
Phoebe Harkin interviews Greg Jackson
In 1993, Greg Jackson was a graduate student at the University of Alabama at Birmingham. He was working in a laboratory with Cynthia Owsley, a pioneer in research on contrast sensitivity and driving – famous for her work into how vision changes with age. Owsley had become interested in night vision in older adults and passed the project on to Jackson. “As no one thought much of it back then, it was a perfect topic for a graduate student. I couldn’t mess it up – or so it seemed!” says Jackson. There wasn’t much information available on the subject: they knew that night vision worsened with age because of aging-related changes in the eye’s optics, but it was unknown as to whether or not the retina was partly responsible for senescence of night vision. They started to investigate dark adaptation – the ability to adjust to darkness. “If you think about visual acuity as a proxy measure for daytime vision, dark adaptation is a proxy measurement for the ease or difficulty in which a person sees at night,” explains Jackson, whose doctoral dissertation topic explored whether older adults had decreased ability to adjust to darkness because of senescence of the retina. To measure dark adaptation, you can present a flash of light to the eye and then repeatedly measure light sensitivity. Over time, the eye will detect progressively dimmer lights – much like how one can see progressively see fainter stars in the night sky. Notably, a young person’s recovery time is significantly faster than an adult over the age of 60.
“Of course, you couldn’t just buy a dark adaptometer in those days,” says Jackson. “Equipment had to be modified or re-programmed to measure dark adaptation.” And so, with the help of a heavily-modified Humphrey Field Analyzer, he started measuring patients’ ability to dark adapt, and all was going smoothly.
A curious thing happened then: he flashed the light at one 72-year-old patient and waited for recovery. “Ten minutes went by. Then 18, then 20, then 25,” Jackson says. “Still no recovery. I started to panic, and by the time half an hour rolled around, I was ready to turn the machine off.” He remembered sitting there in defeat, working out how he’d tell Owsley that he had not only broken the machine, but also wasted the patient’s time. But then, 40 minutes into the test – 30 minutes longer than expected – the patient began to slowly recover. When he turned the machine off at 90 minutes, the patient – later to be known as “the first patient” – was still not fully recovered. “I couldn’t believe it,” says Jackson. “But it happened again… and again.” The team collected five cases of patients with normal retinal health but clearly abnormal dark adaptation. Serendipity had struck – but Jackson didn’t know it yet.
To get to the bottom of these cases, they sent the first patient to see two retina specialists – only to be told that there was nothing wrong. But how could that be true? They sent photographs to the Beaver Dam Reading Center, forerunner of the AREDS Reading Center at the University of Wisconsin, for evaluation. Again, they graded the patient as normal. No comorbid health problems, no further explanation. So what was it?
Friends in interesting places
Christine Curcio, one of Jackson’s colleagues, was studying the retinas of patients with AMD around the same time. Curcio found that older adults generally lose more rods than cones, but when they develop AMD, their rods are affected significantly more – and earlier – than cones. It appeared that rods were almost acting as an early warning system for AMD in the retina. To test that theory, Jackson began measuring dark adaptation in AMD patients and found that their ability to adapt was massively delayed.
“At this point, that first patient was four years older – and had developed AMD,” says Jackson. He went back and re-analyzed his early data and, sure enough, found that patients with the appearance of a normal retina but worse dark adaptation were more likely to develop AMD than their peers with better dark adaptation. They never published that data, but they didn’t forget it either. Indeed, that initial study formed the foundation of later work – but it took Curcio to put the pieces together.
While researching the donor eyes of AMD patients, Curcio made a startling discovery: cholesterol deposition at the back of the eye, which can’t be seen with imaging technology, is the forerunner to drusen – the defining feature of macular degeneration. Up until then, everyone believed drusen were focal. “Curcio upended that theory,” says Jackson. “She found that when RPE becomes dysfunctional, it starts depositing cholesterol throughout the back of the macula – and she used microscopy on donor eyes to prove it.” When cholesterol becomes sufficiently thickened, it becomes visible (a druse). In other words, by the time a clinician can see a druse, they’re looking at the tip of an iceberg – and the damage is already well underway. Not only that, Curcio discovered that the cholesterol in a druse is the same type of cholesterol as that found in carotid arteries of patients with atherosclerosis. “And that was significant. As with atherosclerosis, this cholesterol causes oxidative stress and inflammation – stress that could be quenched with antioxidant supplements,” Jackson says.
This knowledge, paired with the understanding that vitamin A was essential for dark adaptation, formed the basis of the team’s next study: a small, randomized, controlled clinical trial where patients were supplemented with vitamin A. Jackson explains: “The test was never intended to treat the disease, it was meant to prove that the cholesterol layers serve as a barrier to vitamin A reaching the outer retina, essentially causing the localized vitamin A deficiency which impairs dark adaptation – and that’s exactly what it did.” And they finally determined why patients with AMD exhibited extreme dark adaptation impairment; even before a patient has drusen, they have cholesterol deposits at the back of the eye that are limiting vitamin A from getting to the outer retina. The result? Impaired dark adaptation. “And for those persons that do have clinically identifiable macular degeneration, dark adaptation impairment can be used to identify the disease with 90 percent accuracy,” says Jackson. They’d found the last missing piece of the puzzle and, just like that, Greg Jackson’s life changed.

A fork in the road
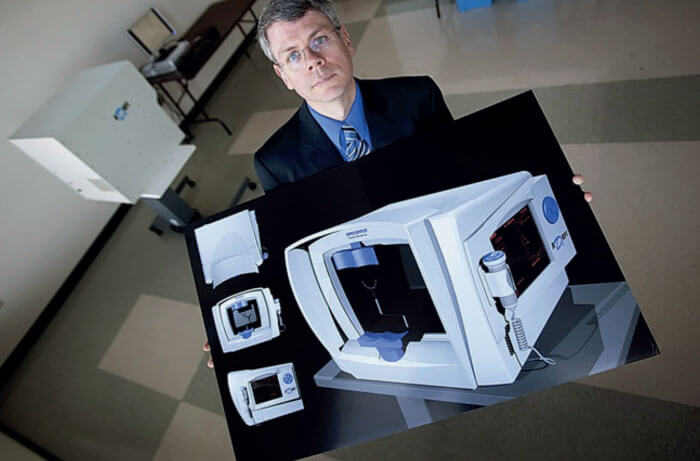
“If you had asked me what career I wanted while working in Owsley’s lab, I would have said, ‘academic researcher,’” says Jackson. But something happened when he was doing the experiments. He ended up spending a lot of time with patients – four to six hours doing tests and filling in questionnaires. Invariably, he would end up hearing about how the patient had come to know that they had macular degeneration. “Many of them told me that they were unaware of their disease before they had severe vision loss in one eye,” he says. Their stories always followed the same pattern: they would realize their visual acuity had dropped in one of their eyes, but they did not go to the doctor. When they finally did, they were diagnosed with AMD. “As I heard more and more stories, I couldn’t shake the irony that I was using a modified visual field machine – the gold standard diagnostic for glaucoma – to measure dark adaptation,” says Jackson. Then, one day, it hit him. “If technology has enabled doctors to accurately diagnose and monitor glaucoma, then why aren’t we using technology to find and monitor AMD?” And that was the moment Jackson decided to build a modern, clinically-accessible dark adaptometer. He had a prototype. He had identified a need. Now all he needed was a buyer.
Nothing in life is so simple, however. And the first challenge Jackson faced was the test duration. With the laboratory prototype, it could take an hour to assess someone’s dark adaptation, significantly longer than a routine clinical visit. “If I wanted doctors and patients to get on board with this idea, I would have to shorten the test – dramatically,” he says. Even with this limitation, he approached industry. Jackson talked to every major company asking them about the opportunity and they all correctly told him that he was crazy. “No one wanted to take it on,” he says. “I realized that I needed to change tactics.” And so he decided to license the technology to an entrepreneur and commercialize it. They signed the license agreement in March 2004 to a company called Apeliotus Life Sciences, the forerunner to MacuLogix. With the help of John Edwards and Bill Grace, Jackson spent the next 10 years shortening the length of the test and optimizing the technology. Today, the device can test if someone has normal dark adaptation in six and a half minutes or less.
The second challenge was deciding how to explain dark adaptation. “Though dark adaptation isn’t terribly complicated, it’s complex enough that doctors might not understand if I was to say, ‘The patient has a change in the slope of dark adaptation as expressed in log units of sensitivity change per minute,’” admits Jackson. To make dark adaptation easier to understand – and easier to explain – they decided to redefine the way they talked about it altogether. Thus, they invented the Rod Intercept (RI) – a single parameter to estimate the speed of dark adaptation. The Rod Intercept is simply the time in minutes by which nearly complete dark adaptation has occurred. “Faster times are better and slower times are worse. Simple.”
The change in approach was effective. The team installed the first AdaptDx automated dark adaptometer to be used in a clinic in 2014, almost ten years to the day that the technology was licensed. It had been a long road – ten years of trial and error, breakthroughs and setbacks – but there was more to come. When Jackson started this project, he assumed his greatest challenge would be convincing doctors that dark adaptation was the best method to detect early AMD. As it turned out, the challenge was convincing them that early AMD was worth detecting at all.

Talking the talk…
“General ophthalmologists and optometrists rarely give bad news,” says Jackson. Indeed, ophthalmologists work in one of the few specialties where most of the patients who walk into their clinics, walk out of happy. Cataracts can be removed. Refractive errors can be corrected. Ocular surface diseases can be treated. But what about outcomes for AMD? “If you’re a middle-aged optometrist or ophthalmologist in the United States, you probably didn’t learn much about macular degeneration in medical school – and why would you?” asks Jackson. After all, there were no supplements or anti-VEGF injections back then. There was nothing an ophthalmologist could do to save a patient diagnosed with macular degeneration from losing their sight; severe vision impairment was a very real possibility. “In some ways, it makes sense that these same doctors did not tend to focus on managing AMD patients,” he says. But it was exactly those doctors who Jackson needed to invest in his technology. To convince them, the original team had to reframe how they thought about AMD altogether.
There is a marketing theory that any type of disruptive technology – whether it be an Apple computer or a smart phone – requires an educational sell. “Steve Jobs had to tell people why they needed a computer in their life because they hadn’t a clue. After all, why did a normal person need a computer back then?” asks Jackson. “Steve Jobs found a way to convince them.” Jackson knew it was his job to sell dark adaptation. But how? They started with the very basics: reminding doctors of the prevalence of the disease. Many doctors were surprised that AMD is three more times prevalent than glaucoma. They would remind doctors that AMD is a progressive, chronic disease with no cure, like diabetes. “When you start thinking about the disease that way, you become much more serious about prevention,” says Jackson. “Because, like diabetes, early diagnosis leads to earlier treatment and better patient outcomes.” Next, they had to educate them about the value of supplements, and how diet, exercise and comorbid disease management could help decrease the patient’s risk of disease progression. And that brought Jackson and his team to the second part of their educational sell: how to identify AMD patients.
The hard sell
“These patients are already in your practice. They will be in your waiting room right now and you’ll probably send each of them home without a diagnosis…” – that’s exactly how Jackson used to begin his pitch to doctors in the early days. If a doctor didn’t believe him, Jackson would propose a test, and ask them to pick patients over the age of 60 years old who they were absolutely sure did not have age-related macular degeneration. Jackson would offer to test them, and guarantee that at least 20 percent will fail.
“Typically, 30 percent of the patients failed,” he says. “Long-overdue retinal images would be taken, and, in most cases, the diagnosis of AMD was confirmed. And the doctors would despair. How could they possibly have missed that many patients?” For Jackson, the answer was clear: the current method of identifying AMD is fatally flawed.
“Doctors have been taught to look for drusen during the clinical examination, but they are often missed,” says Jackson. “Even the most keen-eyed ophthalmologist can miss a druse if they aren’t looking for one. The first thing most ophthalmologists do is review their patient’s visual acuity. If that patient has 20/20 vision, the ophthalmologist is more likely to miss a druse because they are not alerted that there is a problem. If they don’t see a druse, they won’t send them for a photograph. That’s our current protocol for diagnosing macular degeneration. Is it any surprise that AMD patients are going unnoticed?”
The opportunity to outlive our eyesight
The magnitude of AMD under diagnosis alarmed Jackson. He was also shocked by some of his colleagues who were less surprised, contending that, if the disease is missed in its earliest stages, the patient is at very low risk of vision loss, and it will be caught later when AREDS2 supplements are indicated. Jackson’s perspective was different; his focus was clearly set on AMD as a progressive, chronic disease: “Their five-year or even ten-year risk may be low at that point in time, but what is their twenty-year, thirty-year or even forty-year risk of vision loss?” Some patients are diagnosed with early AMD in their 50s and so are likely to have the disease for multiple decades. Jackson believes that patients in the earliest stages of the disease may modify their risk of progression, but they must be given the diagnosis and education to give them an opportunity to preserve their sight. “As people continue to live longer, I felt it was vital to give AMD patients their best chance at outliving their eyesight.”
Today, Jackson and his team are working hard as a company to educate doctors about AMD diagnosis and management. In fact, their company is built with the aim of eliminating blindness caused by AMD altogether. They have installed dark adaptation devices throughout the USA, and are now branching out into Europe, Canada and Australia. With every installation comes a new story of a doctor diagnosing a friend, a partner or even themselves. One employee asked for her parents to be tested after overseeing the installation of a device into the practice that provides eyecare to her family. Her mother failed the dark adaptation test and was subsequently diagnosed with AMD. Her mother now has the chance of a better outcome than her own parents, who previously lost vision in both eyes because of CNV. “If the doctor did not employ the technology, who knows how long it would have been before the diagnosis?” asks Jackson.
Over the 18 years Jackson has been investigating dark adaptation, he has learned that a doctor’s good days are the direct result of good patient outcomes. So, he’s made it his personal mission to lessen the number of bad days – for patients and doctors. “Early adopters often tell me how this technology has helped patients enjoy better outcomes and it is their testimonials that are helping to spread the word about dark adaptation,” says Jackson, with significant pride. This article marks a 15-year anniversary for MacuLogix. “Ten years of science and engineering, followed by another five realizing its true potential for patients and doctors,” says Jackson. “Here’s to the next 15!”

