Featuring
Chair: Ingeborg Stalmans, Head of the Glaucoma Unit, University Hospitals Leuven; Director of the Laboratory of Ophthalmology, Catholic University of Leuven, Belgium
Alain Bron, Professor of Ophthalmology at the University Hospital of Dijon, France
Ike K. Ahmed, Ophthalmologist at Prism Eye Institute; Assistant Professor, Fellowship Director, Kensington Eye Institute, University of Toronto; Clinical Professor, University of Utah; Research Director, Kensington Eye Institute, University of Toronto; Co-Medical Director, TLC Mississauga, Canada
Florent Aptel, Professor of Ophthalmology and Head of the Glaucoma and Anterior Segment Unit, University Hospital of Grenoble, France
On September 15, 2019, in a packed auditorium at the European Society of Cataract and Refractive Surgeons Congress in Paris, France, a panel of renowned experts shared their glaucoma surgery experiences with Santen’s PRESERFLO™ MicroShunt. Chaired by Ingeborg Stalmans, the symposium – “What do you expect from glaucoma surgery?” – began with two lectures, delivered by Alain Bron and Ike Ahmed, and culminated in a panel discussion of real-life case studies.
The PRESERFLO™ MicroShunt: What you need to know
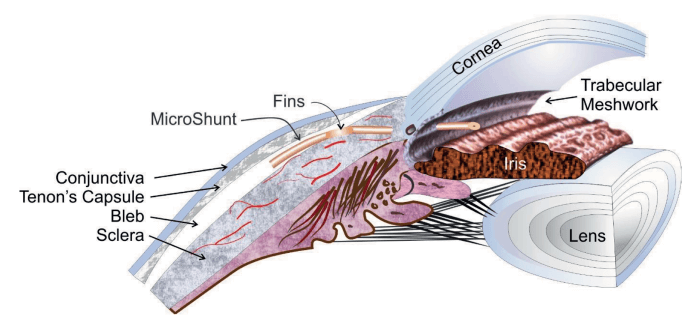
• The PRESERFLO™ MicroShunt is a state-of-the-art glaucoma drainage device, which, like trabeculectomy, uses the subconjunctival pathway, therefore allowing more effective IOP reduction compared with procedures that increase trabecular or uveoscleral outflow (1, 2, 3, 4).
• The PRESERFLO™ MicroShunt benefits from both innovative design (wings which prevent migration and leakage around the tube and direct device orientation) and material (biostable and biocompatible SIBS which minimizes inflammation, scarring and capsule formation, and is soft and flexible to minimize erosion) (2, 3, 4, 5, 6).
• The PRESERFLO™ MicroShunt helps decrease the risk of complications – it is inserted via an ab externo procedure that allows for more predictable outcomes than ab interno implantation (2, 3, 4, 5, 7).
• The PRESERFLO™ MicroShunt first received its CE mark in 2012 (2).
How can we meet the needs of glaucoma patients?
Chair Ingeborg Stalmans invites Alain Bron to talk about unmet needs in glaucoma, which, he admits, are numerous. Bron notes how intraocular pressure (IOP) is the only modifiable risk factor in glaucoma management, and explains that, according to the current guidelines, there is no single target IOP level appropriate for every patient, which means that any treatment decisions are personalized. The clinician must make a choice from a range of available treatment options: drug therapy, laser surgery and traditional surgical approaches (8). For every patient, numerous risk factors, including existing glaucoma damage, life expectancy, untreated IOP values and rate of progression, need to be taken into consideration collectively when deciding on an individual’s desirable target IOP (8).
Bron notes how the rate of glaucoma surgery varies greatly between countries, referring to a survey of 21 countries – from 2.9 per million per year in Ivory Coast to 500 surgeries per million per year in Germany (9). Bron also highlights that the overall number of glaucoma surgeries is decreasing, with trabeculectomy numbers in the USA falling consistently since 1996, following the launch of prostaglandins for IOP control (10). In France, says Bron, the number of surgeons performing glaucoma surgery decreased from 713 to 610 for trabeculectomies and from 288 to 263 for deep sclerotomies, respectively, between 2012 and 2014 (11). At the same time, the number of cataract procedures in France has almost doubled (12). Among other factors, the high rate of complications in the glaucoma subspecialty means surgery is often considered a last resort when medication and laser fail to control IOP and prevent vision loss (13, 14). Glaucoma specialists are still searching for the “Holy Grail” solution, which Peng Khaw defines as the 10/10/10 rule: a 10-minute technique that will reduce the IOP to 10 mmHg for at least 10 years (15).
Minimally invasive glaucoma surgery (MIGS) have entered the market in recent years, giving glaucoma specialists new surgical treatment options. But, says Bron, further evidence is needed to determine the efficacy of these new approaches in patients at different stages of glaucoma and with different symptoms. As well as efficacy, cost is also an important consideration for new treatment options entering the market. Bron points out that both MIGS and trabeculectomy are needed, that artificial barriers should not be created, and that patient outcomes matter most. He concludes, “These new techniques are attracting young doctors into the glaucoma subspecialty, and they are giving patients new hope.”
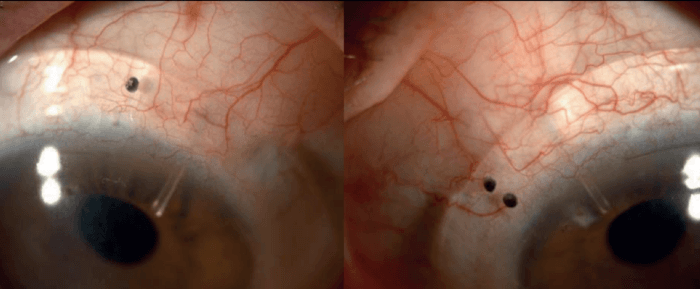
Case: Long-term effectiveness and safety
Ike Ahmed then presents one of his first PRESERFLO™ MicroShunt cases. The patient was a 56-year-old South Asian male, referred with progressive visual field loss in the left eye. IOP values were 13-16 mmHg in the right eye, and 15-17 mmHg in the left eye. He was on three classes of medications. As Ahmed points out, the patient had thinner corneas, which is typical for South Asians. The patient was a high myope and had lattice corneal dystrophy with recurrent corneal erosions; he wore PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) contact lenses from BostonSight®. With home tonometry, significant pressure fluctuations were observed. After a successful procedure using the PRESERFLO™ MicroShunt, the patient was able to wear his PROSE contact lenses over the bleb (see Figure 2). As Ahmed concludes, five years later, the patient’s vision is stable, with pressure in the range of 6-10 mmHg, and no issues with hypotony.
Living in the real world
Ike Ahmed, presenting his real-world experience with Santen’s PRESERFLO™ MicroShunt, points out that a standing-room-only glaucoma symposium at a cataract and refractive meeting signals a welcome change for the glaucoma subspecialty! Ahmed is unequivocal about the fact that glaucoma care is moving towards interventional treatments, which, he notes, can lower IOP earlier, in a safer manner, while addressing adherence and compliance issues. Interventional glaucoma, whether it’s MIGS, drug delivery, novel compounds or surgical procedures, must not only aid clinicians in preventing blindness in a cost-effective way, but also address quality-of-life issues associated with the treatment burden, argues Ahmed. These days, new treatment paradigms with proven safety have not yet been sufficiently evaluated for efficacy. The goal is to have treatments that are at least as efficacious as the solutions we have today, says Ahmed, but also with the ability to change patient outcomes in a safer and more predictable manner.
Enter the PRESERFLO™ MicroShunt – a predictable way of draining aqueous fluid into the subconjunctival space. Ahmed notes the device’s 70 μm lumen and an 8.5 mm length, but particularly highlights the innovative material, which was originally designed for coating coronary stents (2, 3). In the past, surgical devices have been made from polyurethane or silicone rubber – unstable compounds that can degrade and cause chronic inflammation. The innovative poly(styrene-b-isobutylene-b-styrene)(SIBS) compound is more biocompatible (3); Ahmed refers to a study that shows how the material reduces inflammation in normal rabbit eyes (16). The studies have also shown “dramatic differences” in the amount of myofibroblasts and the thickness of the pseudo-capsule around the SIBS material in comparison to other materials. Crucially, says Ahmed, the SIBS material helps tackle one of the biggest challenges in glaucoma surgery – wound and tissue healing (16).
Rather than using complicated valves to control outflow, says Ahmed, the PRESERFLO™ MicroShunt leverages the Hagen Poiseuille equation to set a level of resistance that prevents pressures falling below 6 mmHg at normal aqueous production.
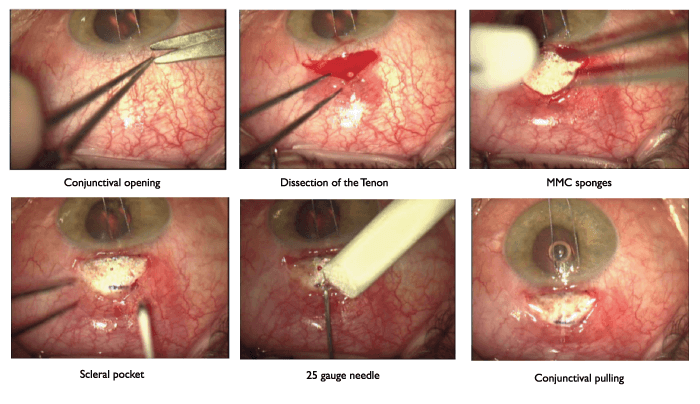
Presenting his implantation technique, Ahmed notes that successful implantation of any surgical device is predicated by the surgeon and their abilities; they are key in delivering desirable outcomes – and, he says, significant differences arise when surgeons vary their technique, potentially resulting in sub-optimal outcomes. “Not for the lazy or those who want to rush,” Ahmed notes that time and care spent during the procedure save considerable time after surgery – for the patient’s lifetime.
Ahmed admits he was originally sceptical about early pilot study data on the PRESERFLO™ MicroShunt (4); in fact, he says he couldn’t believe how good the outcomes were. He shares his own one to two-year data. Ahmed points out that the mean IOP of 150 patients (95 percent follow-up rate) 12 months after implantation with PRESERFLO™ is 13.3 mmHg with an average of 0.5 medications, compared with 21.4 mmHg and 3.4 medications pre-op – “a dramatic reduction,” says Ahmed. Ahmed calls attention to the reduction in the number of medications: at one year post-op, retention of about 80 percent was a “complete success,” with a qualified success for 95 percent, with 75 percent of patients without medication. One of the biggest factors for success, according to Ahmed, was using 0.4 mg/ml mitomycin C (MMC).
Complications in this group were very few and not serious, says Ahmed. The needling rate was low at 8.5 percent, and very few postoperative interventions, revisions or reoperations were required.
Talking more broadly, Ahmed says that, over five years and 1200 eyes, the team has tried the PRESERFLO™ MicroShunt in every possible glaucomatous scenario – and they feel “very comfortable” with the approach. Ahmed’s patients have experienced a rapid return of visual function, minimal numbers of post-op visits and interventions, and were eager to get the same result for their other eye.
Ahmed completes his presentation by bringing the focus back to blebs. The goal, he reiterates, is not just lowering pressure but doing so more safely, which requires the “right” kind of bleb. We need to think about long-term efficacy (IOPs in the low teens and medication free), he says, but also visual recovery, comfort, frequency of post-op visits and interventions. Safety should be a key consideration and, for this reason, Ahmed says a posterior bleb is desirable. Ultimately, safer and more effective bleb surgery will increase the likelihood of its use earlier in the treatment paradigm.
Considering post-op IOP stability, Ahmed shares data visualizations of IOP fluctuations over two months post-op for trabeculectomy (n=169), XEN® Gel Stent (n=185) and PRESERFLO™ MicroShunt (n=196) patients. For trabeculectomy patients, “IOPs are all over the place – up and down everywhere,” says Ahmed. “XEN® is better, and PRESERFLO™ MicroShunt is even better.” Ahmed points out that the high level of IOP control achieved with PRESERFLO™ MicroShunt makes his and his patients’ lives much easier. “They recover quickly, they go home, and I follow up as frequently as needed.” Better IOP control leads to better visual recovery, says Ahmed, who again compares PRESERFLO™ MicroShunt with trabeculectomy and XEN®. The powerful combination of rapid visual recovery and well-controlled pressure afforded by such procedures, says Ahmed, points the way to earlier intervention of this type – “We’re more confident that
we’re performing a procedure that has more efficacy.”
“There’s a role for MIGS, a role for phacoemulsification, and a role for medications and lasers as well,” says Ahmed. “But in my hands – in the real world – the role of subconjunctival MIGS, such as the PRESERFLO™ MicroShunt, is to deliver safety and efficacy that allows us to embrace interventional glaucoma earlier.”
Case: Post-op management
Florent Aptel presents a case study of a 62-year-old male with progressive primary open-angle glaucoma, referred for glaucoma surgery on both eyes. The patient had a decade-long history of medical treatment; his IOP was 22 mmHg in the right eye, and 23 mmHg in his left eye. Trabeculectomy with 0.2 mg/ml MMC was performed in 2017 on his right eye, and six months later the pressure value, with two medications, was 16 mmHg. PRESERFLO™ MicroShunt was implanted in his left eye in 2018, using 0.2 mg/ml MMC. Post-op care included dexamethasone application four times a day for three months. The patient’s post-op pressure values, with no medications, were as follows:
• 3 months: 12 mmHg
• 6 months: 12 mmHg
• 12 months: 14 mmHg
• 18 months: 13 mmHg, with a diffuse avascular bleb.
After presenting the case, Aptel explains that he usually follows up with PRESERFLO™ MicroShunt patients one week, one month, three months and then every six months post-op. Aptel comments on the low rates of complications being one of the main advantages of the PRESERFLO™ MicroShunt over trabeculectomy and other MIGS devices, with few revisions needed (20). ”
Conclusion
Ingeborg Stalmans concludes based on the presentations and the discussion it is clear that there has been an unmet need in glaucoma surgery: finding the right balance between efficacy and safety. Reducing IOP is the only currently known effective approach to managing progression of the disease. As Bron pointed out, glaucoma surgery
has a very high risk of complications (50 percent), compared to other ophthalmic subspecialties, so it should be considered when therapeutic treatment appears unlikely to maintain the patient’s sight in the eye affected with glaucoma. Therefore, any new devices or procedures aimed at lowering the IOP less invasively, should be given proper consideration. The PRESERFLO™ MicroShunt presents such an option, by effectively reducing IOP while at the same time decreasing the risk of complications (2, 3, 4, 7). Surgeons’ experiences with real-world cases and the discussions that followed illustrated how the PRESERFLO™ MicroShunt supports them in meeting glaucoma patients’ needs and, as a result, improving outcomes.
References
- E Ansari, “An update on implants for minimally invasive glaucoma surgery (MIGS)”, Ophthalmol Ther, 6, 233 (2017). PMID: 28730285.
- L Pinchuk et al., “The use of poly(styrene-blockisobutylene-block-styrene) as a microshunt to treat glaucoma”, Regen Biomater, 3, 137 (2016). PMID: 27047682.
- L Pinchuk et al., “The development of a micro-shunt made from poly(styrene-block-isobutylene-blockstyrene) to treat glaucoma”, J Biomed Mater Res B Appl Biomater, 105, 211 (2017). PMID: 26380916.
- J Batlle et al., “Three-year follow-up of a novel aqueous humor MicroShunt”, J Glaucoma, 25, e58 (2016). PMID: 26766400.
- PRESERFLO™ MicroShunt glaucoma drainage system. Instructions for Use.
- L Pinchuk et al., “Medical applications of poly(styrene-block-isobutylene-block-styrene) (“SIBS”)”, Biomaterials, 29, 448 (2008). PMID: 17980425.
- RMH Lee, “The Implications of an Ab Interno Versus Ab Externo Surgical Approach on Outflow Resistance of a Subconjunctival Drainage Device for Intraocular Pressure Control”, Transl Vis Sci Technol, 8, 58 (2019). PMID: 31293813.
- European Glaucoma Society, Terminology and Guidelines for Glaucoma, 4th edition, Publicomm: 2014.
- K Mansouri et al., “Global rates of glaucoma surgery”, Graefes Arch Clin Exp Ophthalmol, 251, 2609 (2013). PMID: 24068429.
- KS Arora et al. “Use of various glaucoma surgeries and procedures in Medicare beneficiaries from 1994 to 2012”, Ophthalmology, 122, 1615 (2015). PMID: 26092196.
- AM Bron et al., “Trends in operating room-based glaucoma procedures in France from 2005 to 2014: a nationwide study”, Br J Ophthalmol, 101, 1500 (2017). PMID: 28292777.
- C Creuzot-Garcher et al., “Incidence of acute postoperative endophthalmitis after cataract surgery: a nationwide study in France from 2005 to 2014”, Ophthalmology, 123, 1414. (2016). PMID: 26992840.
- MarketScope, “2018 Glaucoma Surgical Device Report: A Global Market Analysis for 2017 to 2023, August, 2018” (2018). Available at https://bit.ly/2JlGk7h. Accessed October 24, 2019.
- R Thomas, F Billson, “The place of trabeculectomy in the management of primary open-angle glaucoma and factors favouring success”, Aust N Z J Ophthalmol, 17, 217 (1989). PMID: 2679810.
- P Khaw, “Treatment at the crossroads”, Eurotimes, 18, 4 (2013).
- AC Acosta et al., “A newly designed glaucoma drainage implant made poly(styrene-b-iosbutyleneb- styrene)”, Arch Ophthalmol, 124, 1742 (2006). PMID: 17159034.
- G Durr et al., “Intermediate term outcomes of superior or inferior ab-externo SIBS microshunt in refractory eyes”, Ophthalmology & Vision Sciences, University of Toronto (2019).
- M Schlenker et al., “Intermediate Term Outcomes of SIBS Microshunt Alone or in Combination with Phacoemulsification” (2019).
- M Schlenker et al., “Ab externo SIBS Micro-Shunt with MMC efficacy and safety: consecutive interventional cohort” (2018).
- F Aptel et al. “Two-year results of the MicroShunt Glaucoma Drainage System in patients with primary open-angle glaucoma”. Presented at AAO 2018; Chicago, USA. PO #109.
