All ophthalmologists were compensated by Glaukos for their time during the webinar.
A recent round-table of six glaucoma experts discuss how adopting the “interventional glaucoma mindset” could potentially revolutionize the future of glaucoma treatment and care.
Chairing the event, The Ophthalmologist 2024 Power Lister and President of The Eye Centers of Racine & Kenosha in Wisconsin, Inder Paul Singh, began by asking the gathered surgeons what they were most excited about in the current glaucoma space. Ophthalmology Section Chief at Broadlawns Medical Center in Des Moines, Iowa, Christy Benson, was looking forward to the prospect of “spending more time in the OR,” due to glaucoma now “becoming a more procedural based disease, as opposed to a medical disease.” Deborah Ristvedt, an ophthalmologist specializing in advanced cataract surgery, minimally invasive glaucoma surgery, and oculoplastic procedures at Vance Thompson Vision, Minnesota, noted the “beautiful potential to individualize patient care” that early intervention presented.
Alex Gerber, an ophthalmologist specializing in cataract surgery, LASIK, and minimally invasive glaucoma surgery, as well as serving as Medical Director of Koch Lasik and Aesthetics, Rhode Island, said quite simply that he was excited about “using less eye drops” on patients. Singh added that eye drops can greatly impact patient compliance: “Those who are on drops have more progression compared to those with SLT [selective laser trabeculoplasty].” (1)
Mehul Nagarsheth, an ophthalmologist at Eye Consultants of Pennsylvania who specializes in glaucoma and cataract surgery, was quick to point out that many studies have shown the efficacy and safety profile of SLT. (1) However, he added that it was still important to give patients a full list of options. This prompted Singh to then ask, that if, for example, procedural pharmaceuticals or SLT really were the best things for the patients, should surgeons even be giving them these other options?
Ophthalmologist at Omni Eye Services of Atlanta, Georgia, and specialist in comprehensive glaucoma treatments and advanced cataract surgery, Arkadiy Yadgarov, suggested that, prior to the three-year data from the LiGHT trial (1), patients should have been given all the options. However, “the LiGHT trial really changed everything for me from an interventional mindset, he explained. “The data is right there in front of you and it speaks loudly that SLT long-term is better than eye drops, [so] unless there’s a contraindication of any sort, there’s no reason I wouldn't first offer SLT as a first-line therapy.”
Success and iStent infinite®
Interventional glaucoma is a proactive approach to managing glaucoma that entails early predictive diagnostics, active monitoring, and intervention of procedures earlier in the treatment paradigm. These interventions, which can provide an alternative to traditional surgery and offer a less invasive approach to preventing vision loss, can provide a safer and more effective option for managing intraocular pressure (IOP) in glaucoma patients.
And while experts are increasingly convinced about the success of interventional glaucoma treatment, what does success actually mean for the patients involved?
For Nagarsheth, it simply means that the patient is happy and can see well. Risvedt, meanwhile, added that it was crucial to look at the data gathered from previous trials to indicate success points of devices on the market. “In a study of 50 patients using standalone iStent infinite®, the patients’ mean IOP prior to surgery was around 17; these were mild, moderate and severe glaucoma patients who had failed prior medical and surgical intervention,” she explained. “Afterwards, the majority of these patients were on zero medications. (2) That's just a win for quality of life, for economic burden, and patients knowing that their vision is better. And so [I would say that] success is also about quality of life.”
With regard to the iStent infinite® specifically – an implantable MIGS device intended to lower intraocular pressure (IOP) for primary open-angle glaucoma (POAG) patients who have failed medical and surgical intervention. Singh was curious to learn more about the group’s experiences with this technology. Benson, who took part in the launch of iStent infinite® in the Midwest, said she’s had “really fantastic results from day one.” She continued, “Success is different for each patient, and that's the big thing with interventional glaucoma: it's tailored to each patient. The goals are individualized, and so what success means for one patient is different for another.”

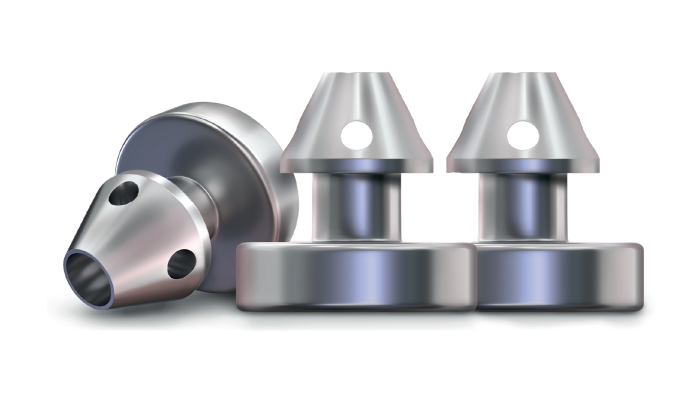
Gerber, an early adopter of iStent infinite®, observed that “the injector system is elegant and straightforward.” For Yadgarov, the iStent infinite® platform “is really a home run – it's extremely versatile, has a great safety profile, and as soon as a surgeon uses one or two, they'll realize that it’s also very intuitive.”
Next up on the agenda was how the surgeons could educate their colleagues on the benefits of iStent infinite®. Yadgarov said he would simply recommend that a surgeon give the implant an initial try and “just see what it does to your patients, how happy they are,” and how it improves their overall quality of life. Risvedt questioned the motives of surgeons not taking on the procedure, given the evidence of its benefits. For her, there are three questions to ask about a surgeon’s potential reluctance to use the implant. “One – are they on the fence because of their confidence? Two – are they skeptical about the technology (even though we have 300+ peer reviewed articles demonstrating efficacy with iStent technologies)? And three – if this was a surgeon’s own family member, then what would they recommend?” Can we “get them off of the fence by thinking in those terms?” she added.

Stents are approximately 360 μm in diameter and 360 μm in height
Changing the paradigm
Wrapping up the lively discussion, Singh acknowledged that, as a surgeon, “it's easy to get complacent” when everything is working in your practice. “But when you go out into the wider world, you realize there's so many ways of doing things, and there's such a high potential for us to further improve a patient’s quality of life. The earlier we intervene, the more we can change the existing paradigms one patient at a time.”
At this next stage of standalone MIGS, it all “just depends on our mindset,” Singh added, noting that surgeons can sometimes be their own barriers, bestowing their own personal fears onto their patients. “So,” he concluded, “trust yourself, and your colleagues, because there's so many potential patients we can help to save from going blind by adopting interventional glaucoma.”
The physicians who participated in this program were compensated by Glaukos for their time.
PM-US-2268
INDICATION FOR USE. The iStent infinite® Trabecular Micro-Bypass System Model iS3 is an implantable device intended to reduce the intraocular pressure (IOP) of the eye. It is indicated for use in adult patients with primary open-angle glaucoma in whom previous medical and surgical treatment has failed. CONTRAINDICATIONS. The iStent infinite is contraindicated in eyes with angle-closure glaucoma where the angle has not been surgically opened, acute traumatic, malignant, active uveitic, or active neovascular glaucoma, discernible congenital anomalies of the anterior chamber (AC) angle, retrobulbar tumor, thyroid eye disease, or Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS. Gonioscopy should be performed prior to surgery to exclude congenital anomalies of the angle, PAS, rubeosis, or conditions that would prohibit adequate visualization that could lead to improper placement of the stent and pose a hazard. MRI INFORMATION. The iStent infinite is MR-Conditional, i.e., the device is safe for use in a specified MR environment under specified conditions; please see Directions for Use (DFU) label for details. PRECAUTIONS. The surgeon should monitor the patient postoperatively for proper maintenance of IOP. Three out of 61 participants (4.9%) in the pivotal clinical trial were phakic. Therefore, there is insufficient evidence to determine whether the clinical performance of the device may be different in those who are phakic versus in those who are pseudophakic. ADVERSE EVENTS. The most common postoperative adverse events reported in the iStent infinite pivotal trial included IOP increase ≥ 10 mmHg vs. baseline IOP (8.2%), loss of BSCVA ≥ 2 lines (11.5%), ocular surface disease (11.5%), perioperative inflammation (6.6%) and visual field loss ≥ 2.5 dB (6.6%). CAUTION: Federal law restricts this device to sale by, or on the order of, a physician. Please see DFU for a complete list of contraindications, warnings, precautions, and adverse events.
References
- G Gazzard et al., “Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial: Six-Year Results of Primary Selective Laser Trabeculoplasty versus Eye Drops for the Treatment of Glaucoma and Ocular Hypertension,” Ophthalmology, 130, 139 (2023). PMID: 36122660.
- D Ristvedt, “Third-Generation Trabecular Micro-Bypass in Eyes Failing Prior Surgical and/or Medical Glaucoma Therapy,” Poster at the Annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS) meeting. April 5-8, 2024: Boston, MA, USA.
