By Osamah J. Saeedi, Professor in the Department of Ophthalmology and Visual Sciences, Director of Clinical Research; Director of the Glaucoma Division; and Vice Chair for Academic Affairs, University of Maryland School of Medicine, Baltimore, Maryland, USA
Case presentation
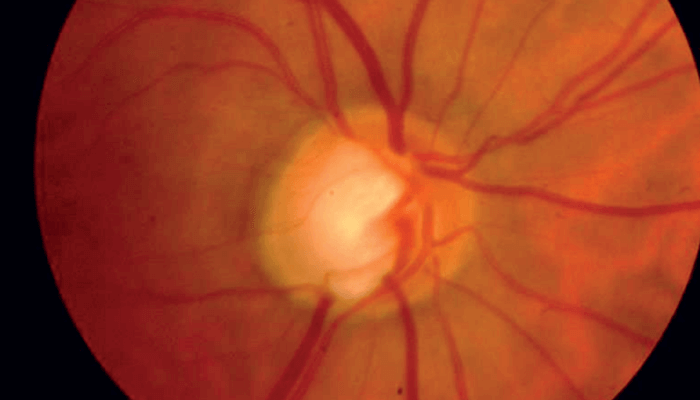
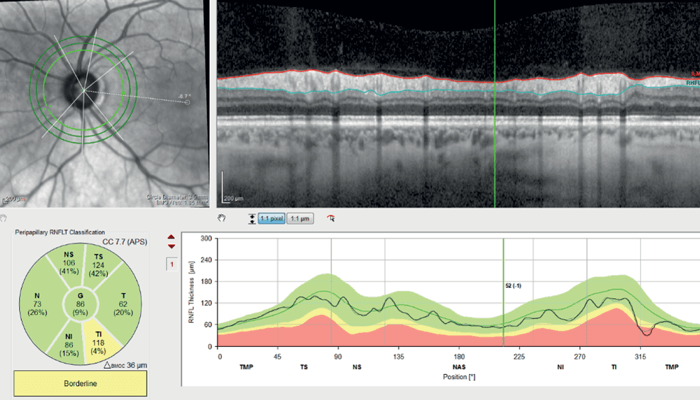
A 57-year-old Caucasian woman with a longstanding history of glaucoma and significant visual field loss in her right eye presented with treated intraocular pressures in the high teens. Her visual field in the right eye showed a deep superior paracentral defect close to fixation, and the left eye showed scattered defects but was grossly normal. Dilated fundus examination on the right eye revealed a cup to disc ratio (C/D) of 0.7 with an inferior notch, and on the left eye a C/D of 0.6 (see Figure 1).

Use of optical coherence tomography (OCT)
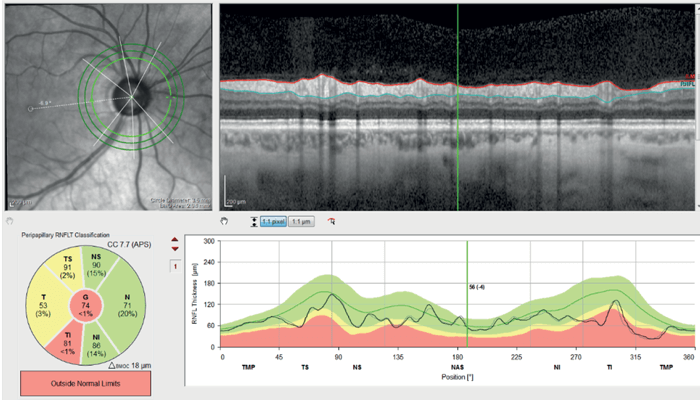
Optical Coherence Tomography Retinal Nerve Fiber Layer (OCTRNFL) with the SPECTRALIS platform (Heidelberg Engineering) revealed temporal thinning in the right eye, more in the inferotemporal quadrant (see Figure 2). Glaucoma causes retinal thinning and asymmetry in the macula (specifically in the ganglion cell layer), so we assessed OCT Macula which revealed relative asymmetry and thinning inferiorly (see Figure 3). Ganglion Cell Layer segmentation revealed generalized thinning and asymmetry between the superior and inferior hemifield.
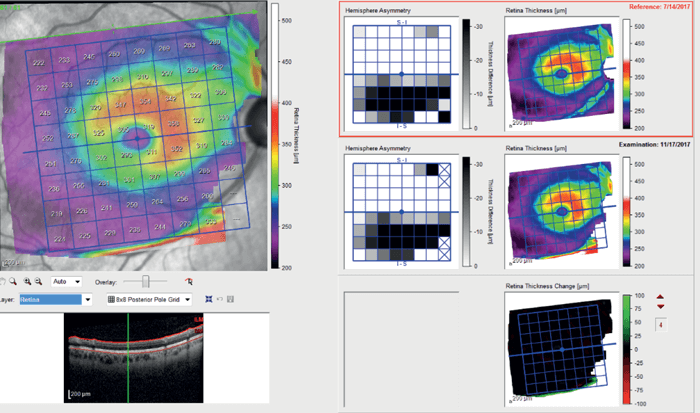
OCT-RNFL in the left eye showed only mild thinning inferotemporally (see Figure 4) and OCT Macula showed asymmetry of retinal thickness with inferior thinning (see Figure 5).
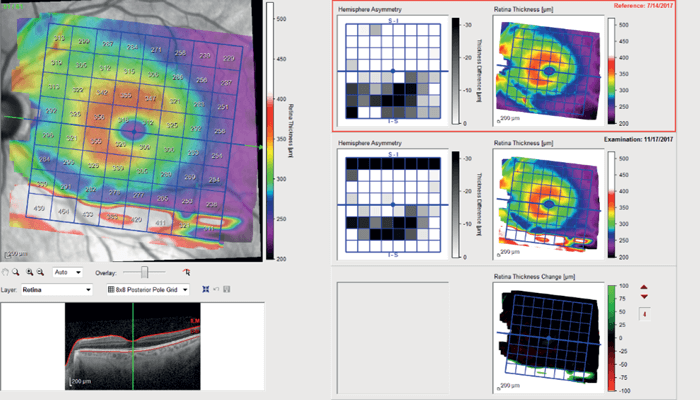
Given the RNFL thinning, macular asymmetry and visual field defects, we recommended aggressively lowering the IOP in the right eye with a low target. In the left eye, given the mild structural changes with normal visual field, it was unclear whether aggressive IOP lowering was required.
Use of optical coherence tomography angiography (OCTA)
As OCTA might be a marker of early disease that precedes RNFL thinning, we employed the SPECTRALIS OCT Angiography Module to further pinpoint the disease severity in the left eye and guide management.
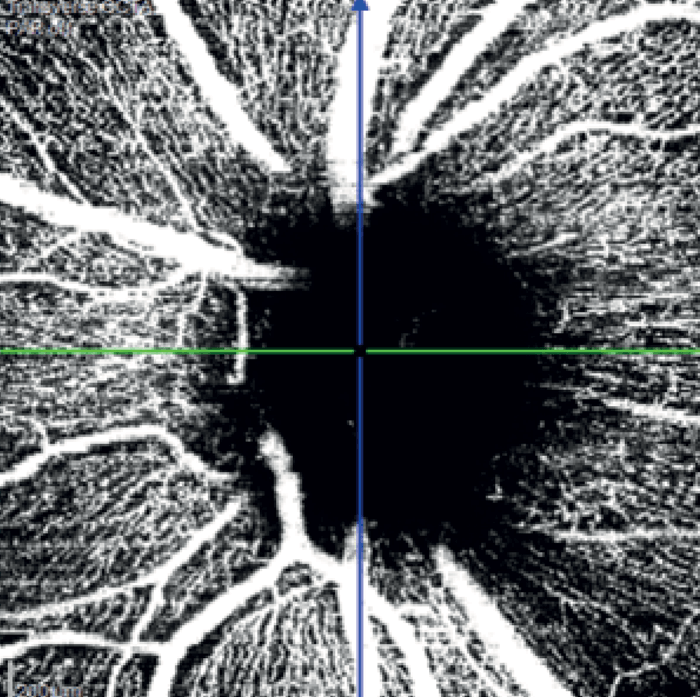
A wedge-shaped defect and inferotemporal thinning of the RNFL in the right eye corresponded with OCTA of inferotemporal capillary dropout (see Figure 6). OCTA of the Macula revealed diffuse capillary dropout inferiorly consistent with retinal thinning (see Figure 7). These dramatic images matched the paracentral visual field deficit in the right eye.
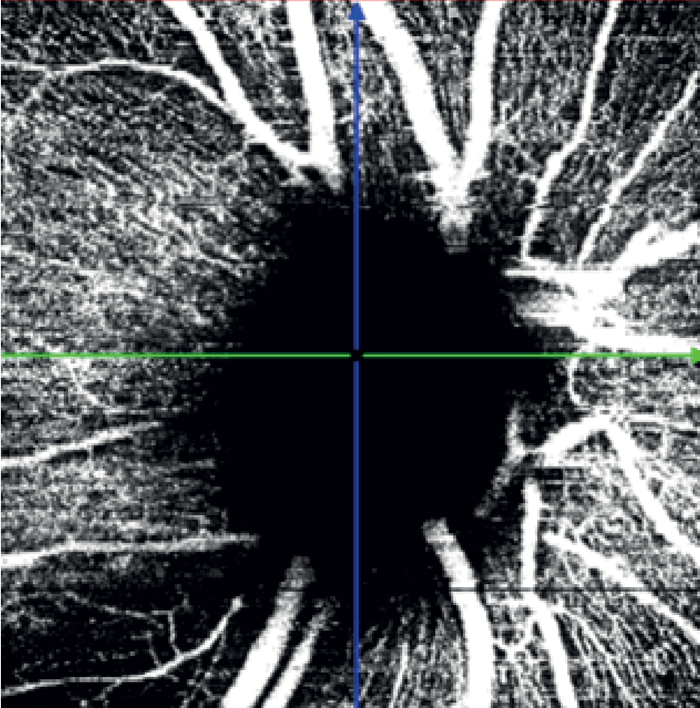
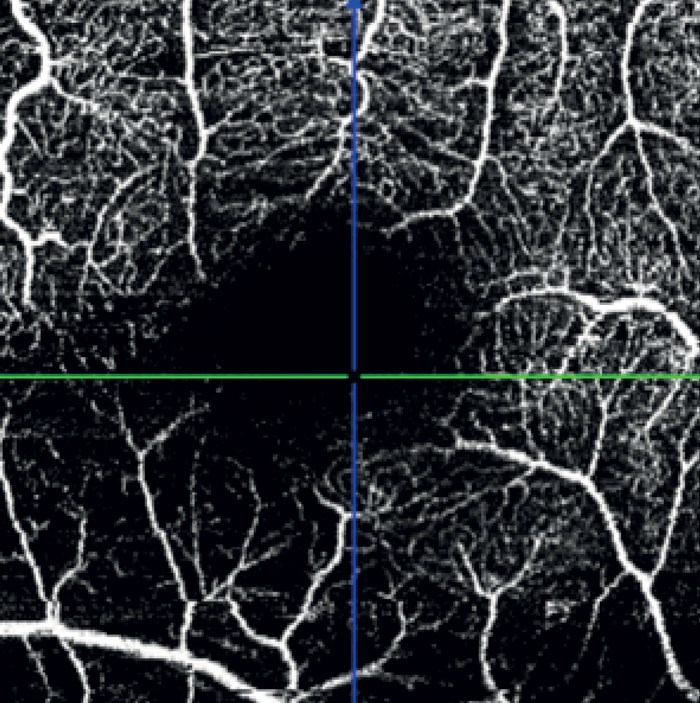
In the left eye – which had a mild inferotemporal RNFL thinning and a normal visual field – SPECTRALIS OCT Angiography revealed a wedge defect and corresponding profound capillary dropout around the optic nerve head (see Figure 8). This corresponded to capillary dropout in the inferior macula (see Figure 9).
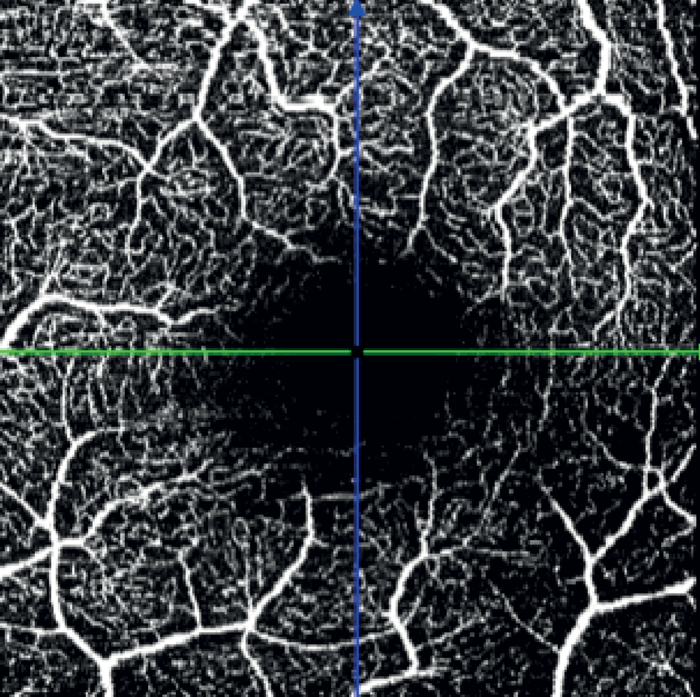
Given the profound loss of vessel density as seen on OCTA in the left eye, an aggressive target IOP was set.
Discussion
In this patient – with severe disease in the right eye and seemingly mild glaucoma in the left eye – SPECTRALIS OCT Angiography Module revealed vascular changes that may precede RNFL thickness changes and visual field deficits. This important information helped to guide treatment in this case. OCTA is helpful in assessing the potential for further risk of progression and identifying patients that may need to be treated more aggressively.
