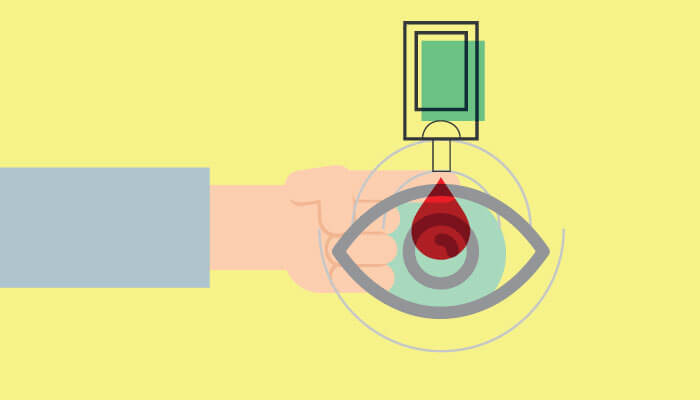
A recent preclinical study by the Diabetes Research Institute (DRI) at the University of Miami Miller School of Medicine has shed new light on islet transplantation for type 1 diabetes. By introducing an anti-CD154/CD40L blocking antibody, researchers found that islets transplanted into the eye survived long-term without continuous immunosuppression – and they also improved peripheral immune tolerance.
The researchers hope the work could unlock the potential of islet transplants for diabetes sufferers – without the downsides of immune suppression. “The best anti-rejection therapy we know of today is generalized – systemic – immune suppression,” says Midhat Abdulreda, Assistant Professor of Surgery and lead author of the study. “Though drug advances have generally improved the survival of solid organ transplants, the side effects of chronic systemic immune suppression, such as cancer formation and stubborn infections that can lead to sepsis, can be life-threatening. This is what we’re trying to eliminate.”
The team split the participating mice into two groups, transplanting islets into the anterior segment of the eye of the experimental group, and into the kidney of the control group – all animals were then treated with CD154/CD40L-blocking antibody.
The results? Both groups experienced immunosuppression-free islet survival of more than 300 days. After 284 days in the kidney group and 412 days in the eye group, the researchers performed a second transplant of islets into the kidney (the kidney group also received a simultaneous nephrectomy to remove the first transplant) to evaluate peripheral immune tolerance. Promisingly, over 70 percent of the eye transplant group experienced more than 400 days survival of the second islet transplant without continued immunosuppression, compared with just 30 percent of those who initially received islets in their kidney.
“Our preclinical studies in animals indicate that, without proper conditioning of the recipient, immune-mediated rejection of islet grafts from mismatched donors will be attacked in the eye. However, our recent findings suggested that conditioning the mouse recipients and a non-human primate (baboon monkey) with a relatively mild and transient immune intervention resulted in significant prolongation in survival of mismatched islet grafts, both in the eye and in the kidney,” explains Dr. Abdulreda. “Our findings also showed a slight advantage of the eye, as a transplant site, in promoting better survival of mismatched islets upon a second transplantation in the same recipients. We don’t fully understand the reasons for this yet, but we believe this makes the eye an attractive site for islet transplant, and worthy of future studies for potential human application.”
Though excited about recent findings, Abdulreda acknowledges that the next step will be more challenging. “We’re currently evaluating the safety and potential efficacy of implanting islets in the eye of legally blind diabetic patients in an FDA-approved clinical trial. This will be critical for future clinical studies building on our preclinical and translational research.”
The team are also planning to evaluate the efficacy of localized immune intervention administered via eye-drops as an alternative to systemic immune suppression.
References
- MH Abdulreda et al., “Operational immune tolerance towards transplanted allogeneic pancreatic islets in mice and a non-human primate”, Diabetologia, Jan 31 [Epub ahead of print] (2019). PMID: 30701283.
