In a perfect world, every patient who wants and needs a presbyopia-correcting IOL would receive one. But in the real world, this aspiration is tempered by considerations of IOL safety and performance. Such issues mandate a degree of patient selection: we must ensure a safe implantation procedure above all else, but we must also consider which patients are likely to be satisfied with the inherent compromises regarding spectacle independence and quality of vision. How can we distinguish between different presbyopia candidates and manage them accordingly? I advise paying attention to three key areas:
- Pre-existing anatomy and pathology
- Likely long-term sequelae of existing disease
- Personality and needs of the patient
Pre-existing anatomy and pathology
All candidates for presbyopia correction should be screened for pre-existing diseases. Among systemic conditions, be particularly alert for diabetes, rheumatoid arthritis and Sjögren’s syndrome. Regarding ocular conditions, be sure to thoroughly check all patients for ocular surface disease; if present, make every effort to resolve it prior to any lens implantation procedure. Screen for glaucoma, and don’t forget to look for corneal irregularities, including keratoconus and pellucid marginal degeneration. Also, assess the ocular endothelium, and note the consequences of any prior refractive surgery. Finally, observe the status of the vitreous, and use OCT or angio-OCT to identify any pre-existing macular disease.
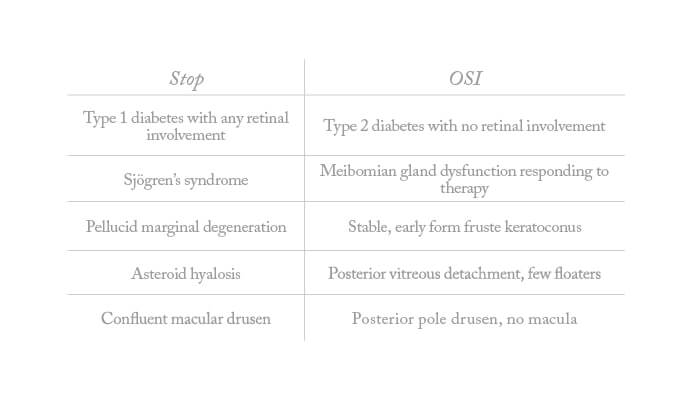
Screening patients in this methodical way should allow you to identify conditions that may compromise the safety of presbyopia correction. But do exercise judgment when acting on your findings – not every pre-existing issue rules out a presbyopia-correcting IOL (Table 1: “Stop or Go”).
Table 1. Stop or Go? Pre-existing disease and presbyopia-correcting IOLs

Long-term sequelae
In making the final decision regarding presbyopia correction in patients with pre-existing conditions, I am guided by the types of long-term sequelae that might reasonably be expected given the condition in question. In brief, we should be very cautious where expected sequelae include macular dysfunction, decreased contrast sensitivity, or tear film deterioration. Conditions which may contra-indicate presbyopia correction therefore include glaucoma, macular degeneration, pucker, and severe systemic disease, such as diabetes, rheumatoid arthritis, and Sjögren’s syndrome. In short, if the pre-existing condition may progress to significant vision impairment, I prefer not to implant a presbyopia-correcting IOL.
Patient factors
Lastly, it is very important to understand the specific motivations and needs of the patient with regard to presbyopia correction. How old is the patient? What kind of job and leisure activities are they likely to do – now and in the future? What level of spectacle independence do they seek, and for what activities? In brief, the surgeon should take time to assess key aspects of the patient’s lifestyle, and very much take these into account when advising the patient about presbyopia-correcting IOLs.
In this context, relevant evaluation techniques include chair-time conversations, discussions with relatives and friends, and self-assessment questionnaires. Always remember that the most important thing is to grasp what patients really want: hence, chair time is necessary not so much for explaining things to patients, but for truly understanding them. To give a simple example, a typical Nordic computer worker, very tall, will probably want to read from a computer screen at a significant distance because his arms are relatively long. By contrast, a little old lady who wants to read small print is more likely to benefit from optimization of near vision. Thus, different patients have rather different needs, which in turn will dictate different IOL parameters. And that’s why it is important to first understand and then match each person’s specific requirements to the most appropriate surgical option.
The art of compromise
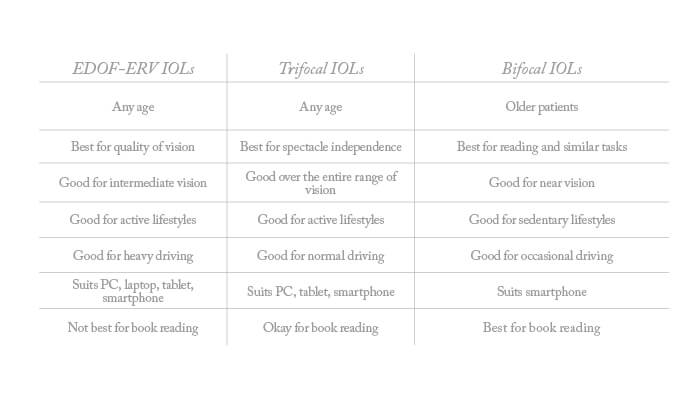
To appropriately advise your patients you must also understand the respective performance attributes of available presbyopia-correcting IOLs: some are better for one purpose, others are more suitable elsewhere (Box 1). In particular, some provide more presbyopia correction than others – an important point because, the more presbyopia correction provided by an IOL, the greater the chance of associated visual disturbances. Take care to inform your patients of this inverse correlation between spectacle independence and quality of vision; it is vital that they understand the compromises inherent in each of the three categories of presbyopia-correcting IOLs.
Once the patient has a realistic expectation of the level of presbyopia correction that can be attained, and a clear understanding of the visual compromises required for this, we can confidently undertake surgery to deliver both expectation and compromise. In my experience, patients usually understand and accept the trade-offs without any problem. Thus, communication of the level of spectacle-independence that an IOL will provide, and the associated effects on quality of vision, are key to keeping patients happy.
Nevertheless, I always try to under-promise and over-deliver. Above all, I am careful to manage expectations regarding haloes. I do not say that the haloes they see on day one will completely disappear, because this almost never happens and then the patients then get worried or frustrated. It’s not fair to set patients waiting for something that probably won’t happen; rather, I prefer to tell them that they’re likely to experience small haloes, but they won’t be bothersome and won’t affect their ability to do what they want to do, like driving. And then, when the haloes decrease, or even disappear, the patients are even happier. So my philosophy is to relieve them of the expectation of vision that is completely free of haloes or glare, and then they are not concerned if they have a very mild vision impairment at night.
Communicate the compromise, set the expectation, accept the outcome
- Disclose the compromise involved with presbyopia-correcting IOLs, and help the patient fully understand it
- Ensure the patient has a clear and realistic expectation of the level of spectacle independence attainable by the IOL
- Ensure the patient is willing to accept the compromise necessary to meet the expectation
The right IOL for the right patient
EDOF-ERV IOLs
Nearly half (47.5 percent) of patients are suited to EDOF-ERV IOLs, where the compromise in terms of quality of vision is low. Typical patients include those who want spectacle independence but are concerned about quality of vision (for example, because of active lifestyles with high demands for distance vision and significant demands for intermediate vision). Taller patients, and patients unsuited for trifocals, also tend to benefit from EDOF-ERV IOLs. For this category of patient, I set post-operative expectations as follows:
- You will be independent of spectacles in a manner fitting your lifestyle, but you may need glasses for near vision (but good illumination may allow spectacle-free reading)
- Your vision quality will be almost uncompromised and you will experience almost no glare or haloes at night
Trifocal IOLS
Patients most suitable for trifocal IOLs (again, 47.5 percent) tend to be active patients seeking complete spectacle independence, who are willing to accept small compromises in quality of vision. Patients who have received laser vision correction are also suitable for these lenses. For these patients, I set post-operative expectations as follows:
- You will attain almost complete spectacle independence but may need good lighting to read (or require glasses when reading in poor light)
- A consequence of almost complete spectacle independence is that you may experience some glare and haloes at night – this is normal
Bifocal IOLs
Only about 5 percent of my patients are good bifocal IOL candidates. Mostly, these are previously myopic patients in the range -2.5 to -4D, who used to read without spectacles and who now seek spectacle independence for near vision; they have few activities based on intermediate vision. For these patients, I set post-operative expectations as follows:
- You will be independent of spectacles over a wide range of distances, with very good reading vision
- However, you may require spectacles for intermediate vision, and you may need good light to read small print, or glasses when reading under very dim light conditions
- You may experience some glare and haloes at night; these are likely to decrease with time but in some cases may never fully disappear
Finding the balance
In conclusion, having fully appraised the patient of the compromises associated with presbyopia-correcting IOLs, and of the degree of spectacle independence they can realistically expect, I make sure that the patient is willing to accept the compromise required to attain the expected outcome. Only then do I perform the surgery required to meet those patient expectations, which involves careful choice of IOL category and power. Always under-promise and over-deliver: this avoids the patient having unrealistic expectations – and developing unjustified concerns – regarding visual disturbances. Using my approach, I believe you will find that many patients experience a better outcome than they had expected, and are correspondingly happier with the surgery.
