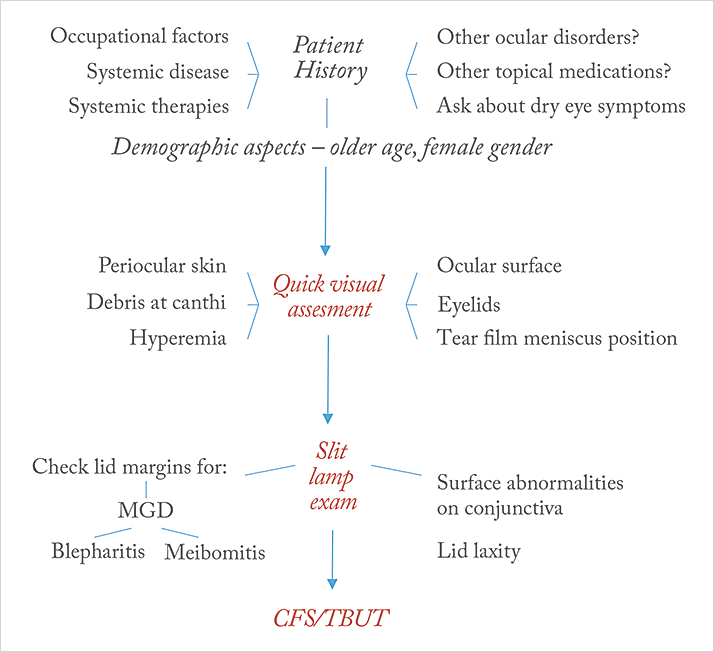
As we’ve seen in previous issues of The Ophthalmologist, there’s a significant proportion of patients with glaucoma who are, or will become, sensitive to the preservatives present in their topical glaucoma medications, and this typically manifests itself as ocular surface disease (OSD) – most commonly as dry eye disease (1,2). This is something that’s best avoided as it negatively impacts patients’ quality of life (2,3) and adherence to their topical glaucoma medication regimens, ultimately accelerating disease progression (4,5). In recognition of the extent of the issue, the European Glaucoma Society (EGS) advise that “particular attention should be paid to glaucoma patients with pre-existing OSD or to those developing dry eye or ocular irritation over time” (6). Further, the European Medicines Agency recommends avoiding preservative-containing topical therapies in patients who do not tolerate eye drops with preservatives, and considering the use formulations without preservatives as a valuable alternative for long-term treatment (7). Clearly, it’s important to find these patients and switch their medications wherever possible, as soon as possible. So how do you identify them? The first thing to do – before any examination – is to take the patient’s history (8), see Figure 1. Ask the patient about any factors that might impair ocular surface function, including occupational factors like computer display use, and any systemic diseases or therapies that may cause them to experience OSD, and consider the patient’s age and gender – older age and female sex predispose patients to OSD (8). If you don’t already have the information, ask the patient about any other ocular disorders they may have been previously diagnosed with, and what other ocular topical therapies they may be taking: if they’re self-administering over-the-counter artificial tears, then that suggests the presence of some degree of OSD. Finally, ask about dry eye symptoms: do they have discomfort along the lines of a “recurrent sensation of sand or gravel in their eyes”, or visual disturbances such as contrast sensitivity, decreased visual acuity and increased optical aberrations? (8).
You then follow this with a clinical assessment. The EGS’ guidelines (6) state that this can be achieved with “careful assessment of redness of the eyelid margin, positive corneal and conjunctival fluorescein staining or reduced tear break-up time”. Recently, Stalmans et al., (8) have also proposed three quick and easy steps are required to assess the patient. The first step is essentially a series of quick glances. Examine the ocular surface, the eyelids (particularly the lower lid) and the periocular skin for any signs that are suggestive of meibomian gland dysfunction (MGD), and look out for abnormal positioning of the tear film meniscus, the presence and location of any apparent hyperemia, and finally, check for the presence of any debris at the canthi. The second step is a slit lamp examination: check the lid margins for signs of MGD, meibomitis or blepharitis. Examine the bulbar and tarsal conjunctiva for surface abnormalities that might affect tear film distribution, and remember to check for lid laxity causing possible lid malpositions, by determining the distance between the peripheral cornea and the inferior lid border. If, at this stage, OSD is suspected, the third step is to reach for the fluorescein bottle, in order to perform conjunctival fluorescein staining (CFS), in order to assess tear film stability (with tear film break-up times [TBUT] of <10 seconds considered abnormal) and to identify any damage to the corneal epithelium (helping to assess the severity of the disease). These simple steps: talking with the patient, taking their history, quick visual assessments (with and without the slit lamp) followed (where appropriate) by CFS/TBUT assessments, will help identify those patients who will benefit from preservative-free topical glaucoma therapy (8). Although many patients with glaucoma receive preservative-containing topical medications and don’t have OSD, continual review of these patients is advised – consider taking the time to explain the issues that the preservatives in their medications can sometimes cause, and alerting them to the early signs of OSD. Dialogue between you and your patient could mean that timely switching to preservative-free therapies is performed, reducing the potential in some patients for poorer clinical outcomes.
Next month
A discussion on the impact of preservative-containing topical glaucoma therapy on glaucoma surgery outcomes. Preservatives present in topical glaucoma therapies may adversely affect the outcomes of surgical procedures (9). Job Code: STN 0717 TAP 00019 (EU).Date of preparation: July 2015.
References
- C Baudouin, et al., “Preservatives in eyedrops: the good, the bad and the ugly”, Prog Retin Eye Res, 29, 312–334 (2010). PMID: 20302969. RD Fechtner, et al., “Prevalence of ocular surface complaints in patients with glaucoma using topical intraocular pressure-lowering medications”, Cornea, 29, 618–621 (2010). PMID: 20386433. GC Rossi, et al., “Dry eye syndrome-related quality of life in glaucoma patients”, Eur J Ophthalmol, 4, 572–579 (2009). PMID: 19551671. B Sleath, et al., “The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity”, Ophthalmology, 118, 2398–2402 (2011). PMID: 21856009. P Denis, et al., “Medical outcomes of glaucoma therapy from a nationwide representative survey”, Clin Drug Investig, 24, 343–352 (2004). PMID: 17516721. European Glaucoma Society, “Terminology and Guidelines for Glaucoma – 4th Edition”, EMEA/622721/2009 (2014). Available at: bit.ly/egs2014. Accessed June 29, 2015. European Medicines Agency, “EMEA public statement on antimicrobial preservatives in ophthalmic preparations for human use” (2009). Available at: bit.ly/EMA2009, accessed July 03, 2015. I Stalmans, et al., “Preservative-free treatment in glaucoma: who, when, and why”, Eur J Ophthalmol, 23, 518–525 (2013). PMID: 23483513. C Boimer, CM Burt, “Preservative Exposure and Surgical Outcomes in Glaucoma Patients: The PESO Study”, J Glaucoma, 22, 730–735 (2014). PMID: 23524856.
