- Astronauts experience cephalad fluid shifts in space, and this can harm ocular health
- Many of the issues have been linked to elevations in intracranial pressure – but not all astronauts have this problem
- NASA’s ocular health program aims to screen astronauts’ ocular health on the ground and in the ISS to try and understand when and why these changes occur
- Successfully understanding the underlying pathologies is key not only to developing prophylactic or treatment strategies – but these findings may also directly impact the future of manned interplanetary space flight
It was an incredible feat of engineering that thrust astronauts into space, and an even greater engineering and political achievement establishing the International Space Station (ISS). But why stop there? NASA intends to send a manned mission to Mars, which will hopefully represent humankind’s greatest space exploration achievement. However, having never evolved in microgravity, humans aren’t built for space travel. Indeed, the medical implications of being in space aren’t trivial (see Table 1 below), and these need to be better understood before humankind can boldly go anywhere in the cosmos for any length of time. Unfortunately, ocular health is something that the microgravity environment in space has the potential to seriously and permanently harm (see Table 2 below).
NASA has been aware for over four decades that space flight is associated with visual acuity impairment, but for many years these visual changes were thought to be minor, transient and not accompanied by other symptoms or significant clinical findings. In 2012, they reported that 15 male astronauts, aged between 45 and 55 years of age, had experienced visual and anatomical changes during or after long-duration flights (1, 2). The changes were not trivial, and included optic disc edema, globe flattening leading to hyperopic shifts, choroidal folds, retinal nerve fiber layer thickening, and increased intracranial pressure (see Figure 1). Some astronauts experienced transient changes that resolved post-flight, but others reported persistent visual acuity changes with varying degrees of severity. Such cases aren’t just a worry for the astronaut, but also their fellow crew, ISS managers, and all of Earth’s space agencies – you can’t have astronauts suddenly becoming unable to read the dials. Something had to be done. Missions to Mars are unlikely to succeed with visually-impaired astronauts.
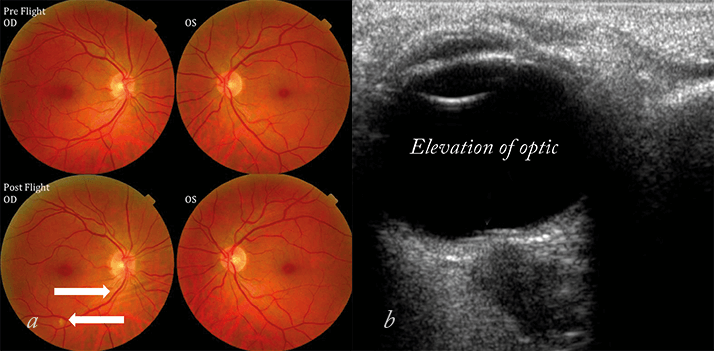
Table 1. Medical problems associated with space travel.
• Loss of bone density and muscle mass• Cardiac disorders
• Fatigue and sleep loss
• Psychological issues
• Cognitive decline/ accelerated development of Alzheimer‘s Disease
• Decompression illness
• Barotrauma
• Immune dysfunction
• Spaceflight radiation carcinogenesis
• Orthostatic intolerance
• Ocular disorders
Table 2. Ocular findings in astronauts.
To date, 21 US ISS long-duration spaceflight astronauts have developed some or all of the following:• Hyperopic shift (50% of astronauts)
• Scotoma
• Cotton wool spots
• Choroidal folds
• Optic nerve sheath distension*
• Globe flattening*
• Optic nerve edema*
* All three are associated with elevated ICP on Earth
Hunting the cause
Immediately, suspicions fell on fluid shift (3). On Earth, gravity constantly forces fluid in the body downwards. On the ISS orbiting the Earth, the gravitational forces are almost zero. In space, both intravascular and extravascular fluid shifts towards the head, leading to the characteristic “bird-legged and puffy faced” appearance of astronauts after extended periods in space. This has multiple, interrelated consequences – principally in the cardiovascular, nervous and ocular systems.Cerebral cephalad shift consequences
Microgravity exposure almost immediately raises intraocular pressure (IOP), and this may be explained by the cephalad shift causing vascular engorgement of the choroid. As the sclera remains rigid and does not expand as ocular volume rises, the consequence could be a rise in IOP. A rise in IOP has been well documented even with transient exposure to microgravity during parabolic flight (4). A cephalad fluid shift can lead to increased perfusion of the ciliary body and increased aqueous humor production. If you combine this with the fact that the fluid shift also causes venous system congestion (and as a consequence, also raises pressure within the episcleral vessels), you increase the resistance to aqueous humor outflow… raising IOP. But raised IOP is likely not the cause you’re looking for. The initial IOP spike on exposure to microgravity is soon followed by a decrease in IOP over the next few days, and it’s been hypothesized to be a result of a compensatory decrease in aqueous volume. Christian Otto, the lead scientist of NASA’s VIIP project, explained that, “so unconvincing have the IOP values been on the ISS, that Medical Operations has scrubbed regular IOP measurements from the Medical Requirements Integration Document, and no ISS crewmembers have experienced ocular hypertension”. The tonometer will likely be staying in its case then...If not IOP, then is raised ICP the culprit? ICP is the central feature of idiopathic intracranial hypertension (IIH), which serves as the closest terrestrial clinical equivalent. The elevated ICP that occurs with IIH on earth can cause many problems – the pressure increase can compress the sixth cranial nerve, resulting in problems with ocular abduction, double vision, and optic disc swelling, which can cause transient vision obscuration, which, if left untreated, can result in progressive and permanent vision loss. Cephalad fluid shifts are well known to cause jugular venous distention which suggests that cerebral venous congestion may occur during microgravity exposure. CSF is thought to be largely produced in the choroid plexus and drainage depends on a pressure differential between the CSF and the venous system. Thus a rise in venous pressure in the head and neck, produced by cephalad fluid shifts may cause impairment of CSF outflow, as well as cerebral venous congestion, both of which could lead to a rise in ICP not unlike that which occurs with IIH. However, what the astronauts are experiencing is not IIH. So far the ICP elevations seen in patients with IIH are far greater than that seen in the astronauts on the ISS, and the astronauts are spared the severe, disabling headaches that many of those with IIH suffer. Whatever is happening may have similarities to IIH, but it’s certainly a unique pathology with a unique etiology. Another possible explanation is that the disc swelling and optic nerve sheath expansion described during long duration space flight may result from localized elevation of optic nerve sheath pressure occurring at the level of the intraorbital optic nerve (i.e. optic nerve compartment syndrome) with or without a rise in ICP.
Floating in a tin can, far, far away
The ISS is a sealed environment, with little in the way of ventilation, and a typical crew of six, respiring, astronauts. Carbon dioxide removal systems are in place, but CO2 levels are still ten to twenty times greater on the space station (2.3–5.3 mmHg) than they are on Earth (~0.23 mmHg). Poor ventilation and microgravity can result in local pockets of elevated CO2 levels – like in the region around a sleeping astronaut’s mouth. If you remember your physiology classes, elevated atmospheric CO2 almost immediately raises ventilation and heart rates. It also results in cerebral blood vessels, increasing cerebral blood flow, CSF production and ICP.Salt and sweat
Astronauts have a pretty sodium-rich diet: more than 5 grams per day in some cases (something that NASA is currently trying to reduce by 40 percent), which can affect fluid balance, and potentially exacerbate the VIIP symptoms. On-board exercise has also been hypothesized to cause transient ICP elevations – either from the short-burst exertions involved in resistive exercise, or from the increased cerebral blood flow that results from a good aerobic workout.Not all men, not all women
Not all astronauts – even those on extended missions – experience problems, raising a number of questions. NASA believes that there is a “high probability that all astronauts have intracranial hypertension (IHT) to some degree” and that, in some astronauts, “if the IHT is not treated, there is a risk of damage to the optic nerve and possible reduced vision capability [in the] long term” (1,5). This means that once the initial IOP spike recedes, it’s likely that most astronauts will have higher ICP than IOP – imposing a subtle anterior force on the lamina cribrosa of the optic disc. Perhaps some astronauts simply adapt better than others. But why?Feeling the pressure and assessing the damage
NASA needed to know more: they required a non-invasive way of screening for retinal, choroidal and optic nerve abnormalities. Basically, they needed to perform a whole suite of health exams – both on Earth and in space (Figure 3) – to ascertain the astronaut’s eye health. A key part of these exams is optical coherence tomography (OCT).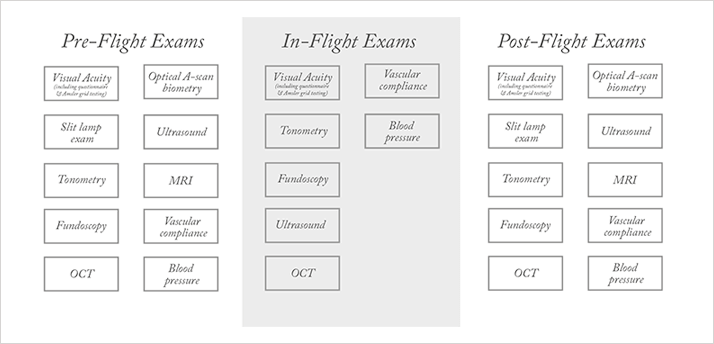
Spectralis ad astra
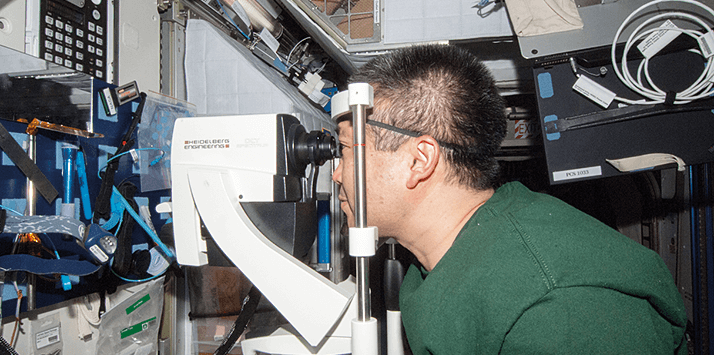
It’s one thing wanting to perform OCT imaging on the ISS. It’s quite another thing doing it. For a start, once you get a device, you have to get it up there. For Heidelberg Engineering, manufacturer of the Spectralis range of OCT instruments, it all started with a phone call, asking if they would like to work with NASA. They agreed – and the work began. Heidelberg Engineering’s Kester Nahen explains: “In February 2013, we took an off-the-shelf product and sent it to NASA. In April, they performed some tests on it, sent it on a parabolic flight for some microgravity tests, where they assessed how the instrument would work in microgravity, and then trained their staff to use it under those conditions.” It looked like the instrument could operate in microgravity conditions – but could it survive a rocket trip?As NASA was testing the Spectralis on the “vomit comet” back in Germany, Heidelberg Engineering’s staff were strapping a Spectralis to a shaking table, in order to see if the instrument could withstand the vibrations of a rocket launch. It seemed that it could; the Spectralis was ready for space. Kester’s colleague, Gerhard Zinser, explained the short timeline of these events: “On June 5, it was launched into space on an Ariane 5 rocket from the European Spaceport in Kourou, French Guiana. It reached the ISS on June 15, was unpacked on June 18, and on June 21, the first OCT image was taken in space – of a test target.” The next step for NASA was to set up the satellites to stream the images down to Houston, Texas, where a team of experts on the ground could remotely guide the astronauts through the procedure. On October 16, the first crew examinations were performed over live video streaming.
Snapshots from space
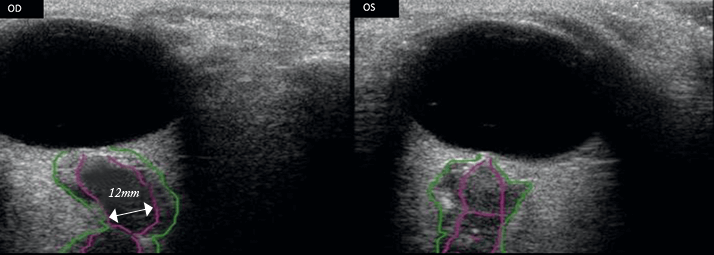
Nimesh Patel, an Assistant Professor at the University of Houston, College of Optometry and a consultant to NASA reported some early data obtained from four astronauts by in-flight OCT earlier this year (6), explaining in some detail how NASA’s VIIP program utilizes in-flight OCT to ascertain retinal changes in a microgravity environment. Patel described how all astronauts underwent a battery of pre-flight ocular tests to set a baseline, including OCT, and that during the mission, the astronaut operating the instrument could use Spectralis’ auto-rescan function to ensure that images captured in space were from same region of the retina that was imaged on Earth. He revealed that confocal scanning laser ophthalmoscopy (cSLO) and OCT images showed that some astronauts had developed retinal and choroidal folds during their time on the ISS – pathologies that were not present at the pre-flight, baseline assessment back on Earth. Microgravity-induced hyperopic shift affects half of all astronauts, and infrared (IR)-SLO imaging managed to document the development of this – Patel noted that a progressive decrease of the apparent size of retinal structures being scanned by the instrument was observed in those experiencing hyperopic shifts.Pathological changes in the optic nerve head (ONH) were also observed during the mission. Star pattern OCT scans, centered on the opening of Bruch’s membrane, revealed that space flight can increase the Bruch’s membrane opening minimum rim width (BMO-MRW) in some astronauts by up to 70 µm, and post-mission assessments showed that the BMO-MRW can remain increased even after the astronauts return to Earth. Furthermore, OCT circle scans of the peripapillary architecture also revealed that the retinal nerve fiber layer and the choroid thicken during the mission, and again, remained thickened after the mission. NASA is not stopping at OCT imaging – the next ophthalmic imaging device to go to the ISS will be a Scheimpflug camera that will enable astronauts to quickly and easily measure IOP, corneal thickness and biomechanics – with Oculus’ Corvis ST camera already having demonstrated its utility in microgravity, during two “vomit comet” flights earlier in June this year.
Mitigating against microgravity
To date, the causative mechanisms underlying the pathological changes are still unknown – no definitive proof yet exists, despite theories relating to microgravity-induced cephalad shifts being compelling. Some of the ocular changes are dealt with easily: shifts in visual acuity are remedied with corrective lenses. But the changes to the retina and ONH are less easily resolved. One possibility is acetazolamide (3). It’s used for the treatment of glaucoma and idiopathic intracranial hypertension, and helpfully reduces cerebrospinal fluid production, and with it, ICP. Another possibility is actively trying to minimize the effects of cephalad fluid shifts. In the absence of artificial gravity – which is still within the realm of science fiction – interventions like thigh cuffs and lower-body negative pressure suits (Figure 4) may help prevent or treat these spaceflight ocular disorders (3). But fundamentally, a better understanding of how microgravity affects the eye – and why only some astronauts are affected – is central to developing effective treatment and prophylaxis. It’s also central to letting a long-duration space mission proceed.
References
- National Aeronautics and Space Administration: Human Research Program, Human Health Countermeasures Element, “Evidence Report: Risk of spaceflight-induced intracranial hypertension and vision alterations”, July 12, 2012. Available here. Accessed July 28, 2014.
- T.H. Mader. C.R. Gibson, A.F. Pass, et al., “Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight”, Ophthalmology, 118, 2058–2069 (2011). doi: 10.1016/j.ophtha.2011.06.021.
- K. Marshall-Bowman, M.R. Barratt, C.R. Gibson, “Ophthalmic changes and increased intracranial pressure associated with long duration spaceflight: An emerging understanding”, Acta Astronautica, 77–87 (2012). doi: 10.1016/j.actaastro.2013.01.014.
- T.H. Mader, C.R. Gibson, M. Caputo, et al., “Intraocular pressure and retinal vascular changes during transient exposure to micro-gravity”, American Journal of Ophthalmology, 115, 347–350 (1993).
- NASA Human Research Roadmap, “Risk of spaceflight-induced intracranial hypertension/vision alterations”, Accessed July 30, 2014.
- N. Patel, “Heidelberg Engineering Xtreme Research Lecture Award (2014)”, Accessed July 28, 2014.
