The introduction of minimally invasive glaucoma surgery (MIGS) – the first generation iStent – back in 2008 signaled a big change in the way that we practiced glaucoma surgery and in the outcomes we were witnessing in patient safety and visual recovery. Since then, the MIGS philosophy has become pervasive; devices have been developed for every known target tissue in the aqueous fluid pathway and it feels like we hear about a novel device or new technique every year.
The initial MIGS buzz surrounded internal drainage devices, which allowed us to augment the natural outflow pathways of the eye. Today, surgeons are implanting the second-generation trabecular bypass devices (iStent inject and Hydrus), which have been shown to incrementally improve efficacy while maintaining an excellent safety profile (1).
The supraciliary pathway has garnered a lot of interest, too, but without enjoying the same level of success; several ab-externo devices have failed to progress beyond the clinical trial stage. The recent voluntary recall of Cypass also did this approach no favors. It continues to be a target of interest, though, especially right now with the anticipated release the iStent Supra.
And finally, targeting subconjunctival flow has also generated some excitement, in particular with the release of the XEN gel stent. I will focus the attention of my article on this device, along with some of our recent results using an adaptation of the implantation technique.
More art than science
For more than a century, subconjunctival drainage procedures have remained the cornerstone of glaucoma surgery. Since the introduction of the first guarded filtering procedure in 1968, trabeculectomy has reigned as the time-tested, gold-standard glaucoma surgery. During the ensuing decades, a number of key modifications to the original technique were introduced which further optimized the procedure. For example, adjunctive antimetabolites, such as 5-fluorouracil and mitomycin-C, have improved long-term efficacy, while releasable and laser lysis of sutures improved safety. However, consistent outcomes and the elimination of serious adverse effects have remained elusive, thanks to the complex interplay of patient and surgical factors. Even after the wealth of clinical experience gained during the half-century of performing trabeculectomies, most glaucoma surgeons would agree that it is more an art than a science.
In my opinion, the XEN45 stent brought science to the art of glaucoma surgery by applying the principles of fluid dynamics to its design. A 6-mm long hydrophilic gelatin tube with a 45 µm internal diameter (designed using the Hagen-Poiseuille equation), the stent serves as a channel to drain aqueous fluid from the anterior chamber to the subconjunctival space. Under physiologic conditions, the implant confers a steady state resistance of 6 to 8 mmHg, significantly reducing the risk of hypotony (2). It’s implanted with an ab-interno approach using a preloaded 27-gauge injector system; the absence of conjunctival incisions and sutures virtually eliminates the risk of wound leaks and induced astigmatism. These unique design and delivery characteristics address the common drawbacks associated with trabeculectomy; however, they expose certain vulnerabilities, too.
Design drawback
The length and internal diameter of the stent confer a standardized flow resistance, making early postoperative pressure outcomes highly predictable; however, these outcomes tend to diverge after a few weeks when fibrosis begins to set in during the proliferative phase of healing. Fibrosis is a well-known risk factor for surgical failure in all bleb forming subconjunctival drainage procedures. It turns out the very features that confer the good safety profile of the XEN45 potentially leave it vulnerable to obstruction; it is easier to obstruct a 45 µm opening compared with the filtering perimeter of a trabeculectomy flap. This issue is further magnified when the distal end of the stent becomes entangled in Tenon’s layer. In practice, this is manifested with the significantly high proportion of patients requiring needling after XEN45 and a slight reduction in efficacy compared with trabeculectomy (3).
Trying something different
The surgical technique has evolved extensively though, with the majority of modifications placing the distal tip of the stent more superficially to reduce Tenon’s entanglement and subsequent obstruction. In its original conception, a 2-2-2 placement of the XEN45 stent was recommended – meaning the anterior chamber, intrascleral, and subconjunctival portion were to be equally distributed at 2 mm. Early on, this was modified to a 1-2-3 placement with the goal of traversing the injector further through Tenon’s layer to achieve a more superficial placement. Along the same lines, others have described the “Air XEN” technique4, where air is injected to create a dissection plane separating the conjunctiva from the underlying Tenon’s; the XEN45 is delivered into the “supra-Tenon’s” pocket to ensure a superficial placement.
More recently, a growing number of surgeons have taken to implanting the stent using an ab-externo approach, which has several potential benefits over the traditional ab-interno approach. First, it frees the surgeon from the ergonomic limitations of working through a corneal incision. The outside-in approach expands the option for stent location from superonasal quadrant to the entire superior hemisphere, which is particularly useful if the superonasal tissue has unfavorable conditions, such as pre-existing fibrosis or scleromalacia. Second, an external approach eliminates the requirement for viscoelastic and consequently the possibility of retained viscoelastic occluding the stent in the early postoperative period. Finally, it potentially positions the distal portion of the stent more superficially thereby decreasing the likelihood of the distal stent becoming embedded in the Tenon’s layer.
How do we do it?
Sebastian Gagne has been credited as first describing this technique and several variations have been made since (4). At Wills, we perform ab-externo implantation under topical anesthesia. My preference is to place a corneal traction suture to aid in exposure and counter traction throughout the case. Here’s how I go about it.
Prior to beginning the case, the injector is prepared and the blue slider is advanced to confirm the presence of the implant. Once the implant is visualized, a marking pen is used to highlight the tip of the XEN45 and the conjunctiva is entered at least 7 mm posterior to the limbus. The injector needle is carefully progressed anteriorly through the subconjunctival space taking care to avoid blood vessels to prevent subconjunctival bleeding. The needle enters the sclera approximately 2 mm posterior to the limbus and is tunneled into the anterior chamber. The needle is securely anchored in the sclera, at which point a mirrored gonio lens may be used to confirm proper needle entry. The blue slider is advanced until the previously marked stent tip is visualized in the anterior chamber.
As the injector was designed specifically for ab-interno delivery, the stent will tend to implant longer in the anterior chamber. To avoid this, a blunt tipped forcep may be used to gently grab the implant through the conjunctiva to adjust stent position. An alternative option is to partially deploy the stent until the tip reaches the desired length and then manually retract the needle from the scleral tunnel. Mitomycin-C is injected following stent placement with care being taken to direct the wheel away from the limbus to prevent reflux of antimetabolite into the eye.
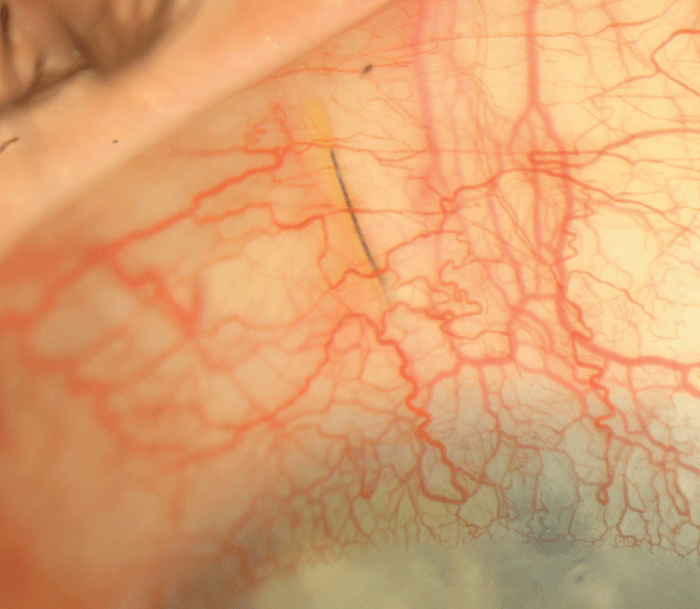
Prior to concluding the case, the final stent placement should be assessed as it could significantly impact outcomes. A posterior placed stent may become occluded by the iris or rub and liberate pigment granules which could occlude the internal lumen (see Figure 2). Therefore, we discourage intraoperative iris manipulation or postoperative laser as iris debris may compromise the stent. Conversely, an anteriorly placed stent carries a theoretical risk of progressive endothelial cell loss. If positioning is in question, the XEN45 should be retrieved (typically ab-interno) and re-implanted.
And the results say…
We recently reported our 12-month, single-surgeon outcomes at the 2020 American Glaucoma Society annual meeting. All surgeries were performed by Jonathan S. Myers with 38 and 23 eyes, respectively, having undergone XEN45 ab-interno and ab-externo implantation (5). Our study demonstrated that, although both approaches had a similar clinical efficacy and safety with no significant difference in IOP, number of medications, or complications, there was a significantly greater need for at least one bleb needling procedure in the ab-interno group compared with the ab-externo group (55 percent vs 13 percent, p < 0.001). This four-fold reduction in postoperative needling supports the claim that ab-externo implantation leads to a more ideal stent position, reducing the need for postoperative manipulation. We now look forward to expanding our analysis to include the remaining members of Wills’ Glaucoma Service.
To be continued
The mastery of subconjunctival glaucoma surgery requires perfect control of both aqueous flow and postoperative fibrosis. I feel that the introduction of the XEN45 was a revolutionary step toward achieving this ideal. In the short few years since it was released, the surgical technique and postoperative management have undergone tremendous evolution, and inventive approaches are continuously being described. Ultimately, a similar leap in fibrosis control is necessary and whether it be sustained release technology or an entirely novel approach, we eagerly await the next revolution.
Disclosures:
Allergan: Consult/Research
Glaukos: Speaker/Research
Optovue: Research
Olleyes: Research
References
- IIK Ahmed et al., “A Prospective Randomized Trial Comparing Hydrus and iStent Microinvasive Glaucoma Surgery Implants for Standalone Treatment of Open-Angle Glaucoma: The COMPARE Study,” Ophthalmology, 127, 52 (2020). PMID: 31034856.
- A Sheybani et al., “Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma,” Invest Ophthalmol Vis Sci, 56, 4789 (2015). PMID: 26218906.
- MB Schlenker et al., “Efficacy, safety, and risk factors for failure of standalone ab interno gelatic microstent implantation versus standalone trabeculectomy,” Ophthalmology, 124, 1579 (2017). PMID: 28601250.
- V Vera et al., “Surgical approaches for implanting XEN gel stent without conjunctival dissection,” Clin Ophthalmol, 14, 2361 (2020). PMI: 32903875.
- RJ Purgert et al., “Outcomes of ab interno versus ab externo XEN gel stent implantation.” Presented at the American Glaucoma Society Annual Meeting; February 27, 2020; Washington, DC, USA.
