Corneal collagen cross-linking (CXL) with UV-A illumination and riboflavin is a useful way of increasing corneal stiffness to halt the progression of corneal ectatic disorders like keratoconus. But there’s still much to be learned about the cellular and molecular events that take place during CXL and afterwards – and plugging those gaps in knowledge has been difficult. Ex vivo testing fails to provide an accurate picture because hydration and preservation processes after enucleation change the properties of the tissue and affect the accuracy of the testing, and to date, only indirect (and often inaccurate) methods of determining the efficacy of CXL in vivo exist. But change is afoot; a group of Swiss researchers led by Farhad Hafezi have tackled the problem by successfully establishing a CXL procedure, in vivo, in mice and then developing tools to accurately measure biomechanical changes in the mouse cornea that are induced by the procedure (1).
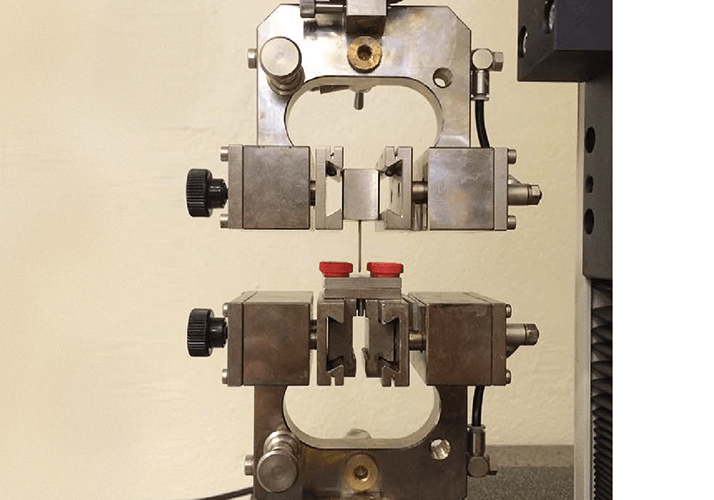
They achieved this by performing CXL with riboflavin on two groups of mice: the first group was used to determine appropriate adaptation of human CXL parameters to the mouse cornea (which is about five times thinner than a human cornea); the second group of mice underwent CXL, but the UV-A fluence was reduced consecutively (from 3 mW at 3 mins, to 1 minute, to 30 seconds) in order to determine the threshold fluence level for effective CXL in the mouse cornea. After treatment, the mice were sacrificed and their corneas harvested for two-dimensional biomechanical testing using a customized corneal holder, designed to accommodate the small corneas of mice (see Figure 1).
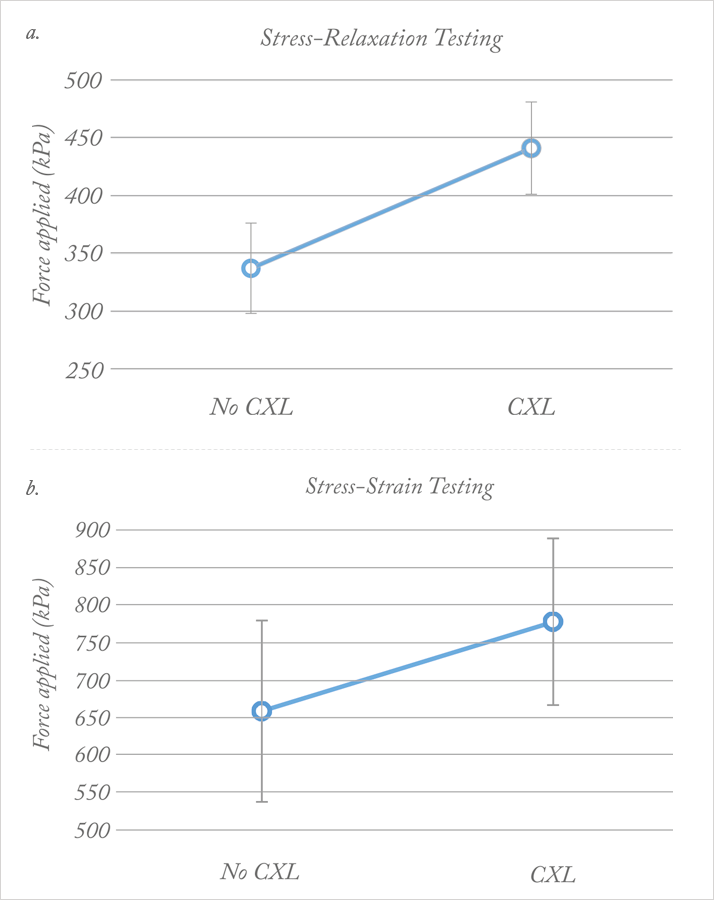
The biomechanical analysis involved three steps: 1. preconditioning with three stress-strain cycles, 2. two minutes of stress-relaxation testing (in which constant force was applied to the cornea and the decrease in stress recorded), and 3. stress-strain extensometry (in which increasing force was applied until the cornea broke). In all cases, stress-relaxation analysis showed significant biomechanical differences between the corneas of mice who received CXL with riboflavin, and those who did not. Cross-linked corneas maintained a higher stress (see Figure 2a) after 120 seconds of constant strain – meaning that they possessed greater structural integrity than non-cross-linked corneas. The findings were confirmed by stress-strain analysis (see Figure 2b), though the team found that this test was less sensitive to CXL-induced changes. Overall, they reached two main conclusions: that two-dimensional extensometry testing more closely mimics natural conditions than previous (one-dimensional) tests on pig, rabbit and human corneas, and that stress-relaxation testing provides a clearer measure of differences between groups than the more standard stress-strain testing. Combining these new discoveries with the establishment of mice as a useful model for CXL testing opens up new opportunities to examine the molecular effects of cross-linking in a living organism – particularly with transgenic mice.
References
- A Hammer, et al., “Establishing corneal cross-linking with riboflavin and UB-A in the mouse cornea in vivo: biomechanical analysis”, Invest Ophthalmol Vis Sci, 56, 6581–6590 (2015). PMID: 26465887.
