- The introduction of trifocal and low add multifocal IOLs (mIOLs) means that cataract/refractive surgeons can now offer IOLs that give good intermediate vision
- One, if not the most important factor is patient satisfaction. Glare and halo are potential complications – but some patients are more bothered by them than others
- We report on a study that used the Heidelberg DATE score to assess patients’ satisfaction and ability to perform daily tasks after AT LISA tri 839MP mIOL implantation: overall, patients were very satisfied
- A full understanding of patients’ needs and how much they might encounter glare and halo (e.g. night driving) and how much that will bother them is key to offering them the right mIOL that will make them happy with their postoperative vision
The introduction of trifocal intraocular lenses (IOLs) to the market in 2011 changed what many ophthalmologists’ think what “functional vision” actually means. Before, intermediate vision wasn’t really given much attention; it was so low on many people’s radar that many studies didn’t even test it; the mindset was near vision and far vision. But now that trifocal and low-add multifocal IOLs (mIOLs) have hit the market, things are changing. Now that we can offer a variety of trifocal IOLs to patients, we’re having to think harder about finding the right IOL for them. This involves thinking about our own daily experiences and individual vision distances as reference points, and asking our patients about theirs, in order to find each person the right mIOL for their needs.
Fulfilling patients’ needs is more than just giving them great distance, near and intermediate vision under a range of lighting conditions – it turns out that this isn’t enough on its own. Patient satisfaction with their postoperative vision should be paramount. No one will ever explant a mIOL in a satisfied and happy patient, even if they have functional vision that’s much lower than average. On the other hand, we’ve all had to explant mIOLs in unhappy patients, some of whom have had great functional results from the doctor’s point of view, but were never satisfied with their own vision.
Asking the right questions
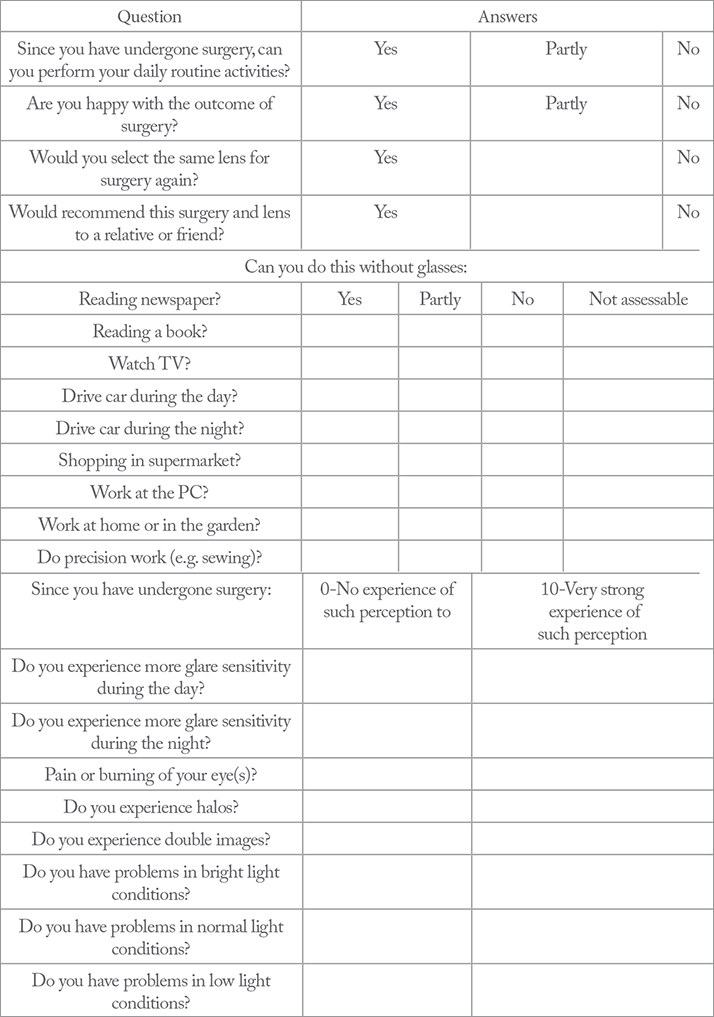
There are multiple questionnaires available (1,2) to help us look more closely into patient satisfaction, but they are often time-consuming and I believe that they don’t ask the right questions. Ulrich Mester and his colleagues recently published a paper discussing the impact of personality characteristics on patient mIOL satisfaction (3) in 180 patients implanted with different mIOLs – finding that four psychometric parameters had a significant effect on patient satisfaction: “compulsive checking” – that is, the need to perform repeated checks (on anything from door locks to news headlines) to calm obsessions; orderliness, competence and dutifulness. These four parameters correlated, not directly with patient contentment, but with the perception of glare or halos, which in turn translated to a likelihood of postoperative dissatisfaction.In our study, we wanted to demonstrate the effect of personality in “compulsive checkers” on satisfaction in a smaller cohort of 52 patients, who all underwent cataract surgery or refractive lens exchange with implantation of an AT LISA tri 839MP mIOL (Carl Zeiss Meditech, Jena, Germany) for the correction of aphakia and presbyopia. We used the DATE (DAily Tasks Evaluation) score – a questionnaire developed at the International Vision Correction Research Centre (IVCRC) of the Department of Ophthalmology, University-Clinic Heidelberg, Germany – to provide a quick method for evaluating patients’ satisfaction and ability to perform daily tasks. The scoring tool consists of 28 questions; three are yes-or-no, 11 can be answered with yes, partly or no, and the remainder offer a scale from 0 to 10, where 0 indicates no problem or influence and 10 indicates a severe problem or significant influence (see Table 1).
The patients’ replies
Figures 1a shows patients’ self-reported results for question 1 (“Since you have undergone surgery, can you perform your daily routine activities?”) and Figure 1b shows the results of question 2 (“Are you happy with the outcome of the surgery?”). Almost all patients (96 percent) replied positively to the first question, with none saying no; to the second, most (83 percent) said yes, with the vast majority of the remaining population replying “partly.” All patients said that they would select the same mIOL model again and would recommend the AT LISA tri 839MP to a friend or relative. They’re pleased with their vision for detailed work, too; 64 percent no longer needed glasses to read the newspaper, 58 percent did not require them to read books, and 38 percent did not have to rely on them for precision tasks (Figure 2) like knitting. Furthermore, there was a significant positive correlation between the binocular uncorrected near visual acuity and the near tasks results, and more than half of our patients were always able to work at the computer without glasses after the mIOL implantation procedure, with only 8 percent unable to do so even part of the time (see Figure 2).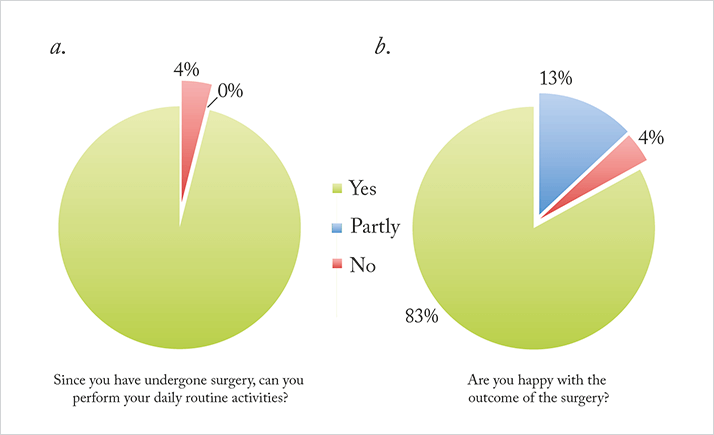
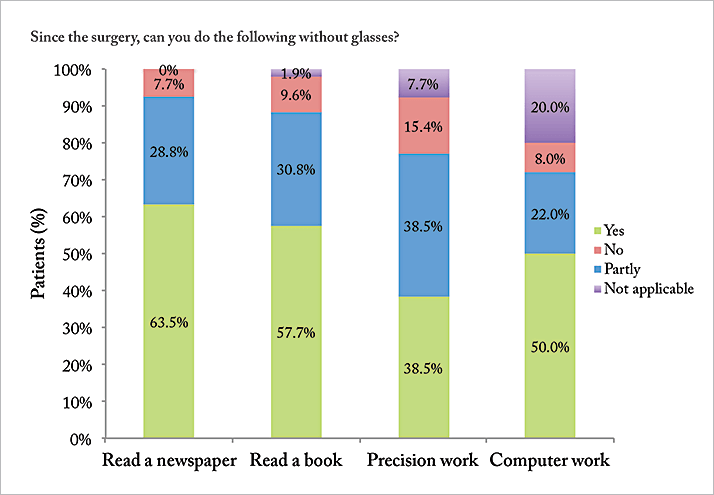
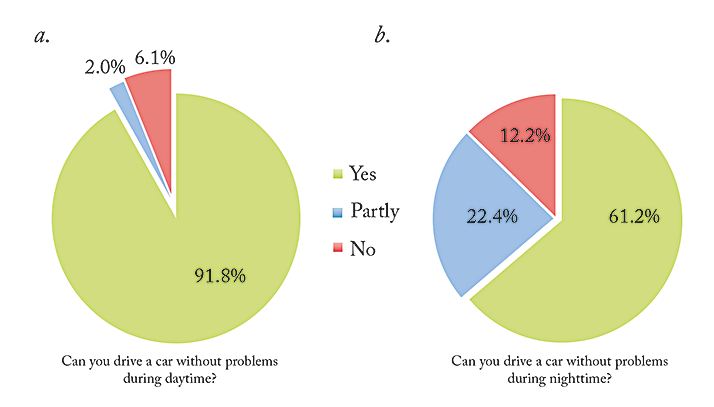
Figure 3 gives an indication of disturbances the patients experience during daytime and nighttime driving. We found a statistically significant correlation between spectacle independence and impairment caused by halos or by increased glare sensitivity during driving. During daylight driving hours, there was no significant association between binocular uncorrected distance visual acuity and glare. For distance vision, 90.4 percent of our patients said that they no longer needed to use spectacles. Median DATE scores (standard deviation) performing tasks that require near, intermediate and distance vision were 2.3 (2.81), 2.5 (2.12) and 3.0 (2.82), respectively.
Adverse events related to mIOLs implantation were minimal. Patients generally experienced very low levels of pain and discomfort after implantation, with a median ranking of 2/10 and a mean of 3.8/10 on the DATE scale. For double image perception, patients reported a median and mean values of 1/10, and 3.8/10, respectively. When we looked at the glare component of the DATE scale, we found that the amount of glare reported in lower light was significantly higher, with values distributed equally throughout day and night. Though patients were able to perceive halos and glare, they all stated that they experienced little to no impairment of daily life – and even with these aberrations, they preferred the convenient lifestyle they had after mIOL implantation to their previous lifestyle with glasses. One patient said, “I don’t know if anyone can imagine how it feels to wake up and not see. Everything is blurry. […] For me, those times are over. I wake up and I can see my husband beside me. It was weird not having to look for my glasses, but now it feels so much better being free and seeing what is around me.” In general, patients have no problems with visual disturbances under normal light conditions – and even under especially bright or low light, they report very few issues. I believe our results demonstrate that overall, our patients are very satisfied with trifocal mIOL implantation compared to their previous vision correction. The AT LISA tri 839MP lens offers a high level of spectacle independence and gives patients the option of intermediate vision as well as near and far (4) – something that has greatly improved their lives. In light of our findings, perhaps it’s time for ophthalmologists to pay more attention to intermediate vision, and to remember that it can be an important contributor to both visual function, and patient satisfaction.
Florian Kretz is a consultant ophthalmologist and research fellow at the IVCRC and the David J Apple International Laboratory for Ocular Pathology at the Department of Ophthalmology, University Hospital Heidelberg, Germany, research coordinator for the International Vision Correction Research Centre Network (IVCRC.net), Heidelberg, Germany and one of the lead surgeons at the Eyeclinic Ahaus-Raesfeld-Rheine (Gerl Group), Ahaus Germany.
Mariyana Dzambazova is an ophthalmology resident and a PhD student at the Medical University of Sofia, Bulgaria.
Matthias Gerl is a member of the IVCRC.net, Heidelberg, Germany and a lead surgeon of the Eyeclinic Ahaus-Raesfeld-Rheine, Ahaus, Germany.
Gerd Auffarth is director of the David J. Apple International Laboratory of Ocular Pathology, ICVRC and IVCRC.net, as well as chairman of the Department of Ophthalmology, Ruprecht-Karls-University of Heidelberg, Germany.
Supplementary Content: Patient Questionnaire
References
- M Lundstrom, K Pesudovs, “Catquest-9SF patient outcomes questionnaire: nine-item short-form Rasch-scaled revision of the Catquest questionnaire”, J Cataract Refract Surg, 35, 504–13 (2009). PMID: 19251145. PJ McDonnell, et al., “Responsiveness of the National Eye Institute Refractive Error Quality of Life instrument to surgical correction of refractive error”, Ophthalmology, 110, 2302–2309 (2003). PMID: 14644711. U Mester, et al., “Impact of personality characteristics on patient satisfaction after multifocal intraocular lens implantation: results from the ‘happy patient study’”, J Refract Surg, 30, 674–678 (2014). PMID: 25291750. FT Kretz, et al., “Level of binocular pseudoaccommodation in patients implanted with an apodised, diffractive and trifocal multifocal intraocular lens”, Klin Monbl Augenheilkd, [Epub ahead of print] (2015). PMID: 25927175.
