
Did you know rates of glaucoma are four or five times higher in African Americans? At my practice, in Harlem, New York City, US, an area with a heavy African American population, the cases of glaucoma that present to us are often advanced – -7/-8 DB visual field loss is not uncommon. Unfortunately, in these more advanced patients, eyedrops are less successful as a first line treatment, so my practice has evolved to doing earlier, safer, more aggressive therapies, including earlier cataract surgery and Schlemm’s canal surgery.
The reasons African Americans suffer higher rates are complex, but can essentially be attributed to hundreds of years of decreased access to care. Legally, Black people were not allowed to read or write for many years. Only as recently as the 1960s were schools integrating, allowing Black people to go to medical school to become surgeons. And even today, the US only has around 400 African American ophthalmologists. With many residential communities in the US remaining segregated, ophthalmologists often end up practicing in their own racial communities, leaving Black communities with limited options. Decreased access to treatment means many African Americans need earlier intervention – namely, earlier microinvasive trabecular bypass surgery – to bend the curve of blindness, which is what I have been doing in my practice.
We’ve published papers looking at surgery as a safe, efficacious initial treatment – and we’ve had excellent results with patients in our practice. It is worth remembering that glaucoma medication is expensive – US$30–50 for prostaglandins and newer combination medications. For some patients, this means having to make a decision between buying food and taking medications; it’s no wonder some people don’t go to the ophthalmologist at all. Finding another way to lower pressure, improve compliance, and reduce the need for expensive medications would go a long way to reducing this healthcare disparity.
In ophthalmology, we generally make a point of not operating until “necessary” – preferring to treat patients with eyedrops and lasers. This mindset is partly due to the fact that surgical skills are not uniformly distributed, which will prove challenging as the future of glaucoma moves towards earlier surgical intervention. We need to train the next generation of surgeons to be experts in cataract and angle-surgery so they can perform them seamlessly. Cataract surgery is far safer today than it was 20 years ago – and this offers tremendous pressure lowering benefits particularly in combination with microinvasive glaucoma surgery. Trabeculectomy remains the standard of care for surgical glaucoma, despite it having more complications and carrying the potential of losing the patient up to two lines of vision. In glaucoma patients whom receive earlier cataract surgery/lensectomy and microinvasive glaucoma surgery will not need medications nor trabeculectomy.
In my practice, we take a different approach. We have found that in patients over 50 years of age, the cataract – or enlarged lens – is the most common identifiable cause of glaucoma. Trabecular meshwork obstruction and obstruction of Schlemm’s canal have an impact on aqueous drainage. Schlemm’s canal is compressed by the enlarged lens. The enlarged lens, creates pigment liberation by rubbing against the posterior iris and the pigment becomes trapped in the trabecular meshwork, which further reduces flow and elevates eye pressure. Eye drops do not address this mechanism but only lowers the pressure and can worsen cataract formation.
In the Baltimore Eye Survey, a study investigating the relationship between intraocular pressure and primary open angle glaucoma among White and Black Americans, the mean normal intraocular pressure in individuals without glaucoma was approximately 15 mmHg and the mean intraocular pressure in patients with untreated glaucoma is 18 mmHg (1). For glaucoma patients with age related cataract, it is essential to perform gonioscopy to identify increased pigment deposition, narrowing of the angle, and compression of the angle structures to identify suitable candidates for potential earlier combination cataract surgery/lensectomy and MIGS glaucoma surgery.

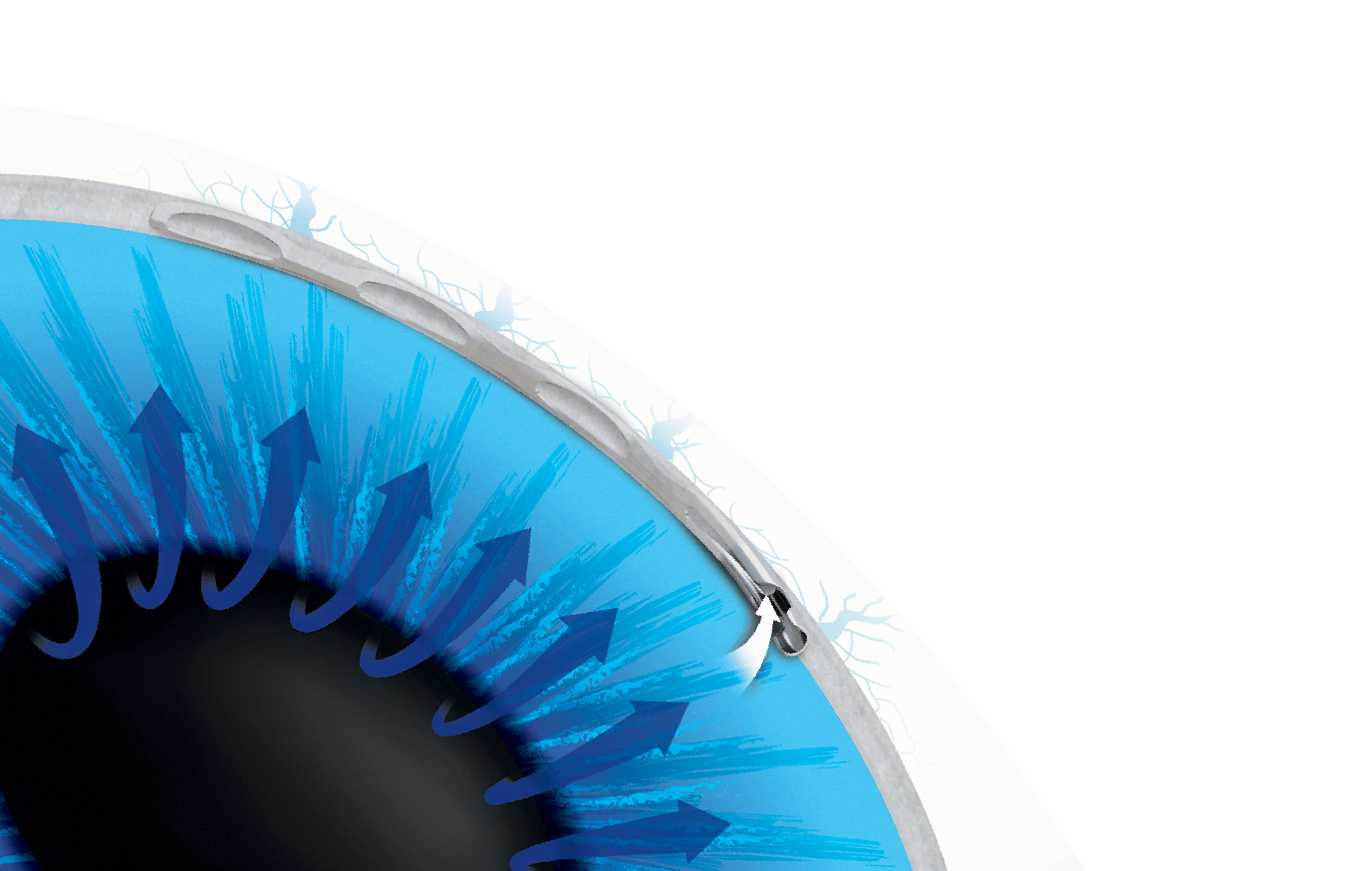
Several randomized clinical studies have shown IOP lowering associated with cataract surgery alone in patients with open angle glaucoma. The addition of a Schlemm’s canal based MIGS device can lower IOP even further without changing the safety profile of the procedure. I currently offer patients initial treatment for glaucoma with cataract surgery and the Hydrus Microstent as we know removal of the cataract opens Schlemm’s canal and expands the trabecular meshwork. The Hydrus Microstent further enhances aqueous outflow through three mechanisms of action: trabecular meshwork bypass, expansion of Schlemm’s canal, and greater access to collector channels (see Figure 2). The bypass feature eliminates resistance to aqueous flow related to the effects of material build up in the trabecular meshwork, while the expansion of the canal over three clock hours of the circumference of the eye allows for optimal access to multiple collector channels.
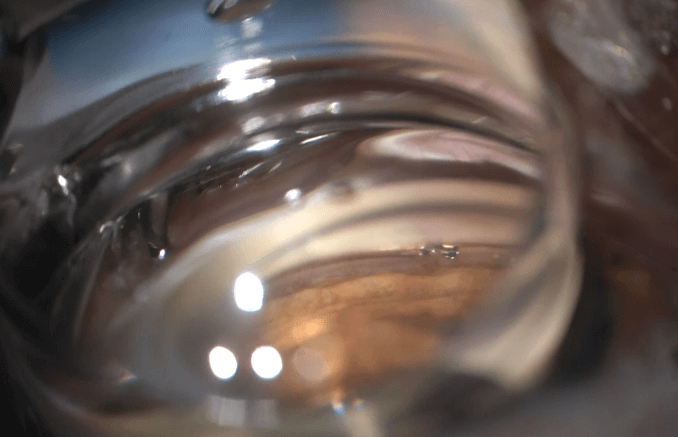
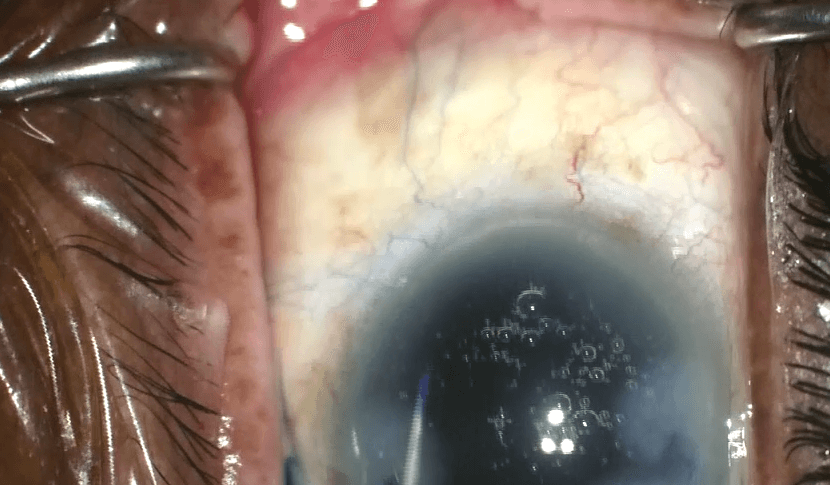
Despite its complex design, the Hydrus Microstent is approximately the size of an eyelash – small enough that it is typically never felt or seen by the patient (see Figure 3). I believe this initial uncomplicated surgical treatment addresses the cause for glaucoma and safely provides the most effective solution currently.

Inserting the Hydrus is an elegant procedure. It is easy to confirm by visual inspection that you are in the right place (see Figure 4). Canal stenting with Hydrus leads to a robust outflow of aqueous to the veins for several clock hours, as may be confirmed. The aqueous veins may be blanched with BSS using the phaco tip. I also use it in advanced glaucoma patients who have not had glaucoma surgery – with very good results.
Two prospective, multicenter, randomized controlled trials supporting the safety and effectiveness of the device have been published in Ophthalmology (2, 3). In the HORIZON trial, the largest MIGS randomized study conducted to date, the Hydrus demonstrated significant reduction of IOP and medications in a wash out comparison for two years postoperatively. As presented at the recent American Society of Cataract and Refractive Surgery meeting, three-year follow-up has shown that intraocular pressure reductions are maintained, with 73 percent of eyes in the Hydrus group remaining medication-free, with a safety profile similar to phacoemulsification alone, and no significant change in endothelial counts. Additionally, compared with phaco alone, Hydrus with phaco reduced the risk of incisional glaucoma surgery by 80 percent during the follow-up period.
In our published series in Black patients, 74 percent of our patients were medication free at six months – important, as I have mentioned before, considering the financial burden drops put on patients from lower socioeconomic statuses. There was also significant improvement in visual acuity and stabilization of mean deviation on visual field test (baseline -9.2; 6 months -9.1; p = 0.22). In my experience, the Hydrus Microstent is the most powerful MIGS device that can be placed in patients with mild to moderate glaucoma at the time of cataract surgery. Even better, there are no serious risks or complications associated with the procedure. The second generation iStent Inject has been problematic in my hands. At times, it has not been able to penetrate a thickened heavily pigmented trabecular meshwork, or conversely penetrated through both the inner and outer wall of the Schlemm’s canal, becoming implanted into the sclera, reducing its efficacy. This has been confirmed by others with AS-OCT imaging of iStent (5). Neither has the Xen subconjunctival stent been foolproof in that the 45 μm small lumen can become obstructed subconjunctivally or intraluminally – an obstruction that cannot be overcome with needling or external revision.
Cataract surgery and implanting the Hydrus Microstent at an earlier stage will often serve to preserve the health of the patient’s collector channel and provide benefit from the beginning to the end of the disease. Having performed over 2,500 of these procedures in patients with glaucoma, not only can I lower the intraocular pressure and dramatically reduce the number of medications needed, but also improve vision from cataract extraction and refractive lens exchange.
We have a responsibility to educate our Black glaucoma patients not only about the need to get checked, but also to inform them about the new surgical treatments available to them – and that should include earlier cataract surgery and Hydrus Microstent. Finally, to clarify, I’ve shared here my initial approach to patients with open angle and angle closure glaucoma over the age of 50, but this does not apply to patients with other types of secondary glaucoma, such a neovascular or uveitic glaucoma. This approach should only be used by skilled experienced surgeons able to regularly provide uncomplicated surgery.
References
- A Harry et al., “Relationship Between Intraocular Pressure and Primary Open Angle Glaucoma Among White and Black Americans: The Baltimore Eye Survey,” Arch Ophthalmol 109, 1090 (1999). PMID: 1867550.
- N Pfeiffer et al., “A randomized trial of a Schlemm’s canal microstent with phacoemulsification for reducing intraocular pressure in open-angle glaucoma,” Ophthalmology, 122, 1283 (2015). PMID: 25972254.
- T Samuelson et al., “HORIZON Investigators. A Schlemm Canal Microstent for Intraocular Pressure Reduction in Primary Open-Angle Glaucoma and Cataract: The HORIZON Study,” Ophthalmology, 126, 29 (2019). PMID: 29945799.
- I Ahmed et al., “COMPARE Investigators. A prospective randomized trial comparing Hydrus and iStent micro-invasive glaucoma surgery implants for standalone treatment of open-angle glaucoma: The COMPARE Study,” Ophthalmology, [Epub ahead of print] (2019). PMID: 31034856.
- K Gillmann et al., “A Prospective Analysis of iStent Inject Microstent Positioning: Schlemm’s Canal Dilatation and Intraocular Pressure Correlations,” J Glaucoma, 28, 613 (2020). PMID: 31058666.
- D Laroche et al., “Real-world efficacy of the Hydrus microstent in Black and Afro-Latinx patients with glaucoma: a retrospective study,” Ther Adv Ophthalmol, 19, 2515841420964311 (2020). PMID: 33150299.
