Ike K. Ahmed, Ophthalmologist at Prism Eye Institute; Assistant Professor, Fellowship Director, Kensington Eye Institute, University of Toronto; Clinical Professor, University of Utah; Research Director, Kensington Eye Institute, University of Toronto; Co-Medical Director, TLC Mississauga, CanadaDirector, TLC Mississauga, Canada
This information is intended for healthcare professionals.
Traditionally, glaucoma patients are offered surgery only late in the patient journey; eye drops remain first-, second- and third-line therapy! But this years-old paradigm isn’t working; too many glaucoma patients are suffering from quality-of-life issues and vision loss (1), and the impact of topical therapy on patient well-being has made compliance problems ubiquitous. This alone is sufficient reason to replace drops earlier than we typically do. But there is also a cost-effectiveness argument: non-adherence is correlated with disease progression (2), and progression results in more expensive treatments (3). Moreover, drops cannot prevent significant progression in the long-term. Clearly, it’s time to drop the drops and adopt a new, more proactive approach – an approach already supported by innovations in glaucoma management.
The era of interventional glaucoma is here
Accumulating evidence suggests glaucoma is best managed when managed proactively: early, aggressive intervention can reduce IOP in a sustainable, predictable way. Remember, each mmHg reduction reduces progression risk by up to 10 percent (4); keeping pressure below 15 mmHg significantly reduces progression risk even in early glaucoma (5), and early control gives better long-term preservation of vision (6). The traditional paradigm should be replaced by a new approach (see Box: Interventional glaucoma).
We must stop judging earlier surgery by the outcomes of late procedures that give less predictable results and more complications than earlier intervention. The data show that for patients with moderate glaucoma it can help control pressure effectively, and sustained low IOP reduces risk of visual field progression (moderate glaucoma, IOP surgically controlled at ~12 mmHg) (7). Patients who maintain pressures of 13 mmHg or less show an improvement in the visual field (8), and primary surgery lowers IOP better than primary medication (9). Overall, early surgery gives better visual field preservation, lower progression risk, lower peak IOPs, reduced pressure fluctuations, elimination of adherence issues, and improved quality of life – and may be less costly, long-term, than drops.
Interventional glaucoma: a new mindset for a new era
• Be more proactive and aggressive from the start
• Aim to get IOP lower, earlier
• Consider early trabeculoplasty, MIGS, and novel glaucoma drainage devices
• Achieve protection by sustaining IOP reduction
• Consider combination cataract surgery
• Balance compliance and risks with more aggressive therapy
• Address adherence; future options include sustained release drug delivery and MIGS synergy
Which intervention to use?
Trabeculectomy is still the gold standard for patients who need very low pressures, but for other patients we have many options. Development-stage products include surface implants, gel-forming drops, punctal plugs, intrascleral implants, intracameral implants, injectable drugs, and subconjunctival implants (10, 11, 12, 13); in addition, we have excellent surgical options available right now. Which one to use? Factors to consider include: safety, efficacy, post-operative management intensity, ease of use, speed of visual recovery, cost, patient age, possibility of combining with cataract surgery, disease severity, target IOP, and medication tolerance. Although no two patients are the same, we can often assign them into provisional categories (see Box How does Ike Ahmed categorize his patients?).
What about outcomes? A comparison of selective laser trabeculoplasty with medical therapy as first-line therapy in earlystage glaucoma patients showed that the surgery achieved good IOP control without medication; note that eleven patients required trabeculectomy in the medication group versus zero in the trabeculoplasty group (14). In many patients, however, a MIGS procedure may be a better choice; these address physiologic outflow safely (and with fast recovery) in early-stage patients, and (even with only ~2 mmHg reduction) reduce medication burden (15). Thus, Schlemm’s canal stent plus phaco reduces risk of secondary surgical intervention at two years by 60 percent versus phaco alone (16). Rather than firstline trabeculectomy, we should consider less invasive, more standardized stenting procedures – notably the subconjunctival MIGS – or micro-invasive bleb procedures. For example, XEN® and PRESERFLO™ MicroShunt blend advantages of both MIGS and trabeculectomy, avoiding hypotony while reducing pressure to acceptable levels. Indeed, XEN® has Kaplan-Meier success curves similar to those of trabeculectomy (but requires significantly more needlings and revisions) (17, 18).
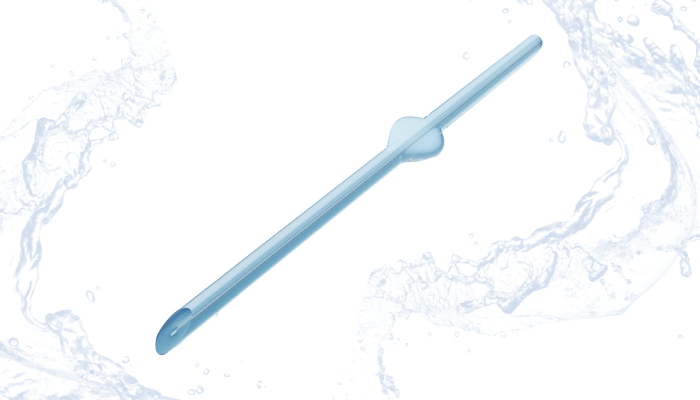
PRESERFLO™ MicroShunt (see Box PRESERFLO™ MicroShunt: A material advantage) is particularly potent: it consistently reduces IOP to 12 or 13 mmHg, requires minimal post-operative management, and usually reduces medications to zero (19). These kinds of results are seen even in refractory glaucoma patients who have had previous surgery (20). Overall, PRESERFLO™ MicroShunt patients have a more rapid and more complete visual recovery than is normal for bleb surgery.
How does Ike Ahmed categorize his patients?
• Those requiring combination with cataract surgery (consider MIGS)
• Those requiring standalone surgery with an IOP target in the mid-high teens (consider a large trabeculotomy ab interno)
• Those requiring standalone surgery with an IOP target of 12 mmHg (typical approach: minimally invasive bleb surgery)
• Those requiring standalone surgery, IOP target <10 mmHg (typical approach: trabeculectomy)
PRESERFLO™ MicroShunt: A material advantage
• Many surgical devices are made from polyurethane or silicone rubber – unstable compounds that can degrade and cause chronic inflammation (21)
• PRESERFLO™ MicroShunt is fabricated from SIBS – poly(styrene-b-isobutyleneb-styrene) – an innovative polymer with a number of advantages (21, 22, 23)
• In particular, when compared with standard devices, ocular implants made from SIBS are associated with less inflammation and with dramatic reductions in myofibroblast numbers and in the thickness of the pseudo capsule surrounding the implant (24)
• Thus, SIBS devices help address one of the biggest challenges in glaucoma surgery – wound and tissue healing
The new era starts now
We are now entering the age of interventional glaucoma; we must respond proactively to uncontrolled disease. Escalating topical therapy is not the answer – it achieves little more than increased toxicity and lower adherence (25, 26). We must remember the many years that our patients have to live with glaucoma, intervening aggressively with safe options that do not preclude future options. A variety of procedures are available – not least PRESERFLO™ MicroShunt, which predictably and consistently achieves IOPs of <15 mmHg with minimal post-operative management (27).
Ike K. Ahmed is a consultant and speaker for Santen.
References
- S Remo et al., Trans Vis Sci Tech, 4, 1 (2015). PMID: 25767744.
- P Newman-Casey et al., Ophthalmology, 127, 477 (2020). PMID: 31932093.
- C Traverso et al., Br J Ophthalmol, 89, 1245 (2005). PMID: 16170109
- MC Leske et al., Arch Ophthalmol, 121, 48 (2003). PMID: 12523884.
- B Chauhan et al., Arch Ophthalmol, 126, 1030 (2008). PMID: 18695095.
- J Caprioli, Am J Ophthalmol, 145, 191 (2008). PMID: 18222187.
- AGIS Investigators, Am J Ophthalmol, 130, 429 (2000). PMID: 11024415.
- D Musch et al., Am J Ophthalmol, 158, 96 (2014). PMID: 24727262.
- J Burr et al., Cochrane Database of Systematic Reviews (2012). PMID: 22972069.
- JD Brandt et al., Ophthalmology, 124, 1565 (2017). PMID: 28528010.
- AA Al-Kinani et al., Adv Drug Deliv Rev, 126, 113 (2018). PMID: 29288733.
- M Chen, SY Choi, Med Hypothesis Discov Innov Ophthalmol, 9, 56 (2020). PMID: 31976344.
- N P Kesav et al., Int J Ophthalmol, 14, 148 (2021). PMID: 33469497.
- G Gazzard et al., Lancet, 393, 1505 (2019). PMID: 30862377.
- H Saheb and I Ahmed, Curr Opin Ophthalmol 23, 95 (2012). PMID: 22249233.
- T Samuelson et al., Ophthalmology, 126, 29 (2019). PMID: 29945799.
- M Schlenker et al., Ophthalmol Glaucoma, 1, 189 (2018). PMID: 32672652.
- M Schlenker et al., Ophthalmology, 124, 1579 (2017). PMID: 28601250.
- M Schlenker et al., Am J Ophthalmol, 215, 141 (2020). PMID: 32173344.
- G Durr et al., Br J Ophthalmol (2020). PMID: 33097520.
- L Pinchuk et al., Biomaterials, 29, 448 (2008). PMID: 17980425.
- L Pinchuk et al., Regen Biomater, 3, 137 (2016). PMID: 27047682.
- L Pinchuk et al., “J Biomed Mater Res Appl Biomater, 105, 211 (2017). PMID: 26380916.
- A Acosta et al., Arch Ophthalmol, 124, 1742 (2006). PMID: 17159034.
- C Valente et al., J Ocul Pharmacol Ther, 27, 281 (2011). PMID: 21557633.
- A Robin, DS Grover, Indian J Ophthalmol, 59, S93 (2011). PMID: 21150041.
- JF Batlle et al., J Glaucoma, [Online ahead of print] (2020). PMID: 33137019.
