
Click here for A Way Out of the Dark, the main feature by Rupert Bourne
The number of individuals with mild vision impairment (VI), moderate to severe (MSVI) and blindness is highest in Eastern Europe (5.34, 11.08, and 0.79 million, respectively), followed by countries of Central Europe (1.98 million, 3.95 million, and 0.33 million, respectively) and Central Asia (2.20 million, 2.95 million, and 0.30 million, respectively). Similarly, the number of individuals with near VI is highest in Eastern Europe (26.03 million), followed by Central Europe (12.18 million), and Central Asia (5.04 million).
Uncorrected refractive error (9.6 million) was the most frequent cause of reversible VI, followed by other causes of vision loss (4.5 million), and cataract (3 million). Age-related macular degeneration (AMD) (228,000), glaucoma (213,000), and diabetic retinopathy (144,000) were most commonly responsible for irreversible vision impairment. The most common causes for blindness were glaucoma (178,000), followed by cataract (291,000) AMD (63,000), uncorrected refractive error (29,000), and diabetic retinopathy (14,000). In Central Europe, Eastern Europe, and Central Asia there are more people blind due to cataract (52,000, 173,000, and 66,000, respectively) than glaucoma (38,000, 105,000, and 35,000, respectively). In Eastern Europe, uncorrected refractive error (16,000) was responsible for more people being blind than in Central Europe and Central Asia (4,000 and 10,000 respectively).
Between 1990-2010, the age-standardized prevalence of mild VI, MSVI, and blindness decreased the most in Central Europe (by 12.0 percent, 2.6 percent and 22.8 percent, respectively), and Central Asia (by 7.6 percent, 4.1 percent, and 26.8 percent, respectively). Stratified by the various causes of vision impairment, the decrease in the age-related prevalence of MSVI and blindness was most marked for glaucoma (1.4 percent, 28.5 percent, respectively) and uncorrected refractive error (4.5 percent, 20.7 percent, respectively). Forecasting to the year 2050, the numbers of blind and people with MSVI are expected to increase, particularly in Eastern Europe; however, the age-standardized prevalence of blindness is estimated to decrease; while MSVI rates are expected to remain relatively stable.
Myopic maculopathy was the second most frequent cause for irreversible MSVI and the second most common cause for blindness in the Ural Eye and Medical Study, one of the few sources of data for Eastern Europe. It shows the importance of myopia as a potentially blinding disease for Eastern Europe and Central Asia, and it demonstrates how important it is that meta-analyses explicitly separate myopic maculopathy from AMD within the group of macular diseases as a cause for vision impairment.
The high-income super-region includes countries of the high-income Asia Pacific region, high-income North America region, Western Europe, Australasia, and Southern Latin America. Within the high-income super-region, the number of individuals with mild VI, MSVI and blindness is highest in Western Europe (10.91, 15.42, and 1.53 million, respectively), followed by the high-income Asia Pacific countries (9.84, 5.34, and 0.54 million) and high-income North America (5.14, 7.44, and 0.71 million), and it is lowest in Southern Latin America (1.29, 2.12, and 0.16 million) and Australasia (0.43, 0.75, and 0.07 million). In contrast, the number of individuals with near vision impairment is highest in high-income North America (4.93 million), followed by Western Europe (4.49 million), and high-income Asia Pacific (1.98 million). In the whole high-income super-region and in each of the subregions, by far the leading cause for MSVI was under corrected refractive error (17 million), followed by cataract (8 million).
The most common causes for irreversible MSVI were age-related macular degeneration (AMD) (739,000), glaucoma (597,000) and diabetic retinopathy (420,000). The most common causes for blindness were glaucoma (786,000), followed by AMD (596,000), cataract (506,000), diabetic retinopathy (161,000), and under corrected refractive error (80,000). In high-income North America, Australasia and Southern Latin America, the number of cataract-related blind individuals (160,000, 18,000, and 49,000, respectively) was higher than the number of glaucoma-related blind persons (154,000, 15,000, and 25,000).
In Western Europe, the number of individuals blind due to AMD (446,000) was higher than the number of individuals blind due to glaucoma (439,000). In the period from 1990-2010, the age-standardized prevalence of mild vision impairment, MSVI, and blindness reduced the most in Southern Latin America (7.2 percent, 2.0 percent, and 28.7 percent), and the least in high-income North America (1.4 percent, 0.9 percent, and 0.7 percent). Stratified by the various causes of vision impairment, the decrease in the age-related prevalence of MSVI and blindness was most marked for AMD (8.3 percent and 26.9 percent), followed by glaucoma (1.5 percent, 24.7 percent), and under corrected refractive error (4.4 percent, 22.9 percent).
The marked decrease in AMD as a blinding cause may be due to the clinical introduction of intraocular anti-VEGF (vascular endothelial growth factor) therapy for the exudative form of AMD. In the forecast of the situation in the year 2050, the numbers of blind individuals and individuals with MSVI are estimated to further increase, in particular in high-income North America, Western Europe and high-income Asia Pacific, while the age-standardized prevalence of blindness is estimated to decrease (except for Southern Latin America). Age-standardized rates for MSVI are estimated to remain constant.
In 2020, there were 77.55 million people with vision loss in Latin America and the Caribbean, including 3.66 million with blindness, 24.48 million with MSVI, 21.47 million with mild VI, and 27.94 million with near VI. VISION 2020 has made great strides in the region, with national VISION 2020 or prevention of blindness committees established in nearly every country at some point. Intersectoral collaboration between ministries of health, national societies of ophthalmology, and nongovernmental organizations has resulted in increased epidemiological coverage, increased cataract surgical rates, and capacity building throughout the region.
Cataract surgical services are a regional strength. Regional epidemiological data generally supports gender equity in eye health, particularly with cataract surgical coverage, although some countries demonstrate disparities. However, men have had greater reductions in prevalence rates than women, but this is likely due to regional demographic trends. The highest prevalence of blindness in most of Latin America and the Caribbean has shifted from cataract to other vision loss, indicating a regional need to strengthen comprehensive eye care. The changing trends in vision loss have likely been driven by the aging population and strengthened economies in some areas, but the most important driver may be the increased epidemiological coverage. However, a paucity of epidemiological data available for younger age groups remains.
Challenges to VISION 2020 in the region include the continuity of national committees, which tend to get disbanded and occasionally reactivated with changes in government, and the need for ongoing external facilitation to ensure that all public and private stakeholders are engaged in the implementation of national, regional, and global eye health plans. Though ophthalmologists vis-à-vis their national societies have had a strong VISION 2020 role, the role of optometrists and allied health professionals is grey, given the lack of universal definitions for these cadres, with many positions lacking formal training and certification and professional societies for advocacy.
The greatest emerging threat to vision loss in Latin America and the Caribbean is the rapidly growing epidemic of diabetes. In 2019, the International Diabetes Federation estimated that there were 79.2 million people living with diabetes in the Western Hemisphere, which affected 13.3 percent of people in North America (including Mexico) and the Caribbean and was expected to increase to 15 percent within 20 years. The rise of diabetic eye disease and diabetes-related complications that may affect cataract surgical outcomes could have dire consequences over the coming decades.

In 2020, there were 53.79 million people with vision loss in North Africa and the Middle East (NAME). This includes 3.09 million with blindness, 21.8 million with MSVI, 14.4 million with mild VI, and 14.5 million with near VI. Cataract was the most common cause of blindness (0.756 million [95 percent UI 0.593-0.841]), followed by glaucoma (0.463 million [0.354-0.578]), age-related macular degeneration (0.194 million [0.136-0.264]), under corrected refractive error (0.842 million [0.638-0.103]), and diabetic retinopathy (0.61 million [0.401-0.918]).
Cataract was also the leading cause of MSVI (5.02 million [4.23-5.92]), followed by under corrected refractive error (4.68 million [3.96-5.55]), age-related macular degeneration (0.493 million [0.39-0.613]), diabetic retinopathy (0.399 million [0.288-0.54]), and glaucoma (0.325 million [0.251-0.419]). Between 1990 and 2020, the age-standardized prevalence decreased by 41.5 percent (-2.7 to -40.3) for blindness, by 6.1 percent (-7.3 to -4.5) for MSVI, by 10.1 percent (-10.9 to -9.2) for mild VI, and by 14.0 percent (-16.8 to -11.5) for near VI.
The age-standardized prevalence due to all causes of blindness has decreased between 1990 and 2020, with the exception of diabetic retinopathy, which has increased by 0.9 percent (-6.2 to 9·3). The age-standardized prevalence of MSVI has decreased in the period from 1990 to 2010 for all causes except cataract, which increased by 0.6 percent (-2.1 to 3.6).
Cataract remains the first cause of blindness and MSVI, with increasing prevalence in the last three decades. Strengthened efforts in terms of promotion, availability, and accessibility are still needed to support high-volume, high-quality cataract surgery in the NAME countries, with intraregional cooperation required to help regions cope with the increased prevalence of visual impairment caused by cataract. Under corrected refractive error remains a major cause of MSVI. Several school eye health programs were established in several countries from the NAME region in association with non-governmental organizations to focus on detection and management of refractive error. These have certainly helped reduce the burden of visual impairment from uncorrected refractive error; however, further efforts are needed for early detection. It is suggested that countries perform vision tests at the beginning of every year to correct refractive errors in schoolchildren.
Diabetic retinopathy, age-related macular degeneration, and glaucoma are a public health problem in several countries in the NAME region. This may be the result of the aging population, combined with an increasing prevalence of diabetes mellitus. Development of educational programs and appropriate screening and management strategies – including promotion of telemedicine-based digital retinal imaging – can help reduce the risk of visual impairment from diabetic retinopathy, age-related macular degeneration, and glaucoma neuropathy.
The global burden of disease (GBD) super-regions, East Asia, Southeast Asia and Oceania, are home to approximately 2.5 billion people. Together, these regions contain some of the most populous and least populous regions on the planet.
The population of East Asia is aging faster than any other region in history. In 2020, there were 9.09 million people with blindness, 53.9 million with MSVI, 60.15 million with mild vision impairment, and 163.58 million with near vision impairment. It is estimated that East Asia’s elderly population – aged 65 years or older – will grow by 22 percent every five years for the next two decades. The increasing burden of cataract blindness presents a confronting challenge for this region, confounded by the increasing prevalence of age-related glaucoma and diabetes in urbanizing populations.
Southeast Asia comprises a mix of developing and high-income regions. In 2020, there were 5.95 million people with blindness, 28.77 million with MSVI, 30.51 million with mild vision impairment, and 29.49 million with near vision impairment. There remains a paucity of ophthalmic epidemiological data from developing regions, but preventable blindness including cataract and uncorrected refractive error remain significant problems in the adult population. Refractive error is exceptionally uncommon in children in developing regions, such as Lao PDR, but is expected to increase as education levels rise.
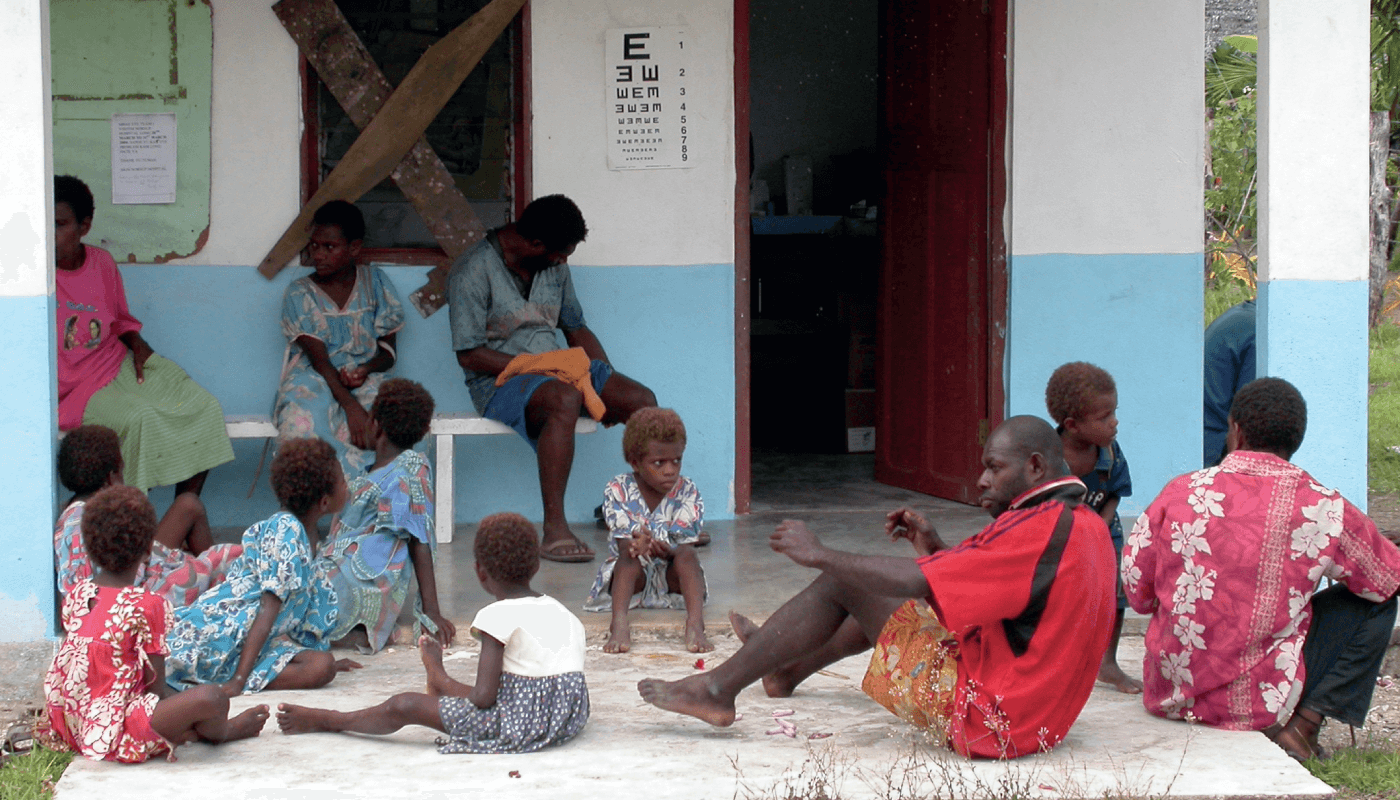
Although there is no universally accepted definition of Oceania – it is not a WHO-recognized region – Oceania broadly reflects the Pacific Island nations in the WHO Western Pacific region. In 2020, there were 40,000 people with blindness, 390,000 with MSVI, 380,000 with mild vision impairment, and 400,000 with near vision impairment. It contains some of the world’s smallest, most isolated and least populous nations, with the world’s highest prevalence of diabetes. In addition to the blinding complications of uncontrolled diabetes, cataract and uncorrected refractive error remain the most common causes of visual impairment in this region, whilst sustainable models of ophthalmic care are a significant challenge in these isolated island nations.
The leading causes of blindness and vision impairment in this super region were uncorrected refractive error and cataract. For diabetic retinopathy, there has been a 286.7 percentage change in cases of blindness caused by the condition between 1990 and 2020. It is crucial to put in place a national plan that prioritizes early screening, detection, and treatment of these ocular conditions, so as to better deal with their challenges. A good example would be the White Paper on Eye Health in China, launched in 2020, which shed light on current challenges, and also indicated work priorities for the next national eye health plan, including the incorporation of eye disease screening into the current chronic disease management system.

South Asia comprises the countries of Afghanistan, Bangladesh, Bhutan, India, Nepal, and Pakistan, and has a total population of 1.94 billion. In 2020, there were 60.08, 96.22, and 1.94 million people with MVI, MSVI, and with blindness, respectively. The total number of people with near-vision impairment from uncorrected presbyopia was 166.82 million. The age-standardized prevalence of blindness for females and males over the age of 50 was highest for cataract (5.0 percent and 3.9 percent, respectively), followed by refractive disorders (0.7 percent and 0.6 percent, respectively), and glaucoma (0.4 percent and 0.6 percent, respectively)
Refractive disorders were the most age-standardized prevalent cause of MSVI in females and males over the age of 50 (20.8 percent and 20.4 percent, respectively), followed by cataract (20.4 percent and 17.4 percent, respectively), macular degeneration (0.9 percent and 0.8 percent, respectively), and glaucoma (0.6 percent and 0.8 percent, respectively). Causes of MSVI and blindness in 54 and 1.5 million people, respectively, were cataract (29 and 6 million, respectively), AMD (1.2 and 0.298 million, respectively), glaucoma (0.955 and 0.579 million, respectively), and diabetic retinopathy (0.445 and 0.197 million, respectively).
Between 1990 and 2020, there was a significant decrease in age-standardized prevalence of blindness (-47.7 percent) and MSVI ( -12.6 percent) in adults over the age of 50. While age-standardized cataract-related causal blindness (-46.5 percent) decreased during this period, MSVI (+1.72 percent) showed a slight increase, as did age-standardized blindness related to diabetic retinopathy, with a rise of +17.7 percent. Blindness and MSVI related to glaucoma (-38.1 percent and -12.6 percent, respectively), age-related macular degeneration (-41.0 percent and -20.5 percent, respectively), and uncorrected refractive error (-52.3 percent and -23.3 percent, respectively) also decreased in prevalence. Promisingly, though the forecasted trends for those blind and/or with MSVI by 2050 shows an increase, age-standardized prevalence shows a significant decrease.
Cataract was the most significant cause of blindness in the region, followed by uncorrected refractive error, glaucoma, and age-related macular degeneration. Overall, the age-standardized prevalence of MSVI and blindness for all causes has shown a significant decrease since 1990, with the exception of diabetic retinopathy, which has increased. This is an important change; one that may be related to the rapidly shifting economy of South Asia as the region gradually improves its sociodemographic index (SDI), with associated lifestyle and life expectancy changes.
If levels of visual impairment and blindness are to be reduced substantially, several challenges in public health services and resource allocation must be overcome. Fortunately, due to improvement in economic standing and life expectancy, as well as the predicted decline in population post-2050, over time, South Asia may see a significant change in the causes and trends of regional blindness.
The sub-Saharan Africa (SSA) super-region (~1.1 billion population) generally includes the area south of the Sahara, including Eastern (~452 million), Central or Middle (~183 million), Western (~408 million), and Southern Africa (~68 million). Within this area, visual impairment is exceptionally high, especially considering the young age-structure of the region. By age 75, approximately 10 percent are estimated to be blind, with an additional 25 percent estimated to have MSVI. The absolute respective number of individuals with MVI, MSVI, and blindness is highest in Western Africa (15.99, 9.86, and 2.35 million), followed by Eastern Africa (11.33, 7.01, and 1.97 million), Central Africa (3.84, 2.01, and 0.29 million) and Southern Africa (2.53, 1.56, and 0.48 million).
The number with near visual impairment from uncorrected presbyopia is 19.99 million, 17.26 million, 4.71 million, and 9.57 million respectively, with the higher number in Southern Africa relative to distance visual impairment reflecting the older population (as age is the primary factor determining presbyopia). In general, the leading single cause of blindness in all these subregions was cataract, distantly followed by glaucoma, uncorrected refractive error, diabetic retinopathy, and age-related macular degeneration.
The leading cause of MSVI by several-fold was uncorrected refractive error, followed by cataract, with the other specified causes far behind. However, “other” causes of visual impairment – usually not specified in the source studies – were in aggregate a more common cause of blindness than cataract and were the second or third most common cause of MSVI. Overall, the change in cause-specific blindness has improved from 2000 after standardizing for age structure and population size – a shift which has been favorable for cataract (-29.4 percent), uncorrected refractive error (-14.5 percent), glaucoma (-23.7 percent), age-related macular degeneration (-19.4 percent) and “other” causes (-30.0 percent). The exception to this being diabetic retinopathy (+22.4 percent), as the population with diabetes mellitus rises, which is similar to that reported in other developing regions.
Changes in cause-specific MSVI were relatively small, with the exception of cataract (+13.2 percent), diabetic retinopathy (+9.2 percent) and “other” causes (-32.4 percent). The rise in cataract MSVI might reflect prioritization of cases with very advanced disease in backlog-clearing programs.
SSA is projected to have the highest age-standardized prevalence of blindness of any region of the world by 2050, which will translate to a huge increase in the burden of blinding eye disease as the population in this region rapidly ages. As most disease requires individual-level clinical care to avoid blindness, the need for expanding clinical training and institutional development is especially great in this region, especially when given the huge expected increase in the absolute number of visually impaired cases by 2050.
