Spheres of Influence
Could little balls of hydroxyapatite be the initiator of drusen formation?
One hallmark of the aging retina is the accumulation of sub-retinal pigment epithelium (RPE) deposits of proteins and lipids. If clumped together, they’re known as drusen, if diffuse, they’re referred to as basal laminar deposits. But irrespective of their nomenclature, they’re believed to be involved in the pathogenesis of age-related macular degeneration – (AMD) as impaired metabolic exchange between the choroid and the retina, ultimately damages the latter structure. But what initiates their formation? What keeps them in Bruch’s membrane? A team of researchers based in the US, UK and Germany may have the answer: hydroxyapatite (bone mineral) spherules (1).
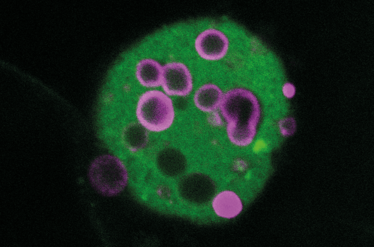
Figure 1. Hydroxyapatite spherules, stained with Bone-Tag 680RD (magenta), as revealed by confocal microscopy. (I. Lengyel, University College London)
Richard Thompson, associate professor of biochemistry at the University of Maryland, and the study’s first author, explained how they came to that conclusion: “Imre Lengyel and his colleagues were examining the composition of the sub-RPE deposits taken from human cadaver eyes. X-ray diffraction indicated the presence of the bone mineral hydroxyapatite, and we found that a diverse group of fluorescent dyes – some of which were developed as bone stains – could selectively stain it. Striking confocal fluorescence micrographs of the stained drusen revealed the remarkable spherular morphology of hydroxyapatite,” said Thompson (see Figure 1).
Lengyel’s colleagues at University College London demonstrated that hydroxyapatite “can provide a scaffold for common drusen proteins like complement factor H and vitronectin, and therefore may be a catalyst for drusen development – and ultimately, AMD”. According to Thompson, his collaborators at the University of Tübingen “analyzed which RPE-secreted proteins adhere to hydroxyapatite by using a combination of stable isotope labeling by amino acids in cell culture (SILAC), followed by secondary ion mass spectrometry,” and at Imperial College London “created a high-resolution map of the molecular constituents of the spherules in drusen, also using sophisticated mass spectrometric techniques.”
“The presence of calcium phosphate precipitates in the aging retina and other tissues was known, but we didn’t expect to find hydroxyapatite in the deposits themselves because it is much harder, more chemically stable, and has lower solubility than ordinary dibasic calcium phosphate – hence its vital role in bones and teeth,” explained Thompson, before adding, “We were also surprised by the (mainly) hollow, near-perfect spheres that the HAP formed.”
The research should have an almost immediate clinical impact: “Our preliminary data suggest it will likely be possible to fluorescently label and image spherules in the living retina with a fluorescence ophthalmoscope, which will lead to earlier identification of people who will go on to develop AMD, prompting earlier treatment. We also plan to explore new treatments which focus on preventing hydroxyapatite development and hopefully, AMD progression”.
- RB Thompson et al., “Identification of hydroxyapatite spherules provides new insight into subretinal pigment epithelial deposit formation in the aging eye”, Proc Natl Acad Sci U.S.A., Epub ahead of print (2015). PMID: 25605911.
I have an extensive academic background in the life sciences, having studied forensic biology and human medical genetics in my time at Strathclyde and Glasgow Universities. My research, data presentation and bioinformatics skills plus my ‘wet lab’ experience have been a superb grounding for my role as a deputy editor at Texere Publishing. The job allows me to utilize my hard-learned academic skills and experience in my current position within an exciting and contemporary publishing company.