Sometimes an occasional missed drug dose isn’t a big deal; sometimes, it’s deadly. But often, in ophthalmology, it ends up with patients losing vision. It’s understandable that people are busy, forgetful, and in the case of intravitreal injections, can strongly dislike the procedure or find monthly clinic visits inconvenient – but it can be acutely frustrating to watch a patient lose vision because of something as simple (yet as common) as regimen noncompliance.
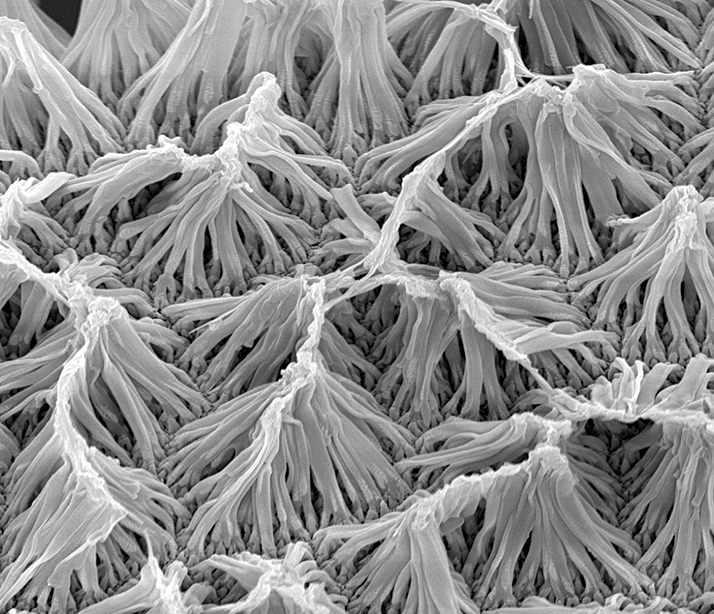
One method of addressing this problem is the use of implants that slowly release therapeutic drug doses over an extended period – and there are already a few of them on the market today. But these release their drug based on a combination of the formulation’s intrinsic release properties and the local ocular environment in which it’s placed. What if you wanted more control? A neuroscientist, Wen Gao, and a biomedical engineer, Richard Ben Borgens, may have an answer: a “smart” nanowire that releases drugs when exposed to a strong electromagnetic field (1). The nanowires are fabricated out of the inert, biocompatible polymer polypyrrole (Figure 1), and can be loaded with a drug. Borgens explained, “When the correct electromagnetic field is applied, the nanowires release small amounts of their payload. This process can be started and stopped at will, like flipping a switch.”
To test their tiny drug delivery device, they impregnated the nanowires with dexamethasone, deposited them onto a droplet of sterilized water, placed it on a spinal cord lesion in a mouse, and then applied an electromagnetic field for two hours a day for a period of one week. Compared with controls, treated mice showed significantly lower levels of glial fibrillary acidic protein, a marker of spinal inflammation, at the location of the spinal injury. Furthermore, the effect was hyperlocal – no systemic dexamethasone was detected in the mice. The authors noted one major limitation: the maximum depth that the implanted nanowires would function was limited to just under 3 cm, although as the mean axial length of an adult human eye is ~2.4 cm, this shouldn’t be a problem with ophthalmic use. They are also working on developing biodegradable nanowires. This technology is years from making it to the market (if it ever does), but the implications for telemedicine if it does so are quite profound. If we take the example of a patient with wet AMD; rather than be assessed and injected every month or two with an anti-VEGF agent by a hospital-based ophthalmologist, the patient could see the ophthalmologist just once to be injected with the nanowires, and then be monitored by a local optometrist or community healthcare center using automated OCT imaging devices. The resultant images can be assessed remotely (or by algorithm), and the appropriate dose can be calculated automatically and administered by timing the patient’s EMF exposure. And if the EMF device is something a patient could take home and have programmed remotely, the drug administration part becomes even easier – and helps ensure that the patient receives the effective therapy they need every time they need to receive it.
References
- W Gao, RB Borgens, “Remote-controlled eradication of astrogliosis in spinal cord injury via electromagnetically- induced dexamethasone release from “smart” nanowires”, J Control Release, 13, 22–27 (2015). PMID: 25979326.
