We have been involved in studies of two innovative approaches to overcome the challenges of transepithelial cross-linking (CXL). At present, epi-off CXL remains the gold standard in most of the world, but many of us find it worthwhile to continue investigating new techniques for epi-on – or transepithelial – CXL in search of a safe and effective way to offer patients a shorter procedure, faster recovery (without the lengthy process of epithelial remodeling), less pain and lower risk of infection.
Iontophoresis CXL (I-CXL) has been CE-marked in Europe for some time. I-CXL uses a positive electrical charge to facilitate penetration of a negatively-charged, dextran-free 0.1 percent riboflavin solution (Ricrolin, SOOFT Italia) through the epithelium into the stroma. 10 mW/cm2 ultraviolet light is applied with I-ON CXL device (SOOFT Italia).
Early on, we tested the technique in rabbits. Iontophoresis allowed riboflavin diffusion with a much lower concentration of riboflavin than in conventional procedures, and I-CXL resulted in similar corneal stiffening to conventional CXL (1).
In published, clinical studies, there have been positive results from several randomized, controlled clinical trials demonstrating clinically significant topographic, visual and refractive improvements with I-CXL (3). Some have found that removing the mucin layer prior to iontophoresis is helpful. Compared with standard CXL, the procedure seems to have more refractive effect, but less effect on Kmax, especially in younger patients.
Most recently, a group of researchers reporting on three-year follow-up of 40 pediatric eyes found that standard epi-off CXL halted progression in 75 percent of cases, compared with a slowing down of progression in only 50 percent of the eyes treated with I-CXL (4). There have also been some reports of significant patient discomfort (5). This study and others have shown that I-CXL is not as efficient as standard epi-off CXL and needs to be improved.
Another recent innovation in transepithelial CXL is the addition of supplemental oxygen to increase the efficiency of the riboflavin-UVA reaction. As part of a multicenter European clinical trial, I have treated 34 eyes with progressive keratoconus (defined as Kmax progression >1 D in one year).
During this procedure, we gently clear the surface mucin layer of the tear film. Two different riboflavin solutions are employed. First, two drops of 0.25 percent riboflavin and benzalkonium chloride is applied every minute for four minutes, followed by two drops of the 0.22 percent riboflavin every 30 seconds for six minutes.
After both riboflavin solutions have been applied, Boost goggles (Avedro) are positioned over the patients’ eyes so that oxygen flows over the surface of the cornea. Once the surface oxygen concentration reaches 90 percent, pulsed UV irradiation at 30 mW/cm2 is begun, for a total dose of 10 J/cm2.
Finally, the cornea is rinsed with balanced saline solution, and a bandage contact lens is placed on the eye. We don’t yet have final data but will be presenting our six-month results at ESCRS.
In one recent case in the supplemental oxygen study, a 23 year-old male patient was being followed at our clinic for suspected bilateral keratoconus (Stage 1 of the Krumeich classification). Noting that the patient had a 1.0-D change in Kmax over a seven-month period, we decided to cross-link. The patient agreed to enter the transepithelial/supplemental oxygen study based on hoped-for improvement in comfort during and after the procedure.
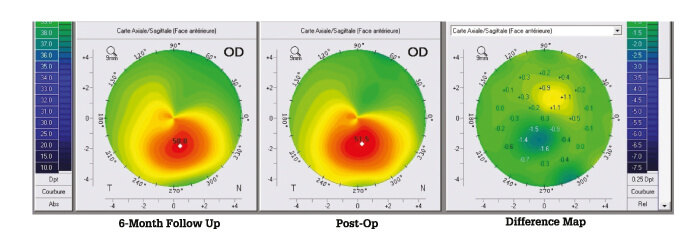
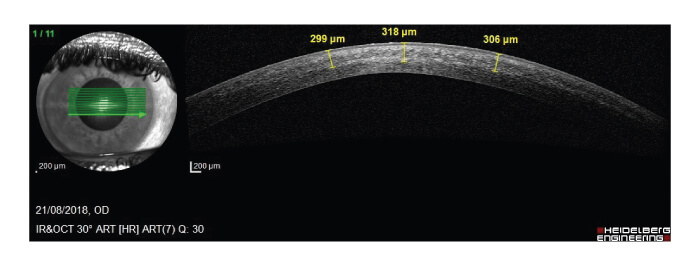
Cross-linking was performed without any issues or adverse events. Two days postop, the patient had some moderate pain, foreign body sensation and photophobia, which resolved in the first week. The epithelium was intact, with mild superficial punctate keratitis at day two. There was transient haze between one and three months, without vision loss. At six months, the patient was satisfied with the result. The visual acuity was unchanged; corneal changes are shown in Figure 2.
In conclusion, there are several promising efforts to improve upon transepithelial cross-linking techniques. I-CXL techniques may improve visual acuity, but may be less effective than epi-off CXL at halting the progression of Kmax. The addition of supplemental oxygen to epi-on procedures is a new innovation with promising early results.
Though it is too soon to say whether these efforts will elevate epi-on procedures to the same standards as epi-off, clinicians should continue to follow the results of clinical trials with great interest.
References
- M Cassagne et al., “Iontophoresis transcorneal delivery technicque for transepithelial corneal collagen crosslinking with riboflavin in a rabbit model”, Invest Ophthalmol Vis Sci, 57, 2, 594 (2016). PMID: 24644053.
- M Lombardo et al., “Randomized controlled trial comparing transepithelial corneal cross-linking using iontophoresis with the Dresden protocol in progressive keratoconus”, Ophthalmology, 124, 6, 804 (2017). PMID: 28283279.
- M Lombardo et al., “Two-year outcomes of a randomized controlled trial of transepithelial corneal crosslinking with iontophoresis for keratoconus”, J Cataract Refract Surg, 45, 7, 992 (2019). PMID: 31003798.
- L Buzzonetti et al., “Iontophoretic transepithelial collagen cross-linking versus epithelium-off collagen cross-linking in pediatric patients: 3-year follow-up”, Cornea, 38, 7, 859 (2019). PMID: 31026242.
- S Taneri et al., “Evaluation of epithelial integrity with various transepithelial corneal cross-linking protocols for treatment of keratoconus”, J Ophthalmol, 614380 (2014). PMID: 25197559.
