It is common for ophthalmic patients to need input from clinicians specializing in more than one area. When coexisting conditions can be treated by one surgeon in a single procedure, time and money are saved and visual outcomes and IOP lowered at the same time – greatly benefiting patients.
Fritz Hengerer, Director and Chief Medical Officer at the Department of Ophthalmology at Buergerhospital Eye Clinic in Frankfurt, Germany, explains the benefits of linking cataract procedures with glaucoma treatment. “The conditions themselves are often linked in real life: in my own practice, about 15 percent of cataract patients also have glaucoma or ocular hypertension. And in addition, cataracts can interfere with glaucoma diagnosis; for example, lens opacification impedes retinal imaging and ophthalmoscopic evaluation of the optic disc and cataracts’ effect on visual acuity can make perimetric evaluations unreliable. Therefore, it is helpful to address both cataracts and glaucoma as part of a single clinical management strategy – and, now that safe and effective trabecular micro-bypass devices (such as iStent inject® W) are broadly available, we can do exactly that. If it is possible to address both cataracts and glaucoma symptoms within a single procedure, at a relatively early stage, why not do so? It just makes sense.”
Karsten Klabe, ophthalmic surgeon at Breyer, Kaymak & Klabe Augenchirurgie in Düsseldorf, Germany, agrees with this view. “Perhaps the major advantage of iStent technologies is that it allows us to offer both a solution for cataracts and an effective glaucoma treatment within a single surgical episode. iStent inject® W combines elegantly with cataract surgery – the only additional requirements are viscoelastic and a gonioprism. You don’t need another assistant or additional sophisticated devices – you just put a gonioprism on your operating table and that’s it! Also, the time demands of the procedure are acceptable.”
Have surgeons noticed any advantages to using the iStent technologies for combined procedures during the COVID-19 pandemic? Imran Masood, Consultant Ophthalmic Surgeon, Birmingham and Midland Eye Centre, UK, offers his perspective. “Some patients whose cataracts might have gotten worse over the first months of the pandemic, when cataract procedures were cancelled, have noticed their visual function deteriorating at a time when they rely on their vision for tasks that keep them occupied at home. Combining cataract and iStent inject® surgery has allowed me to improve those patients’ vision at the same time as getting their pressure under control, preventing deterioration of their glaucoma and improving their ocular surface, which has been welcomed by my patients.”
Fritz Hengerer concludes, “Surgeons should consider the benefits of combining cataract surgery with iStent inject® W implantation. Advantages for the surgeon include time and cost savings; advantages for the patient include a single surgery experience, a single anesthesia, and a single postoperative appointment for both glaucoma and cataract treatment. Thus, integration of iStent inject® W into cataract surgery for glaucoma patients allows us to kill two birds with one stone.”
iStent inject® W case study
Anshoo Choudhary, glaucoma specialist and Consultant Ophthalmologist at the Royal Liverpool University Hospital, Liverpool, UK, presents a case study of a patient with progression of primary open angle glaucoma despite triple therapy.
Zhihang Cheng, Ophthalmology specialty trainee at the Mersey Deanery, with an interest in glaucoma and minimally invasive glaucoma surgery research.
Patient
A 72-year-old man referred by a local eye department with open angle glaucoma progression.
Initial examination
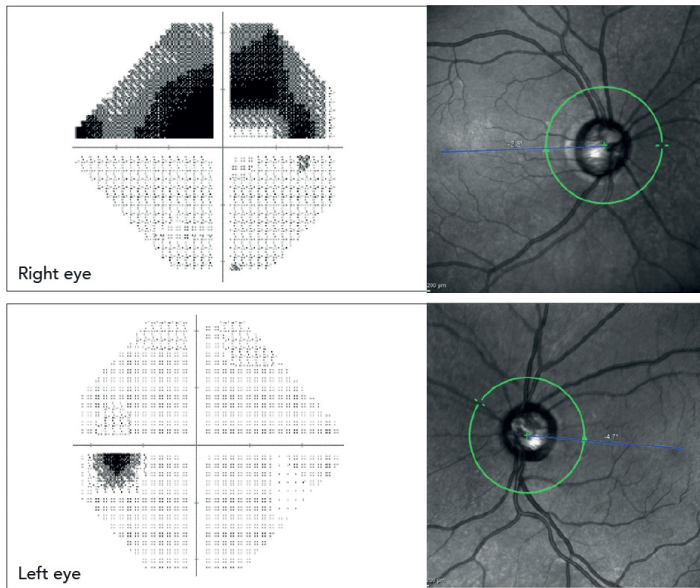
Right eye: A significant cataract
Advanced cupping: cup-to-disc ratio 0.9
IOP, with topical therapy: 16 mmHg
Visual field: advanced changes with a mean deviation of -11.89 dB
Left eye: A significant cataract
Moderate glaucoma: cup-to-disc ratio 0.75
IOP, with topical therapy: 15 mmHg
Visual field: early changes with a mean deviation of -1.54 dB
First procedure and subsequent therapy
The patient underwent a cataract surgery and deep sclerectomy (DS) to reduce the IOP in his right eye, which was kept on monotherapy following the surgery to maintain target IOP. His left eye was kept on dual therapy and the IOP remained in the high teens. Eye drop intolerance limited his ability to receive additional ocular hypotensive agents. There were also concerns regarding possible visual field progression.
Combining cataract surgery with iStent inject® W
Two years since the initial referral, the patient reported worsening vision consistent with symptoms of cataract in the left eye. Surgical options discussed with him included a standalone cataract procedure or a combined procedure with iStent inject® W to reduce his left-eye IOP. Taking into consideration the potential benefit of better pressure control and reduction of drop burden, the patient opted to have a combined procedure.
Results of the combined procedure
At three months post-op, his IOP was 12 mmHg in the left eye without drops, and disc appearance was stable. Twelve months post-procedure, the patient’s left-eye IOP remained stable at 13 mmHg with a stable visual field (mean deviation -0.94).
Conclusion
The iStent inject® W is a Trabecular Micro-Bypass glaucoma procedure which is designed to restore outflow of aqueous humour through the physiological outflow pathway. The landmark randomised control trial showed more than 75 percent of patients achieve a 20 percent reduction in IOP and in some patients the IOP reduction may be greater. With proven safety and efficacy, it is an attractive option as a combined procedure for patients with mild to moderate glaucoma who are undergoing cataract surgery. Early intervention and improved IOP control might have the added advantage of avoiding filtration surgery in these cases.
References
- TW Samuelson et al., “Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract,” Ophthalmology, 126, 811 (2020). PMID: 31973839.
