
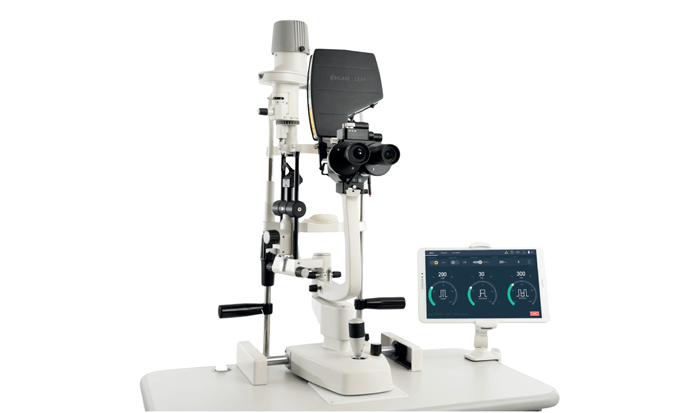
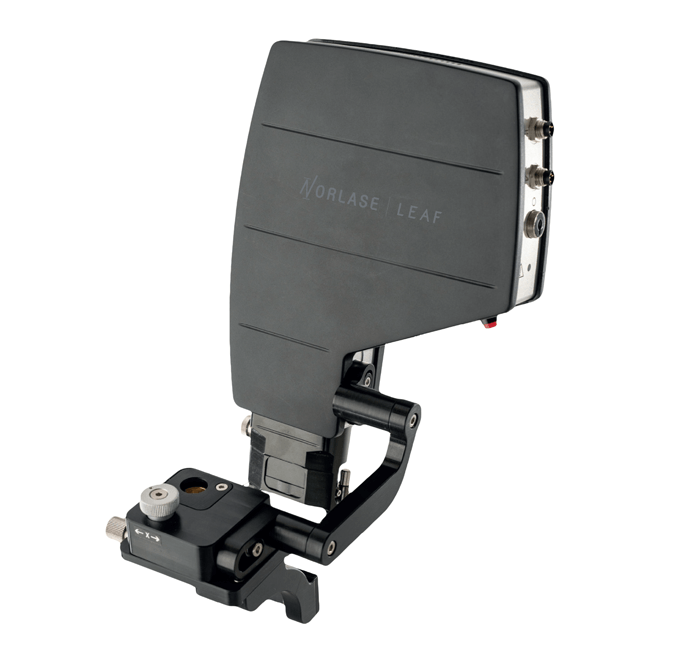
At one-tenth the size of competing systems, Norlase’s ultracompact photocoagulator is light, portable, and small enough to sit directly on the slit lamp. The laser device’s advanced features include voice control and microsecond energy pulsing. Is it time for surgeons to broadly employ this value-for-money device? We asked Giovanni Staurenghi, Professor of Ophthalmology, Chairman of the University Eye Clinic, and Director of the University Eye Clinic Department of Biomedical and Clinical Science at Luigi Sacco Hospital in Milan, Italy…
What are your current interests and specialties?
I’m a retinal specialist, but – as it is usually practiced in Italy – I cover everything from cataracts to orbits! In terms of academic and clinical research, however, I can and do focus on the retina, and in particular on the treatment of AMD, diabetes-related retinopathy and inherited retinal disease. I also have a strong interest in improving imaging techniques to permit better differential diagnoses for my patients. There have been many changes to the diagnosis and management of retinal disease over the last decade, and I am proud to have contributed in this field. In particular, I was involved in combining laser treatment with angiography: this approach exploits the ability of indocyanine to absorb the near-infrared wavelengths of standard laser light. Of course, attitudes to this approach have changed over the years, and there is now a general feeling that laser treatment is damaging.
What lasers do you use in your practice?
We use a variety of systems, from the old argon lasers to the new 532-nm instruments and yellow lasers. And now we are experimenting with Norlase – this is a new system, but it is based on the green laser that we are familiar with. Our experience is that the Norlase instrument is very practical and easy to use – we are extremely happy with it.
Tell us more about your impressions of LEAF…
We use LEAF for cases of AMD, diabetic retinopathy, central vein occlusion, and retinal holes or breaks in the periphery. It is perfect for treating the posterior and periphery, which is not granted in many other lasers. It’s an excellent addition to our practice: the alignment is always easy to calibrate, and it is very easy to use. Furthermore, it has the benefit of familiarity: it uses a green laser, which is absorbed by melanin, and is therefore similar to the 532-nm system ideal if you are targeting the retinal pigment epithelium.
We are working on a small study to compare green, yellow, and Norlase laser systems.
What are the main benefits of LEAF?
One of the instrument’s major advantages is its portability – it’s hard to believe that the Norlase system can be contained in such a small box! This has a number of benefits – for example, private practitioners who work from many different clinics can carry the laser with them from one office to another. There are other useful features, too, for example voice control, though this is probably most relevant for native English speakers who pronounce words in a way that the system can easily recognize. But that is more of a nice-to-have than an essential addition, because Norlase is easy to adjust without recourse to the voice control feature. In summary, the LEAF instrument is extremely well-balanced, and clearly designed with convenience in mind.
Is LEAF simple to adopt?
Very much so. It took my team almost no time to become familiar with the system and adept in its operation. Of course, new users will always benefit from some technical guidance, but the bottom line is that LEAF really is very simple to learn.
Are you happy with LEAF outcomes?
Yes – my experience of using LEAF is successful treatment, time after time. The only problem we have come across is not related to the Norlase system itself, but rather is the fault of the ophthalmology community, in that we no longer effectively teach younger residents and specialists to use lasers in the most effective way. This is a consequence of the attitude change over the last decade that I noted before. For example, in polypoidal vasculopathy, where anti-VEGF treatment usually results in only an incomplete response, we should encourage surgeons to use a laser directly on the polyps when those are not under the fovea. My view is that we really need to see more laser use in regular AMD management.
Any final thoughts?
What I would say to retinal specialists who haven’t yet tried LEAF is that there’s no need to hesitate – you’re getting exactly the same laser that you are used to, except with big advantages in portability and ease of use.


