The diagnosis of keratoconus is not difficult when clinical signs like corneal ectasia, Vogt’s striae, or Fleischer rings, are present. But not all patients present with these signs – and in their absence, identifying keratoconus is much trickier. There are a number of sophisticated tools that can be used to assist in the diagnosis and staging of the disease; corneal topographers, tomographers, biomechanical assessment devices, and so on. But dedicated, high-tech approaches aren’t the only way to diagnose keratoconus – the humble retinoscope also has a part to play.
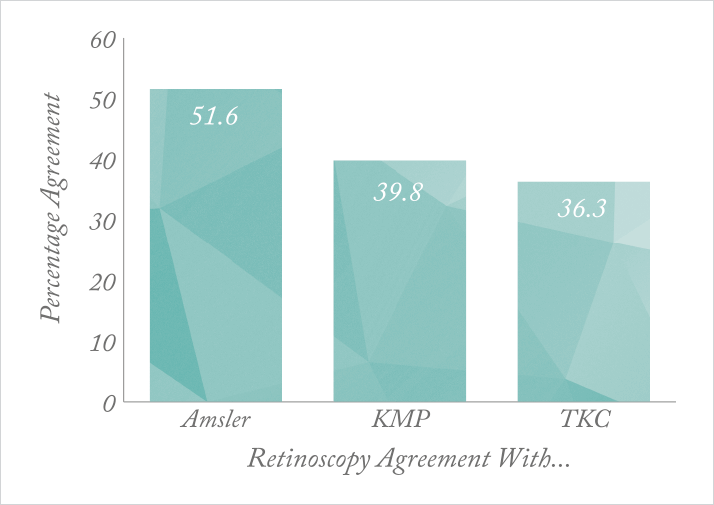
A team of ophthalmologists from Saarland University (Homburg, Germany) compared different techniques for investigating keratoconus (1). They analyzed data obtained by Amsler grading, retinoscopy, topographic keratoconus classification (TKC), and keratoconus match probability (KMP) in 126 patients, classifying their disease into one of five stages from normal to severe. Using descriptive analysis and cross tables, the researchers discovered that the different methods showed significant classification differences when staging keratoconus; Amsler grading agreed with TKC in only 54 percent of cases and with KMP in 48.4 percent, whereas TKC and KMP agreed with one another just 53.3 percent of the time. Retinoscopy was equally incongruent, matching Amsler grading in 51.6 percent of cases, KMP in 39.8 percent, and TKC in only 36.3 percent (see Figure 1). In a binary decision (between normal eyes and keratoconus), the different classification methods performed much better. Retinoscopy agreed with Amsler grading 98.6 percent of the time, KMP 82.4 percent, and TKC 88.8 percent, and featured a sensitivity and specificity of 98.8 and 94 percent, respectively. The team were surprised to find that the various diagnostic techniques – both clinical and instrument-based – were so inconsistent, but the consequences of this discovery are clear. The techniques cannot be used interchangeably, meaning that in longitudinal studies or in disease monitoring over time, trends can only be reported properly if the same classification technique is used at each point in time. The study authors concluded that retinoscopy is no more consistent than any other method, but hasten to add that it has other advantages – for instance, it is easy to use in noncompliant populations such as children or disabled patients, or, as a result of its low cost, in developing regions where expensive instruments are unavailable. However, the researchers raise another key issue in the diagnosis of keratoconus: the need for an international expert committee to define a “gold standard” for classification of the disease.
References
- S Goebels et al., “Can retinoscopy keep up in keratoconus diagnosis?”, Cont Lens Anterior Eye, [Epub ahead of print] (2015). PMID: 25731818.
