
Dr Michael Mikhail
Back in 2022 I had the chance to move from the UK and set up as a consultant ophthalmologist and vitreoretinal surgeon in Rwanda. Upon arrival in the country, I quickly realized that my skills were in high demand: there was only one vitreoretinal (VR) surgeon accounting for a population close to 15 million, and Rwanda's leading eye care institution, Kabgayi Eye Unit (KEU), had been without a full-time VR surgeon for over two years, relying on sporadic visits from visiting surgeons to manage a growing backlog of cases.
Aggravating this backlog was an increasingly high number of premature babies who had survived but were now suffering from bilateral blindness due to tractional retinal detachment. My exposure to pediatric retina in the UK was limited to retinal detachments from dialysis or atrophic holes, for which I would typically perform scleral buckle procedures. After Dr. Chien Wong, the leading retinopathy of prematurity (ROP) expert in the UK, visited Rwanda and we operated together, I gradually developed the skills to manage complex ROP cases. This mentorship was crucial in my journey to help these children and their families.
Building local capacity
Kabgayi Eye Unit is dedicated to enhancing ROP treatment and management. We concentrate our efforts on initiating awareness campaigns, training ophthalmic technicians in screening procedures, and educating pediatricians on the importance of early detection and timely referral. So far, this collective effort has resulted in a significant increase in weekly referrals for screening and, more importantly, a decrease in children presenting with advanced ROP requiring surgery.
My pediatric surgery list is typically scheduled on Wednesdays, where we handle three to four infants. These cases include examinations under anesthesia (EUA) for new or follow-up patients. For stage 4 ROP, we perform sequential bilateral lens-sparing vitrectomies (LSV), treating each eye as a separate procedure with new instruments for each. We have achieved a zero endophthalmitis rate in bilateral cases. For stage 5 ROP, I operate on one eye at a time.
Key surgical lessons from ROP surgery
I’d like to share my approach to these cases, summarizing some key points:
A pediatric eye is not simply a smaller version of an adult eye. The anatomy of pediatric eyes is unique, with its own set of rules and techniques. For instance, the crystalline lens is comparatively large and more spherical, the pars plana remains underdeveloped until around eight to nine months of age, and the sclera is thinner and more elastic. Additionally, the vitreous in these eyes is well-formed and typically has strong adhesions to the retina.
Zero-tolerance of complications. We maintain a zero-tolerance approach to complications as even a single retinal break can lead to catastrophic failure, resulting in total retinal detachment and eventual phthisis. Similarly, during LSV we take extreme care to avoid any lens injury. This requires careful precision at each step to prevent complications and ensure optimal surgical outcomes.
Common misconceptions. The first misconception is that for macula-sparing retinal detachment (stage 4A), surgery can be delayed until the macula is detached. In my experience, prompt intervention is crucial as it offers the best chance for visual normalization. The second misconception is that surgery for stage 5 ROP is not worthwhile. My experience shows that while the prognosis is typically poor for these cases, surgery in open funnel cases can preserve light perception, enabling children to distinguish between day and night. This ability is vital for their quality of life.
Examination Under Anaesthesia (EUA). During the EUA session, we capture baseline color images using a digital wide-field fundus camera, followed by fluorescein angiography (FFA) to assess ischemia and vessel growth. If laser photocoagulation is required, we opt for retinal argon laser treatment using an indirect ophthalmoscope. This approach reduces the time spent inside the eye and minimizes unnecessary traction on the vitreous base from moving the endolaser probe in eyes with a well-formed vitreous.
Surgical aims. In stage 4A, preservation of the lens and total retinal reattachment is the goal. In stage 4B/5, the practical surgical goal is to reattach as much of the retina as possible without causing a retinal break. Partial residual detachment and retinal folds are common in such eyes, and should not be regarded as failure.
Planning vitrectomy ports placement. In stage 4B ROP, traditional vitrectomy port placement can be risky as the temporal retina may retract into the retrolental space. If this is observed during EUA, I adjust by positioning myself on the nasal side of the eye. The infusion line is placed horizontally between the supero-nasal and infero-nasal ports, and we proceed with standard LSV technique to protect the temporal retina.
Stage 4 ROP. Aiming for LSV, we begin with a partial conjunctival peritomy, primarily to facilitate suture closure at the end of the case. Port placement is determined by the patient's age, with a simple rule of thumb being 1 mm from the limbus for each year of age (e.g., for a 2-year-old child, the ports would be inserted 2 mm from the limbus). This continues until the child is 4 years old, at which point 4 mm from the limbus becomes the standard, as in adults. I insert the ports perpendicular to the iris plane rather than directing them towards the center of the eye.
We typically use a 23-gauge transconjunctival vitrectomy system. While performing the core vitrectomy, we pay close attention to the vectors of traction, aiming to cut the connections that create traction—whether it's from ridge to ridge, ridge to the periphery, ridge to the lens, or ridge to the optic nerve head. Often, the release of traction intraoperatively can be seen by the relaxation of the tented retina. We avoid inducing a posterior vitreous detachment (PVD) in these cases. Once the dissection is complete, we perform a partial air-fluid exchange to prevent vitreous incarceration.
Our standard operating time per eye is typically around 20 minutes from start to finish. This involves careful planning pre-surgery and during surgery. Prior to surgery, detailed examination under anesthesia is performed to plan port placements. During surgery, surgical goals are well defined with relief of main tractional vectors being the key. Complete vitrectomy (including PVD induction) is not the goal and would increase the risk of surgery.
The subretinal fluid and traction RD is expected to reabsorb gradually over the following weeks to months. A key indicator of surgical success is the absence of disease progression.
Stage 5 ROP. The learning curve is steeper for stage 5 ROP cases, where the retina is complexly detached due to traction forces involving the peripheral retina and ciliary body. My main goal is to release as much traction as possible, particularly in the central region, while avoiding iatrogenic retinal breaks.
We perform limbal vitrectomy with lensectomy, including the lens capsule, to access the retrolental fibrous tissue. Using a bimanual approach with retinal forceps, scissors, and a vitreous cutter, we dissect the retrolental membrane. We limit extensive dissection in the far periphery, as sometimes differentiating between thin membranes and avascular retina can be challenging. Additionally, traction on the peripheral retina must be handled cautiously to avoid retinal disinsertion. A critical concept is that maximizing the chances of retinal reattachment relies on thorough membrane removal; however, this must not come at the expense of causing iatrogenic retinal breaks.
In cases with anterior segment changes, like posterior synechiae, we may use iris hooks or make iris incisions for adequate pupillary dilation. After completing the procedure, we close all ports with Nylon 10/0 suture.
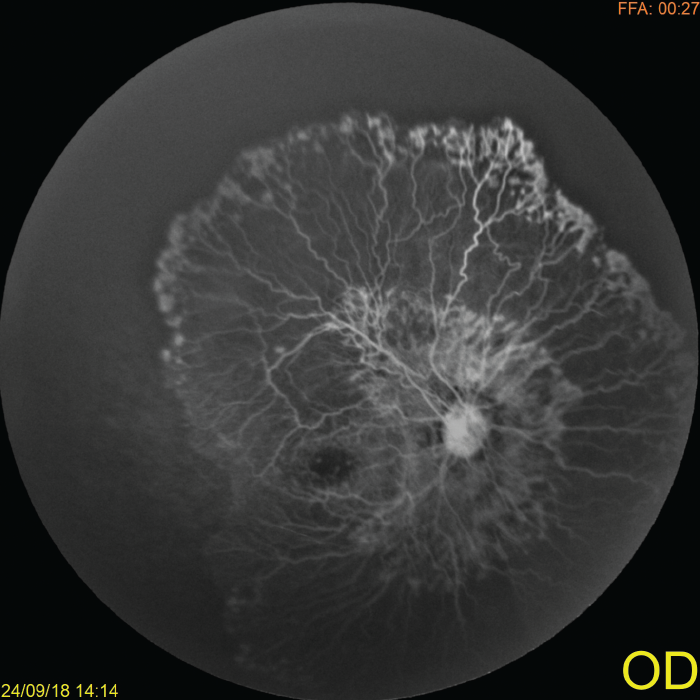
Fundus Fluorescein Angiography (FFA) of an ROP baby during EUA, revealing type 1 retinopathy of prematurity (ROP). If left untreated, this condition can lead to retinal detachment
Aggressive refractive and amblyopic care until the child’s visual potential can be reached is crucial. KEU is the only center in Rwanda with a low vision aid department, where children come for supportive management.
When not to operate. We tend not to operate in advanced late stage 5 cases with corneal opacification, or when one eye has no traction RD whilst the other eye has advanced stage 4B/5.
Over the past two years, I’ve operated on more than 120 eyes with a reasonable success rate, establishing KEU as the only center in the region treating ROP detachments.
ROP surgery has shaped my professional growth, allowing me to help families while raising the profile of KEU. Witnessing the individual impact of this type of surgery has helped to reaffirm my belief that early surgical intervention can have a lifelong effect on patients, providing hope and brighter futures for these children and their families.
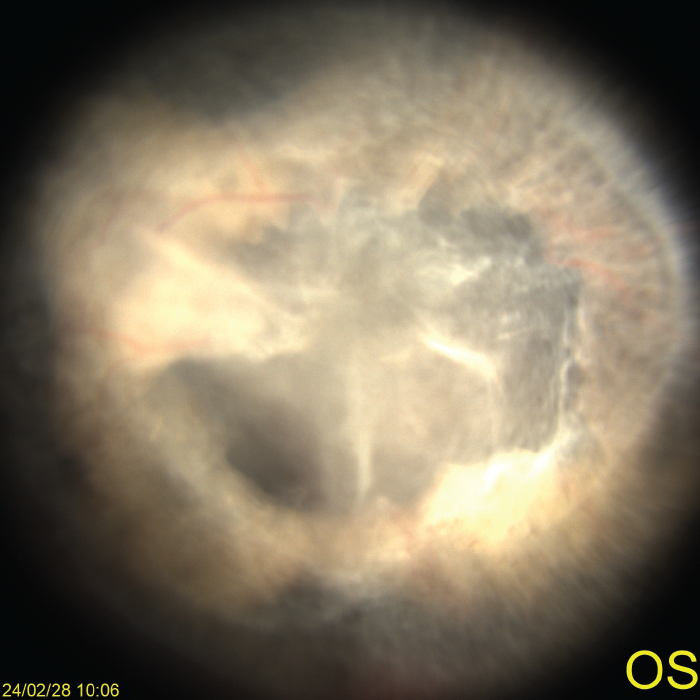
Color photograph of a 6-month-old baby with Stage 5 Retinopathy of Prematurity (ROP) exhibiting funnel-shaped detachment in the left eye
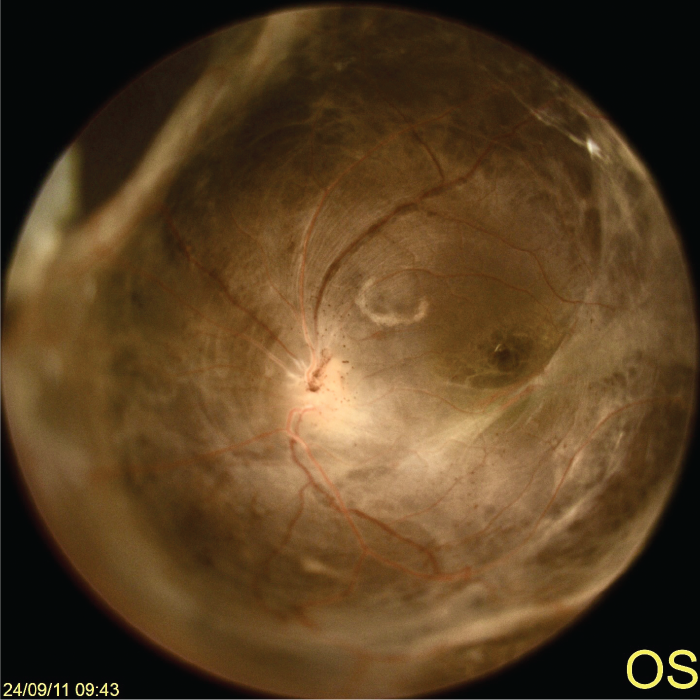
Postoperative image taken six months after surgery, demonstrating the opening of the funnel detachment and partial reattachment of the retina
