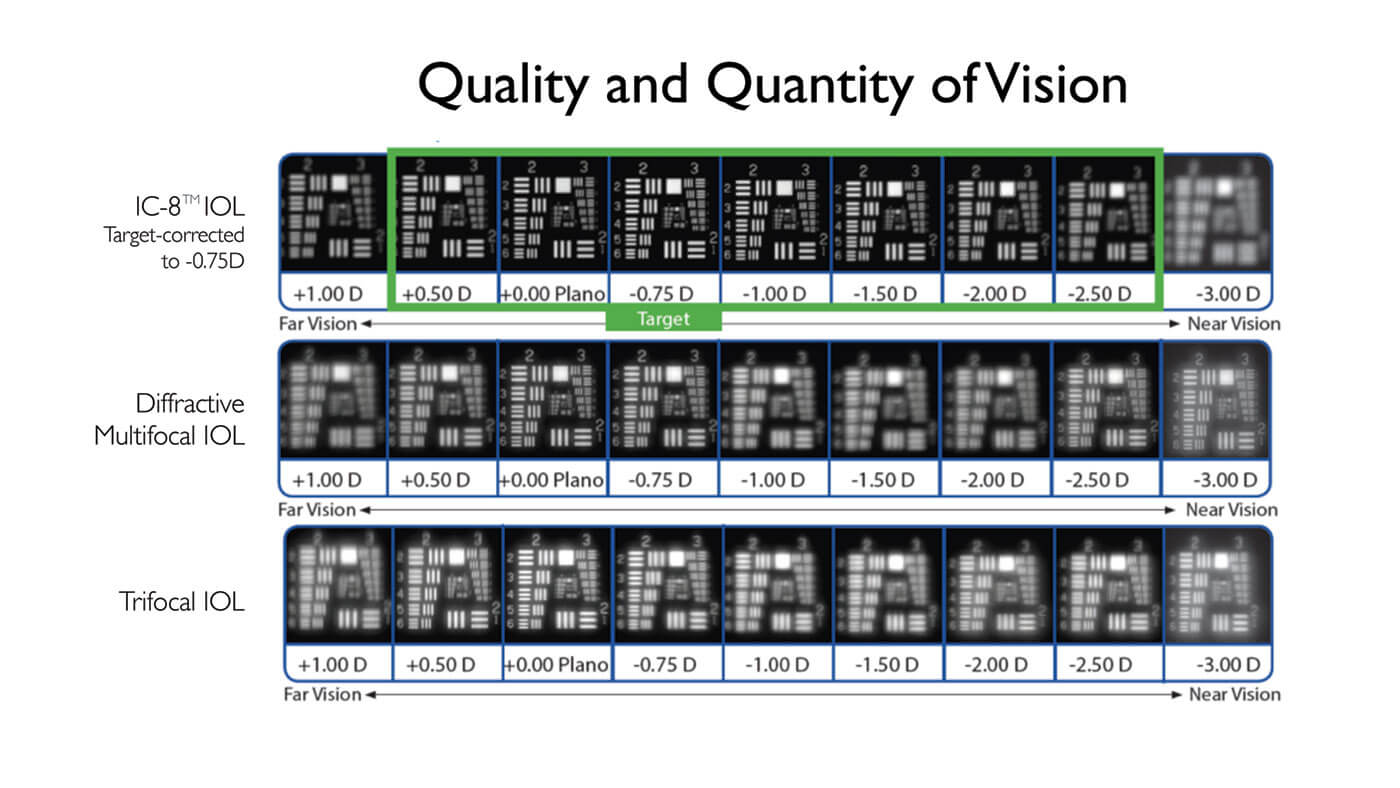
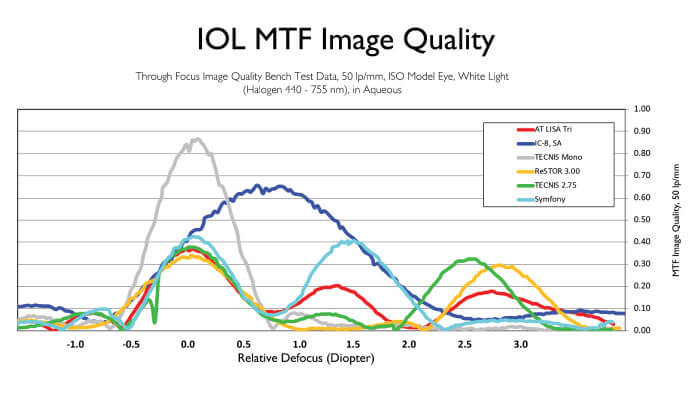
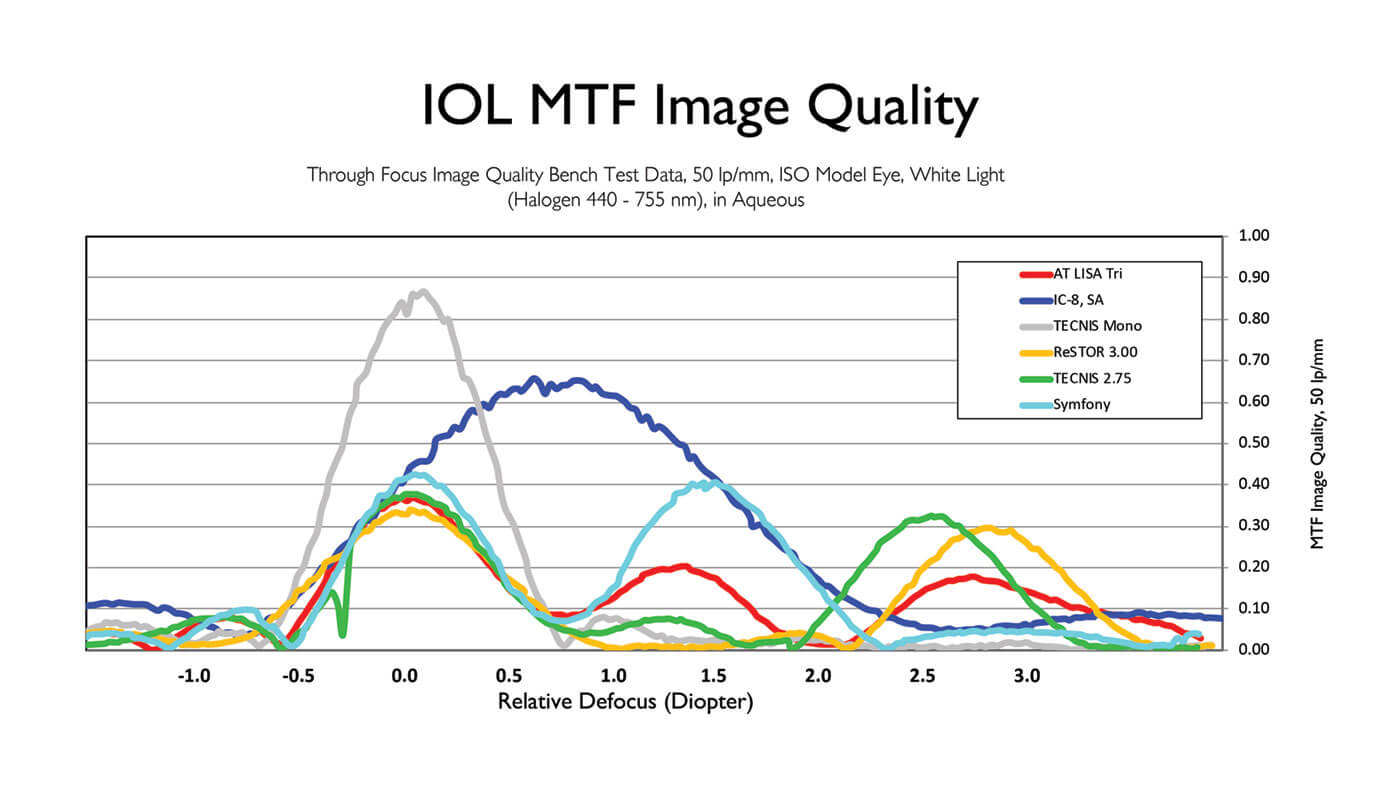
Brendan Vote provides some detail: “The small (1.36 mm) non-diffractive aperture of the IC-8 lens, together with the absence of diffractive surface structures in the IOL, allows it to act as a ‘universal’ corrective lens. Furthermore, the optimized size of the mask provides both excellent quality of vision and a modulation transfer function superior to that of other multifocal or EDOF lenses” (Figure 3).
Jacqueline Beltz reminds us of a practical benefit: namely, that the IC-8 IOL can compensate for up to 1.50 D of astigmatism without needing to be placed on a particular axis. “Hence, this IOL has a larger ‘sweet spot’, making it easier to use and to achieve patient satisfaction,” she says (Figure 4).
Vote elaborates: “The 1.50 D value is significant, because this level of astigmatism is commonly introduced by biometric errors, arising from dry eyes
and tear film irregularity.”
Overall, Auffarth summarizes that the IC-8 IOL’s pinhole effect blocks peripheral defocused light which may actually block glare in some situations. These features, says Chan, explain why, in his experience, the IC-8 IOL has lower dysphotopsia rates than multifocal IOLs but exhibits no significant reduction in binocular contrast sensitivity. Vote concludes: “Compared with monovision patients, IC-8 IOL recipients have good binocular distance vision as well as good intermediate and near vision.”
Extended range of patients
The IC-8 IOL uses a unique method of action, small aperture optics, to correct vision for cataract patients. In general, the IC-8 IOL may be applied to cataract patients with up to 1.50 D pre-existing corneal astigmatism. Typically, it is used in combination with a small amount of monovision (-0.75 D): implanting the IC-8 lens in one eye preserves distance vision binocularity while achieving good near and intermediate vision – with less ametropia than required by monofocal monovision.
What kinds of patients are recommended an IC-8 lens by our expert panel?
Michael Shiu considers any patients suitable for a standard cataract operation to be a potential IC-8 IOL candidate, particularly if they want spectacle independence. “Age is not a limiting factor,” he says. Shiu also notes the benefits of an IC-8 IOL in young patients with traumatic cataract formation: “In these cases, monofocal IOLs are not appropriate, because the patients still need near vision. For these patients, I choose the IC-8 lens, even if their pupils are a bit larger than recommended for this IOL.” Outcomes, he says, are good; he has had no complaints of glare. Shiu adds: “One of them even achieved good vision with imperfect centration – I was very, very impressed!”
Beltz prefers to use the IC-8 IOL in combination with monovision: “Generally, I like to target between -0.75 and -1.00 D of myopia with the IC-8 IOL in the nondominant eye, whilst targeting emmetropia with a monofocal in the dominant eye.”
Any other points? Sathish Srinivasan shared: “I have found for patients where power calculation is a problem, the small aperture IC-8 lens is quite forgiving – even when the refractive outcome is not perfect, the patient will have good distance, intermediate and near vision.” Vote notes that patients with HOA >0.3 and especially those with >0.5, who are not suitable for standard multifocal IOLs, are likely to benefit from the improved optics from the IC-8 IOL’s small aperture design. Auffarth agrees: “The IC-8 IOL is an important alternative to diffractive IOLs, as it is not associated with halo or glare issues in my experience.” Beltz notes that the IC-8 lens allows treatment of presbyopia in patients unsuitable for trifocal IOLs or unable to tolerate anisometropia or monovision. Shiu agrees: “If patients need very clear near vision, trifocals are good, but if they don’t want glare or halos the IC-8 IOL may be better – it depends on the patient’s requirements.” In summary, Chan states that the IC-8 lens gives him the option of offering spectacle independence to patients who are not candidates for other presbyopiacorrecting lens technology and would otherwise be limited to a monofocal IOL.
But there must be patients unsuited for the IC-8 IOL – what factors do our experts consider? Vote is clear: “Avoid eyes with central corneal scarring that overlaps the center aperture.” He also notes that he typically excludes patients with mesopic pupil sizes >6 mm as they are more likely to experience dysphotopsias, especially glare. Similarly, Shiu counsels avoiding eyes with with mesopic pupils larger than 5 mm (again, because the patients will likely experience halos and glare), and patients with macular pathology (because the IC-8 lens’ pinhole effect may reduce contrast too much). “I also avoid patients with severe glaucoma because of their existing issues with restricted visual field and contrast sensitivity,” says Shiu. Chan avoids monocular patients, patients with vitreous opacity, large or eccentric pupils, and those with retinal diseases such as AMD, advanced glaucoma, or significant diabetic retinopathy. Similarly, Auffarth cautions against implanting an IC-8 IOL in patients with very high need for near vision, severe retinal problems, glaucomatous damage, capsular rupture, pseudoexfoliation syndrome, or zonular weakness. Beltz suggests avoiding patients who don’t want to notice a difference between their eyes, and those at high risk of developing ocular diseases such as glaucoma, AMD, or DR.
Extending surgeon expectations
Overall, a small aperture IOL should provide a presbyopia-correcting solution for patients who, until now, had no options in this area, and give them and others an excellent functional range of vision from near to far, without blurred zones (Figure 4). Does the IC-8 IOL meet these expectations?
Beltz reports that her prospective randomized trial of 40 patients – receiving monovision with either bilateral monofocal IOLs or a monofocal IOL in the dominant eye and the IC-8 IOL in the non-dominant eye – showed that the IC-8 IOL group enjoyed similar near and intermediate visual outcomes but superior distance vision. She adds: “High overall satisfaction and a low symptom rate was expressed in both groups.” Similarly, Boon Ham notes that most or all of his patients attained good vision for both distance and near, and Vote states that patients typically show high quality of vision across a much greater depth of focus, with few night vision problems. Indeed, Vote can express his satisfaction in numbers: “My initial outcomes were part of a published series of 126 patients (5). In patients without ocular comorbidity, 98 percent achieved a UDVA of 6/9, 94 percent a UIVA of 6/12 and 91 percent a UNVA of 6/12. Patients reported good satisfaction with near vision (8.1/10) and distance vision (9.1/10)” (5).
Chan also can quantify outcomes: “My chart review of 42 recipients of the IC-8 lens in combination with a toric IOL showed that 93 percent had binocular UCDVA of 6/6 or better, 86 percent had binocular UCIVA of 6/7.5 or better, and 90 percent had binocular UCNVA of N6 or better.” He adds that he has seen no significant reduction in brightness perception, and only very low levels of nocturnal dysphotopsias such as starburst and halos. “In addition, the IC-8 lens was very forgiving with regard to refractive surprises.” And Auffarth promises us similar numbers in the future: “The MOSAIC study showed that IC-8 lens gives very good near, intermediate and distance acuity – we will publish the data soon.”
Vote sums up the experts’ feelings like this: “It’s an old cliche but a good one - would you use the lens on yourself or a family member? My father (outdoor lifestyle/fishing) and brother-in-law (builder) each had IC-8 IOL implantations, and each enjoyed excellent outcomes, including spectacle independence, suited to their lifestyles.”
Extending post-operative possibilities
Initial outcomes with the IC-8 IOL are clearly good – but what are the longer-term implications of a small aperture IOL? Does it hinder taking refraction, interfere with retinal visualization or impede subsequent retinal surgery? Certainly, some procedures need minor adjustment: Beltz points out that, due to the increased depth of focus, it can be difficult to determine a suitable “end point” while refracting. “The best method to use is termed ‘mid-point refraction’ and involves performing a normal manifest refraction and then establishing the maximum plus lenses to blur and the maximum minus lenses to blur – then you calculate the mid-point.” Beltz notes that it is also acceptable to perform a red/green balance test. Shiu concurs: “We usually use the red and green method to ensure we are not giving patients extra refraction due to the extended range of vision.” Vote states that autorefractors do not perform well in eyes that have been implanted with an IC-8 IOL: “Consequently, refractive outcomes should be assessed subjectively.”
Regarding subsequent surgery, Ham has this comment: “In a dilated pupil, we can view the retina fairly well so I think retinal surgery in an IC-8 IOL eye will be
reasonably straightforward. There may be exceptions depending on the VR surgeon.” – Vote too does not anticipate significant issues: “Modern VR operating systems (such as BIOM) deal very well with small pupils.” Chan reminds us of a UK report (6) indicating that the IC-8 IOL does not impede the intra-operative view during pars plana vitrectomy, and Auffarth notes anecdotal reports from German surgeons that retinal detachment and peeling surgery can be performed in IC-8 IOL eyes. Srinivasan concurs: “There is no issue regarding performance of retinal surgery in IC-8 IOL eyes. I have personally assisted a retina colleague on an IC-8 IOL eye where the surgeon noted the lens did not impede viewing of the posterior segment or his ability to perform pars plana vitrectomy.” Srinivasan also noted: “The advantage the IC-8 IOL has is the center and periphery of the lens is a monofocal optic so the retinal surgeon does not have to constantly change focus of the microscope like when working through refractive and diffractive rings.”
How does one deal with PCO in an IC-8 IOL implanted eye? Vote puts the issue in perspective: “All IOLs designed to give spectacle independence are sensitive to PCO.” He asserts, however, that YAG can be performed through the IC-8 IOL aperture: “Take care not to hit the mask with the laser – you won’t affect quality of vision but you may change the visual appearance of the IOL, with cosmetic consequences.” Alternatively, Vote says, we can go around the outer edge of the mask, gaining access via a U-shaped flap hinged at the bottom: “I find this approach provides more lasting benefits.” Chan agrees: “My personal preference is to perform laser outside the mask, as this allows a better view of the fundus when the pupil is dilated.” Shiu also prefers to apply YAG from outside the periphery; his experience is that this procedure restores patients’ vision very quickly. By contrast, Beltz prefers to apply laser through the central aperture. Srinivasan takes the view that neither technique (through-the-middle versus around-the-edge) is better than the other: “Both are good – which one you use depends on how the capsule falls.”
With regard to performance in dim light conditions, Vote states that although patients may be aware of a difference between the eyes if they cover each eye in turn, the awareness will diminish over time and in any case is insignificant: “In our visual system, the pupil only accounts for one log unit of the total 10-11 log units of light adaptation.” Chan notes that he has had few complaints of patients experiencing difficulty under low light conditions; nevertheless, he warns patients that they may need glasses to read in dim light. He adds: “Research indicates that perceived brightness with the IC-8 IOL is higher than predicted by simple calculation of actual light reaching the retina through the central aperture.”(7) Shiu emphasizes monolateral IC-8 IOL recipients will have enough light in the dominant eye for neuroadaptation to provide good bilateral low-light vision. He also notes the importance of expectation management: “We tell patients they will need reading glasses in some circumstances – and because there are no surprises, we get few complaints.” Auffarth and Srinivasan state that none of their patients has reported significant night vision difficulties; similarly, Beltz reports that her patients have very high satisfaction with vision in dim light: “The mean satisfaction scores for dim light and bright light vision were equivalent.”
Could the IC-8 IOL small central aperture affect the ability to examine the retina? Vote thinks not: “The mask only extends to 3.23 mm in total, and the peripheral IOL remains clear – peripheral retinal details can be seen easily.” He adds that OCT is not typically impacted. Chan agrees: “There is no problem performing OCT or OCT angiography through an IC-8 lens.” He further notes that fundus examination is also little affected by the small aperture, although it is more difficult if the pupil is not dilated. Auffarth agrees: “For the experienced ophthalmologist, retinal examination in IC-8 IOL eyes will not be a big issue.” Beltz is unequivocal: “I have not had any issues with fundoscopy or OCT imaging; no special attachments or variations to technique are required to image the retina with the IC-8 IOL in place.” She goes on to cite Srinivasan’s data from 10 patients (6): “These showed that standard posterior segment investigations including non-mydriatic fundus photography, optical coherence tomography, and automated perimetry could be safely and effectively performed in eyes with small aperture IOLs.” She adds that the data did not indicate differences in quality between images taken from small and standard aperture IOLs. Srinivasan corroborates this: “In IC-8 IOL eyes we can perform all routine retinal examinations including OCT without concern for image quality.”
Warm feelings
In conclusion, our experts appreciate the straightforward technology behind the IC-8 IOL, which reliably provides 3.00 D of EDOF, accommodates 1.50 D corneal astigmatism, and forgives refractive target misses. When implanted monolaterally with a monofocal IOL – the IC-8 IOL preserves distance vision binocularity while achieving good near and intermediate vision. At the same time, the IC-8 IOL avoids typical issues associated with multifocal lens designs while improving vision quality in a range of patients. Cases that benefit from the IC-8 IOL include traditional cataract eyes, patients with a successful history with monovision, eyes with a high risk of a missed refractive target, and those who do not qualify for trifocals. IC-8 IOL recipients typically report high quality vision across a continuous 3.00 D range of focus with no significant issues under dim light conditions. Furthermore, although taking refraction requires use of the mid-point or red/green methods, in all other respects post-surgical management of the IC-8 IOL eye does not significantly differ from eyes with other IOLs: for example, YAG capsulotomies, retinal imaging by OCT, and retinal surgery can all be performed substantially as normal. In summary, the experts report that the IC-8 IOL meets and exceeds their expectations.
References
- Data on file at AcuFocus, Inc.
- H Dick et al., “Prospective multicentre trial of a small-aperture intraocular lens in cataract surgery”, J Cataract Refract Surg, 43, 956 (2017). PMID: 28823444.
- RE Ang, “Small-aperture intraocular lens tolerance to induced astigmatism”, Clin Ophthalmol, 12, 1659 (2018). PMID: 30233128.
- RE Ang, “Comparison of tolerance to induced astigmatism in pseudophakic eyes implanted with small aperture, trifocal, or monofocal intraocular lenses”, Clin Ophthalmol, 13, 905 (2019). PMID: 31213762.
- J Hooshmand et al., “Small aperture IC-8 intraocular lens in cataract patients: achieving extended depth of focus through small aperture optics”, Eye, 33, 1096 (2019). PMID: 30792521.
- S Srinivasan et al., “Posterior segment visualisation in eyes with small aperture IOL”, J Refract Surg, 35, 538-542 (2019) PMID: 31393993.
- S Manzanera et al., “Adaptation to brightness perception in patients implanted with a small aperture”, Am J Ophthalmol, 197, 36 (2019). PMID 30236772.
