
Eye health is an essential part of everyday living – and loss of vision to any degree can massively affect quality of life and impact the lives of friends and family. Age-related macular degeneration (AMD) is the most common cause of blindness and, in our aging population, is on course to become a significant healthcare burden. Dry AMD accounts for the majority of AMD cases but, unlike the wet form, there are no effective therapeutic options for patients. In the advanced form of AMD, geographic atrophy (GA), vision loss is irreversible.
Improving patient expectations
A major surgical intervention for AMD is the implantation of an intraocular lens (IOL) to improve eyesight. Although the surgery should improve vision, an underappreciated step in patient management is managing expectations for post-operative eyesight – because vision will not be restored to pre-AMD levels. This is where our Danish-Austrian collaboration is aiming to improve the situation – with a “Real-Life AMD” task-based questionnaire that specifically looks at AMD-related changes in vision (1).
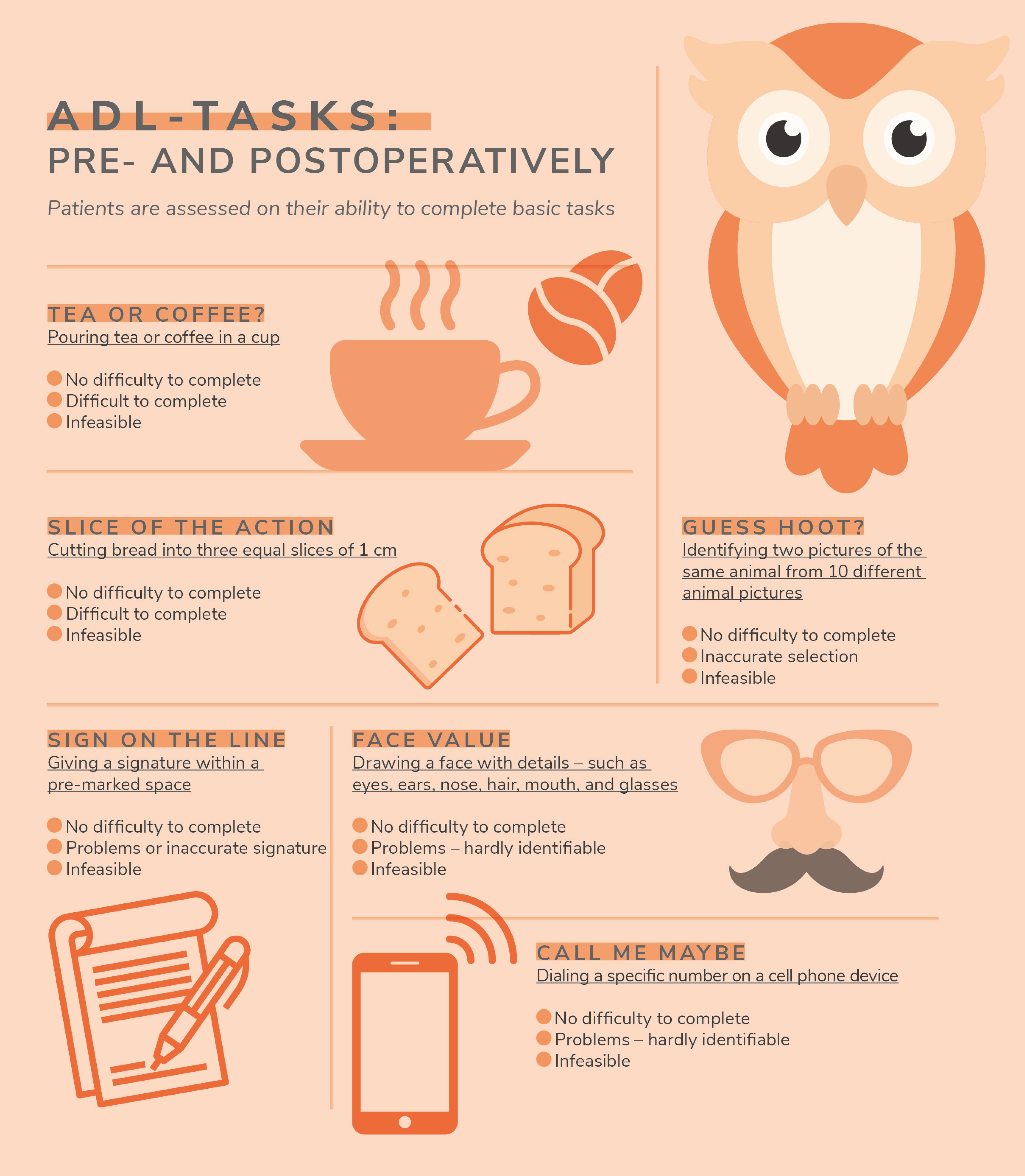
We do this by focusing on more rounded activities of daily living (ADLs), because AMD increases the risk of ADL task impairment 3- to 13-fold, depending on the condition’s severity. The key advantages of this assessment are that the test is simple enough to perform at home or in the clinic, it is reproducible, and the results of task completion or failure are extremely clear – for example, pouring a cup of tea or coffee. Clarity of results is a refreshing step forward; many other tests involve patient recollection and general impressions on the level of improvement, all of which will be heavily subjective and affected by other psychosocial factors.
The Real-Life AMD questionnaire can give an accurate assessment of pre- and postoperative vision for AMD patients, which enables the ophthalmologist to paint a better picture of future vision and improves patient satisfaction. This is important – patient satisfaction can reduce the risk of postoperative depression and other mental health problems that both negatively affect the patient and detract from postoperative vision training. Although improvements from IOL implantation may be modest, they nonetheless improve a patient’s vision and ability to perform ADLs.
There are great potential benefits from IOL implantation, but many ophthalmologists are unwilling to take this step. Reasons include concerns about surgical techniques, poor outcomes in previously treated patients, or even a misunderstanding over what is the best lens to select for a patient. This, too, can tie into patient expectation management, with poor patient preparation leading to poor feedback and a reluctance to repeat the procedure.

Trial and error
The complete lack of therapeutics to tackle dry AMD poses a significant problem – but one way to increase the odds of finding a treatment is to improve patient selection for clinical trials. Recruiting the wrong patients can affect the outcomes of clinical trials when looking at AMD specifically. A common example is when AMD patients also have a visual comorbidity such as cataracts – which can leave researchers wondering, “What is the real reason this therapeutic succeeded (or didn’t)?”
Most current AMD studies use Early Treatment Diabetic Retinopathy Study (ETDRS) chart-based assessments of vision – such as Best Corrected (Distance) Visual Acuity (BCDVA). Unfortunately, BCDVA does not correlate with dry AMD lesions – especially for GA – and therefore may not be appropriate for assessment of vision in AMD. There are other tests that are more rounded and applicable to AMD and GA – including NEI-VFQ-25, Functional Reading Index (FRI), novel patient-reported outcome (PRO), and maximum reading speed – which have all previously been used for either AMD or GA studies. But there are no assessments yet that are specifically designed for the challenges that arise from AMD.
Real life solution
Our assessment has been trialed in over 100 patients with various AMD-IOLs in both Denmark and Austria and may offer better visual functional assessment for both AMD and IOL implants, against static visual acuity measurements – providing applicable “true” and real-world results. Because the tasks are all very common activities to independent living, the test also serves as a reliable marker for patient expectations. We started our Danish-Austrian collaboration about five years ago and have published some interesting case reports (2–4), showing fantastic and surprising results in patients with low chances of success – proving the German idiom, “Those who are said to be dead, live longer.”
We welcome the use of our questionnaire in larger studies to validate its effectiveness in a broader patient population. Despite the increasing medical healthcare burden imposed by AMD there are still no validated tests for functional vision or PROs specifically for AMD – a gap that our questionnaire fills. Besides our Danish-Austrian collaboration’s efforts to improve patient outcomes, there are other research groups across the globe attempting to identify suitable vision and ADL tests. These could be incorporated into a central battery of core tests that clinicians can use for AMD patients. Therefore, we also believe that a white paper should be created by an AMD-IOL task force to set out the correct use of AMD IOLs, proper patient selection, and suitable evaluation methods.
References
- AF Borkenstein et al., “Improving Outcomes for Patients with Age-Related Macular Degeneration and Cataracts: The Importance of Including an Assessment of Activities of Daily Life (ADL),” Clin Ophthalmol, 15, 3333 (2021).
- AF Borkenstein, EM Borkenstein, “A case report detailing use of a new intraocular lens with advanced technology, designed specifically for patients with center-involving macular disorders,” Medicine (Baltimore,) 98, e16583 (2019). PMID: 31348295.
- AF Borkenstein, EM Borkenstein, “Four Years of Observation to Evaluate Autonomy and Quality of Life after Implantation of a High-Add Intraocular Lens in Age-Related Macular Degeneration Patients,” Case Rep Ophthalmol, 11, 448 (2020). PMID: 32999675.
- AF Borkenstein, EM Borkenstein, “Creating Hybrid Monovision with 7.0 mm XL Optic and High-Add AMD Intraocular Lenses (XL-MAGS) in a Patient with Retinitis Pigmentosa,” Case Rep Ophthalmol, 10, 304 (2019). PMID: 31762761.
