
At a Glance
- SFT is an alternative method of pupilloplasty, requiring the surgeon to pass the suture end through the loop four times
- Compared with current pupilloplasty methods, it offers faster visual recovery and reduced postoperative inflammation
- Reconstructing the pupil this way prevents patients from glare, photophobia and untoward images formed due to reflection of light
- PPP with SFT is suitable for patients with a range of visual disorders – from high astigmatism and corneal injuries to post-penetrating keratoplasty.
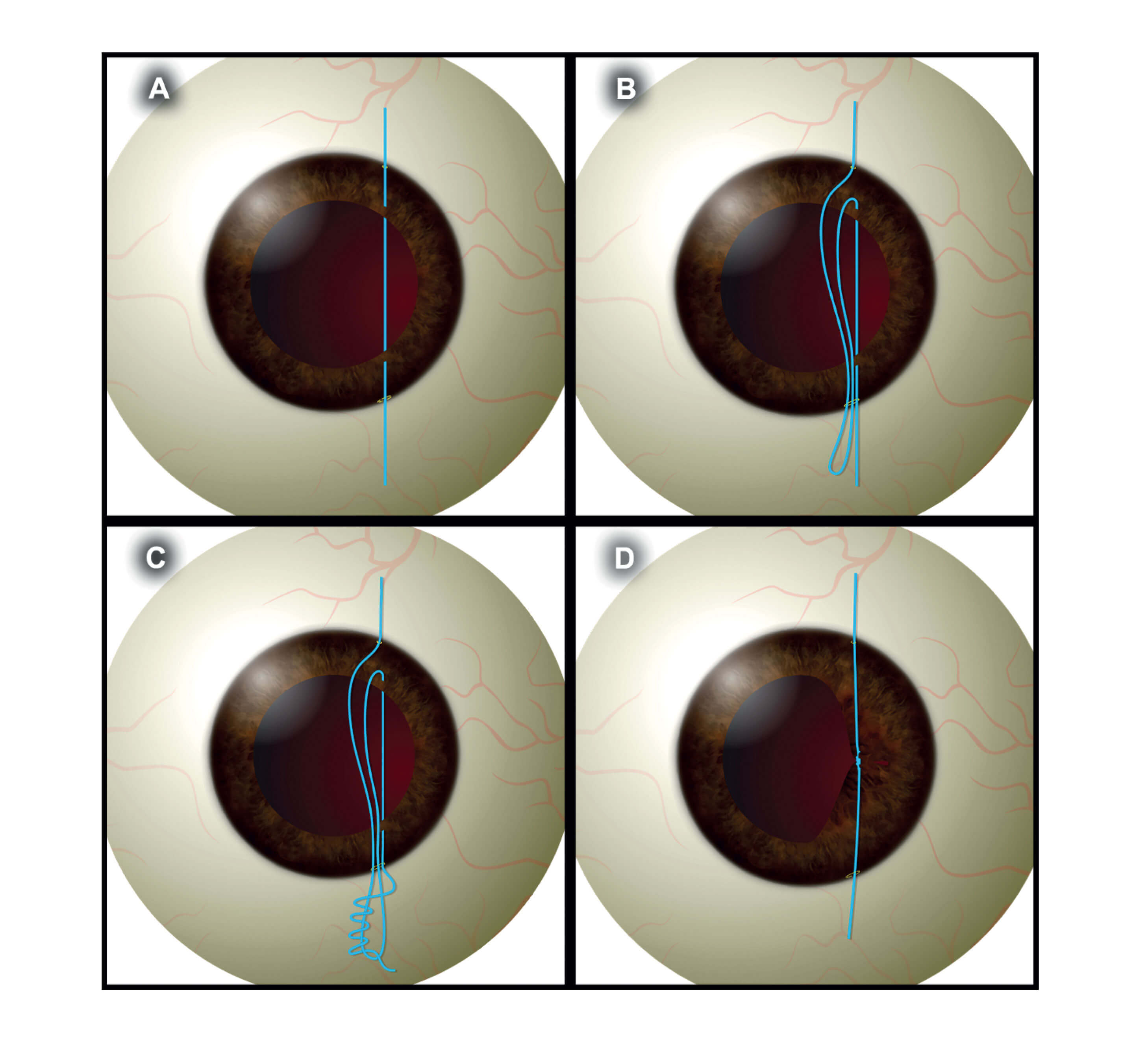
Single-pass four throw (SFT) pupilloplasty is a relatively new surgical technique (1). It was initially described as a modification of the Siepser’s method, but the knot formation has been found to belong to the Timber Hitch method of tying. In this technique, a 10-0 or a 9-0 polypropylene suture attached to a long arm needle is passed through the proximal iris tissue that is to be involved in the pupil reconstruction. A 26 G needle is introduced from the paracentesis in the opposite direction, where it engages the distal iris tissue to be approximated (Figure 1 A). The 10-0 needle is then passed in to the barrel of the 26 G needle, before it is withdrawn from the eye. A Sinskey’s hook withdraws the loop of the suture (Figure 1 B) and the suture end is passed from the loop four times, thereby taking four throws (Figure 1 C). Both the suture ends are pulled, and the loop slides inside the eye, thereby approximating the pupillary edges together (Figure 1 D). A micro-scissor is introduced inside the eye and the suture ends are cut. The helical structure created due to the loop approximation forms a self-locking and a self-retaining knot inside the eye.
Figure 1. Surgical technique of single pass four throw (SFT)
A – The 10-0 suture is passed through the proximal and distal iris tissue.
B – A loop of suture is withdrawn from the anterior chamber with a Sinskey’s hook.
C – The suture end is passed through the loop four times.
D – Both the suture ends are pulled and the loop slides inside the eye approximating the iris tissue.
A recent study has demonstrated the scope of pupillary dilation after SFT (2), allowing posterior segment surgeons to visualize the fundus and perform any retinal procedures that may be needed in future. SFT is also faster and easier to perform than current forms of pupilloplasty, including both the modified Siepser’s and McCanell methods. These procedures are more time intensive, requiring more than two passes to be made from the anterior chamber – as well as additional manipulation of the iris tissue – whereas only a single pass is needed with SFT. But reduced postoperative inflammation and faster visual recovery are not the only benefits of the technique.
SFT has been found effective for a number of conditions – including patients with Urrets Zavalia syndrome who present with raised IOP and persistent pupil dilation (3). As SFT pulls peripheral iris tissue, it prevents secondary angle closure, breaking the formation of peripheral anterior synechias and inhibiting the mechanical blockage (4). SFT has also been found effective in selected cases of secondary angle closure, along with silicon oil induced glaucoma (5). Because the knot formation associated with SFT is almost parallel to the surface of the iris (6), it is beneficial for patients undergoing endothelial keratoplasty as the manipulation involving graft unrolling occurs in the center of the pupil area where the knot is present. Studies have also found SFT useful in treating patients with higher order corneal aberrations (7). The pinhole pupil is 1.5 mm in size, and as such, blocks the stray light emanating form the peripheral cornea and decreases the overall aberrations of the optical system of the eye.
In summary, SFT is the latest variant amongst pupilloplasty procedures with a very effective implementation for perfomig a pinhole pupilloplasty (PPP). Studies have reported a statistically significant difference in the Chord MU values after performing PPP using this technique, along with an improvement in visual acuity. SFT is easy to perform, with the added advantage of requiring minimal intervention inside the anterior chamber. Importantly, reconstructing the pupil this way prevents patients from glare, photophobia and untoward images formed by reflection of light.
How does pinhole pupilloplasty work exactly?
Let me tell you about a marine mollusc called the nautilus! The eye of the nautilus does not have a lens – it is aphakic by design. Instead, nature has built it in such a way that it has a pinhole eye, so it can see better. We are using the same principle in our SFT technique to improve our patients’ vision.
The basic principle is to make the pupils small – 1.5 mm or less. PPP is usually performed so that rays of light are blocked from the peripheral cornea and focused only on the center of the pupil, thereby increasing visual acuity. According to the Stile-Crawford effect – referring to the directional sensitivity of cone photoreceptors – light that enters the center of the pupil produces a greater photoreceptor response than light that enters the periphery.
What makes it so effective?
Its simplicity. Every optician, optometrist and ophthalmologist uses a pinhole. You don’t have to be a very skilled surgeon to do it, and there are no expenses involved. All you need is a suture and a microscope light to establish a visual axis.
What advantages does SFT have over other methods?
The beauty of this whole procedure is its speed – it takes 10 minutes at most. Compare that with the alternatives: both penetrating and pinhole IOL are significantly more time-consuming. But what if you don’t have the IOL, or you do have it, but don’t have FDA approval? By choosing pinhole pupilloplasty, these problems are negated.
And the results?
We’ve had phenomenal success so far. We have done around 20 cases, which is a large number for such a new technique, and our first case was a patient with astigmatism of 24 dioptres who had a patch graft during small incision cataract surgery. Four days after SFT PPP, the patient’s vision had improved to 6/12. We have made sure to operate on patients with different conditions, such as corneal ring segments and corneal injuries, and combined it with IOL implantation to experiment with extended depths of focus.
Which patients are suitable for this operation?
Patients with:
- high astigmatism
- corneal injuries
- highly abberated corneas
- post-penetrating keratoplasty
- intra-corneal ring segments…
It is an extremely versatile technique!
Does it work on phakic patients?
It does, but I suggest making them pseudophakic first – removing the cataract and implanting the IOL before you do the pinhole pupilloplasty to avoid damaging the crystalline lens.
Are there any repercussions to having smaller pupils?
Not at all. For argument’s sake, let’s say the patient developed detachment a few years after the operation. If you want to treat them surgically, all you need to do is treat the iris with a Yag laser, and the pupil will dilate, so you can examine them as usual. As for field effects and contrast sensory, those aren’t affected at all from what we have seen. All in all, SFT is a simple, cost-effective procedure, which can be done by every ophthalmologist in the world – without any long-term implications.

References
- 1. P Narang et al., “Single-pass four-throw technique for pupilloplasty”, Eur J Ophthalmol, 27, 4, 506-508 (2017). PMID: 28009401. 2. D Kumar et al., “Single-pass four-throw pupilloplasty: Postoperative mydriasis and fundus visibility in pseudophakic eyes”, J Cataract Refract Surg, 43, 1307-1312 (2017). PMID: 29056302. 3. P Narang et al., “Single pass four throw pupilloplasty for Urrets-Zavalia syndrome”, Eur J Ophthalmol, Mar 1:1120672117747038. doi: 10.1177/1120672117747038. [Epub ahead of print] (2018). PMID: 30058383. 4. A Agarwal et al., “Single pass four-throw pupilloplasty for angle closure glaucoma”, Indian J Ophthalmol, 66, 120-124 (2018). PMID: 29283136. 5. A Agarwal et al., “Single-pass four-throw pupilloplasty for secondary angle-closure glaucoma associated with silicon oil tamponade”, Eur J Ophthalmol, 1 (2018). PMID: 2987701. 6. A Agarwal et al., “Single-Pass 4-Throw Pupilloplasty for Pre-Descemet Endothelial Keratoplasty”, Cornea, 36, 1580-1583 (2017). PMID: 28957977. 7. Pinhole pupilloplasty (ppp): small aperture optics for higher order corneal aberrations. J Cataract Refract Surg 2018; Article in Press.
