• Micropulse transscleral cyclophotocoagulation (MP-TSCPC) has proven to be a safe, effective and reliable approach for lowering IOP
• Unlike other interventions, MP-TSCPC delivers energy in a 31.3 percent duty cycle, allowing tissue to cool between each application, so there is minimal impact on target tissue and a reduced risk of injury to adjacent ocular tissue
• MP-TSCPC can be used early in the disease course and requires minimal medication, reducing the reliance on anti-inflammatory drops post-procedure
• It can also be used on a wide range of glaucoma severity, not just those in the most advanced stages of disease progression.
As the only fellowship trained glaucoma and advanced anterior segment specialist (GAASS) in the province of New Brunswick, Canada, I see many patients who have traveled great distances to reach my practice. This scenario can create logistical challenges in following a condition that requires close monitoring, not to mention that long-term success in managing glaucoma often depends on timely escalation of therapy. Because many of my glaucoma patients are followed locally by a comprehensive ophthalmologist, there may be delays between the documentation of IOP elevation or disease progression and the patient coming back to my office for an evaluation. Even if a new intervention is performed during this follow-up, it may be some time before it effectively lowers the pressure.
An overall trend in glaucoma is the increasing popularity of procedural interventions, ranging from laser to minimally invasive surgeries. Generally speaking, this development has reduced the need to rely on patients instilling drops on a routine basis, while also offering advantages for avoiding IOP fluctuations. There are several options within the category of procedural glaucoma interventions, and some of them may be more advantageous in terms of follow-up protocols.
In my practice, the addition of the micropulse transscleral cyclophotocoagulation (MP-TSCPC) procedure with the MicroPulse P3 probe and the Cyclo G6 Glaucoma Laser (Iridex) has proven to be a safe, effective and reliable approach for lowering IOP. The vast majority of patients who travel to see me and have been treated with MP-TSCPC are able to perform their follow-up with a local comprehensive ophthalmologist, only returning to my clinic if further intervention is warranted. Because it differs from traditional cyclodestructive procedures, MP-TSCPC treatment has also proven to be a versatile option for a diverse range of patients in my practice.
Cyclodestructive procedures have historically been reserved for more advanced glaucoma – most typically for refractory cases or individuals with poor visual prognosis. The classic thinking has been that because these treatments damage the secretory epithelium of the ciliary body, they should be used as a last resort to reduce aqueous production before opting for incisional drainage procedures. The procedure with the MicroPulse P3 probe is different in this regard. As the name implies, MP-TSCPC is unlike traditional transscleral cyclophotocoagulation, which is performed with a continuous wave laser. MP-TSCPC uses energy that is delivered using a 31.3 percent duty cycle (0.5 milliseconds on, 1.1 milliseconds off), thereby allowing the tissue to cool between each application. As a result, there is minimal impact on target tissue and a reduced risk of injury to adjacent ocular tissue. Because there is no remnant scarring, MP-TSCPC is also repeatable if the target pressure is not achieved after the first application.
In various clinical trials, MP-TSCPC has been shown to achieve up to 30 percent reduction in IOP with reduction of an average of one medication (1, 2, 3, 4). Interestingly, most of the current literature with this modality is in patients with relatively high baseline IOP, suggesting enrolled patients had more severe glaucoma at the time of treatment. Though cyclophotocoagulation reduces production of aqueous humor, there is a possibility that MP-TSCPC may also increase uveoscleral outflow. With this is mind, MP-TSCPC could be an option for a wider range of patients than has been suggested in studies. Personally, I have used MP-TSCPC on patients with what I would call mild to wild glaucoma – and for good reason. It is safe and effective without yielding major impact on the target tissue, and it’s repeatable if necessary. It makes as much sense for a patient on two to three drops with uncontrolled pressure or those who cannot manage drop therapy but who are not yet indicated for frank glaucoma surgery (penetrating filtration surgery or MIGS) as it does for those patients with neovascular glaucoma. With regard to patients who travel to see me, I have found that I can intervene early in the disease course with MP-TSCPC to get the pressure under control, and then have them followed locally with low medication requirement, reducing the reliance on anti-inflammatory drops post-procedure.
I learned an interesting lesson with my first few cases of MP-TSCPC. Initially, I would prescribe a steroid and a nonsteroidal anti-inflammatory, and ask patients to return in two weeks – which is what I would have done had the treatment been performed with a continuous wave laser. Despite some of these patients not using their drops, I found no signs of active inflammation when I saw them again. As a result, I now only rarely use an anti-inflammatory protocol after a MP-TSCPC treatment, and plan for the first follow up at five or six weeks. This significant change has had a positive impact on my patients’ daily lives, particularly for those who have to travel long distances to see me.
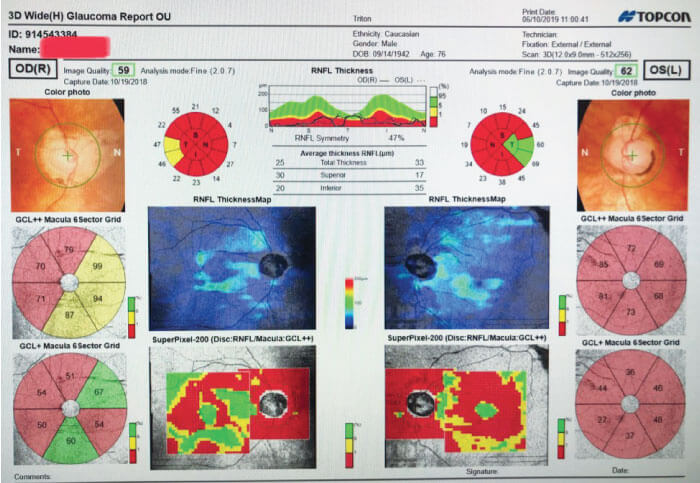
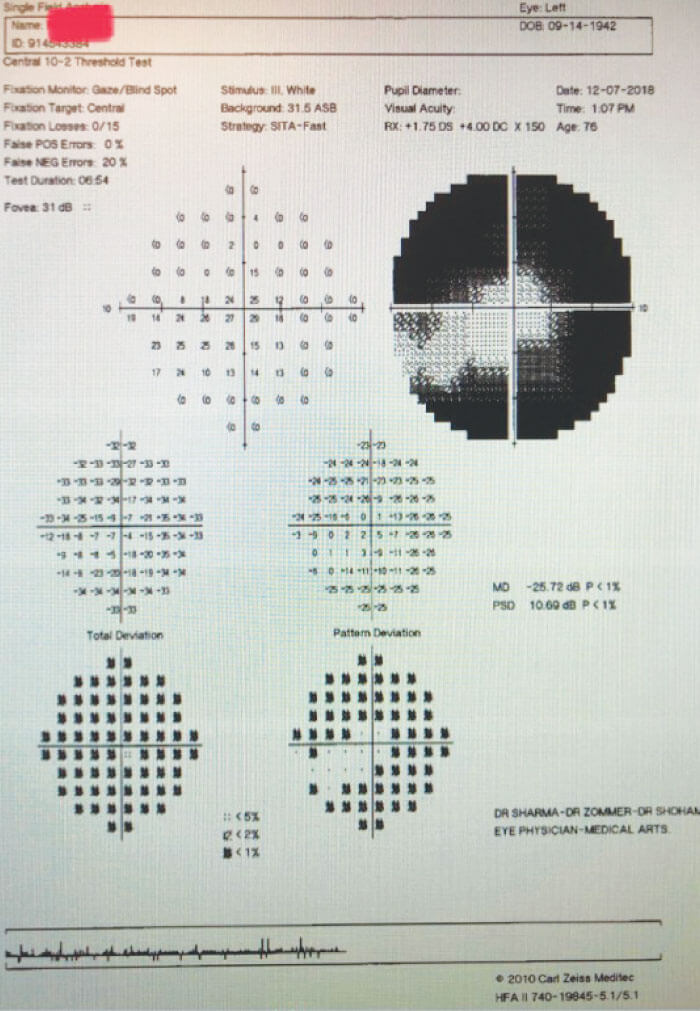
A recent case of a 76-year-old man with advanced primary open-angle glaucoma (Figures 1 and 2) demonstrated the benefits of MP-TSCPC. In addition to an eye condition, the patient was in poor health, which presented a challenge when it came to frequent monitoring examinations. His ocular history included a previous trabeculectomy and, at the time of the visit, his IOP was 20 mm Hg, which was above his target pressure. He stated he was having difficulty tolerating his ocular medications. The patient was on a combination drop (beta-blocker and carbonic anhydrase inhibitor) taken twice daily and a prostaglandin analogue at bedtime. Due to his overall medical condition and extent of his disease (remaining 5 degrees of fixation on visual field), I determined that the patient was not a good candidate for frank filtration surgery and that additional medications would not be helpful. The decision was made to offer MP-TSCPC using the MicroPulse P3 probe and the Cyclo G6 Glaucoma Laser (Iridex). After a single treatment, pressure was lowered to 11 mm Hg. When we saw him next, I was able to stop one of his bottles and he has maintained the target IOP with a stable visual field for over one year.
Why use MP-TSCPC for this patient? First, there was a need to quickly gain control of the pressure and typically patients have a rapid response to MP-TSCPC. I usually do not alter the settings on the unit (2000 mw, 5 passes per hemisphere, 80 seconds); in cases where I want to achieve a little more pressure lowering – especially in treatment enhancements – I start treatment in the inferior hemisphere, move to the superior and then re-treat the inferior a second time. This process allows me to titrate the treatment without adjusting the settings. The second reason is that the previous trabeculectomy, as well as his frail health, limited the viability of performing a surgery. Needling this filter ran the risk of destabilizing the IOP in a fragile nerve, while longstanding hypotony or IOP elevation might snuff out his optic nerve completely. Moreover, additional medications would likely be unsuccessful if his current regimen was already problematic. Thus, the non-incisional, minimally invasive nature of MP-TSCPC represented a more favorable approach.

Achieving and maintaining the target pressure is the primary objective of treating glaucoma. In the past, adding drops or escalating to surgery were the best options for patients who were out of range. Fortunately, we now have a variety of procedural options that allow us to achieve that goal while also considering quality of life factors, such as the convenience of the treatment and follow-up protocol. As a result, the treatment paradigm for glaucoma has slowly shifted to the point where we can now safely and effectively intervene at earlier stages, with implications for achieving the target pressure sooner while delaying the need for more invasive approaches. Though there are many options for doing so, the unique manner in which laser energy is delivered with the MP-TSCPC procedure results in relatively little destructive effect to the ciliary processes and surrounding tissue, in turn yielding a safe and effective procedure with little post-procedure inflammation. Because of these characteristics, it is widely applicable across a range of glaucoma severity – from mild to wild.

References
- MC Aquino et al., “Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study”, Clin Experiment Ophthalmol, 43, 40 (2015). PMID: 24811050.
- A Tan et al., “Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma”, Clin Experiment Ophthalmol, 38, 266 (2010). PMID: 20447122.
- N Radcliffe et al., “Micropulse transscleral cyclophotocoagulation (mTSCPC) for the treatment of glaucoma using the MicroPulse P3 device”. Presented at: American Glaucoma Society Annual Meeting, San Diego, CA. February 26-March 1, 2015.
- S Kuchar et al., “Treatment outcomes of MicroPulse trans-scleral cyclophotocoagulation in advanced glaucoma”. Presented at: American Glaucoma Society Annual Meeting, San Diego, CA. February 26-March 1, 2015.
