
When implanting toric IOLs, the surgeon must accurately identify the magnitude and axis of astigmatism and precisely position the lens on that axis intraoperatively. After all this effort – both before and during surgery – it is disheartening to see a lens rotate out of position postoperatively. Larger rotations of over 10° may require a secondary surgery to reposition the lens, contributing to a negative patient experience. In recent years, the majority of surgeons responding to ASCRS and ESCRS clinical surveys have indicated that they find over 5° of postoperative toric rotation to be unacceptable (1,2).
In my own practice, I have employed a variety of strategies to avoid malrotation, including the use of capsular tension rings, creating a posterior optic capture to improve lens stability, and even switching IOL platforms.
Developing design
In 2018, Bryan Lee and David Chang reported that TECNIS Toric lenses (Johnson & Johnson) were more likely than Acrysof toric IOLs (Alcon) to rotate between surgery and the first postoperative check (3). At the time, Johnson & Johnson was engaged in a process of developing and testing new toric designs, including one with frosted, squared haptics that eventually came to market as the TECNIS Toric II. This haptic design is now used in all of the TECNIS platform toric lenses, including the Eyhance, Symfony OptiBlue, and Synergy toric IOLs.
A proof-of-concept (POC) study conducted outside the US showed that the frosted haptics produced significantly lower rates of rotation compared with the predecessor ZCT series IOLs (see Table 1) (4). Post-approval, I was one of seven US surgeons who participated in a prospective study to confirm the results of the earlier POC study (5). In this study, which better reflected a real-world setting, we implanted the lenses in routine cataract surgery patients and we each used our own preferred surgical techniques and approaches to marking and intraoperative alignment;
In addition to recording subjective factors, such as satisfaction and visual acuity, we also objectively measured lens position and rotational stability using an image analysis method that has been previously described (6). For this robust measurement technique, the positions of 10 iris and scleral landmarks (Fig 1) were compared between photographs taken through the operative microscope at the conclusion of surgery and slit lamp photos taken at postoperative visits.
The findings
We found a very low level of rotation in 202 eyes of 125 patients implanted with TECNIS Toric II (ZCU series) IOLs in the study (5). The mean absolute rotation was less than 1°, with a tight standard deviation indicating that there were few outliers. In fact, 99.5 percent were within the tight tolerance of ≤5° of rotation that ophthalmologists are keen to see in a contemporary toric IOL. Our results mirror those from the POC study (see Table 1) and represent a considerably lower average rotation than was reported for either of the two lenses evaluated by Lee and Chang in their large series of more than 1,200 eyes (3). Though there is likely not a real clinical difference between an average rotation of 1° versus 3°, getting as close to zero as possible is desirable, especially when implanting higher toric powers.
Visual acuity was excellent in our study, with mean monocular uncorrected distance (UCDVA) of 0.03 ± 0.14 logMAR (about 20/21) and best-corrected distance visual acuity (BCDVA) of -0.06 ± 0.10 logMAR (about 20/17) for all study eyes. Nearly 97 percent of the eyes had BCDVA of 20/25 or better and 84.5 percent had UCDVA of 20/25 or better. Mean residual refractive cylinder was 0.30 D ± 0.35 D at the one week visit. The participating surgeons were satisfied or very satisfied with the rotational stability and overall clinical outcomes in 98 percent of cases. No IOLs needed to be repositioned.
In clinical practice, we rarely dilate an eye to measure how many degrees off-axis an IOL might be positioned. If the patient is happy and the visual acuity is good, we assume that the IOL is positioned in the correct axis – or quite close to it. However, with this study, we were able to show objectively that the positioning was accurate and that rotation was uniformly low and clinically insignificant. In short, the lenses stayed exactly where we put them!
In addition to these findings, we also evaluated whether various factors affected the likelihood of rotation. We found that there was no difference in rotation by race or ethnicity or by axial length (AL). This latter result was particularly interesting in light of a recent study that demonstrated that AL is not correlated with lens volume, so the expectation that high myopes with longer eyes are at higher risk of lens rotation may be inaccurate (7). Despite enrolling eyes with a wide variety of refractive error and anatomical measurements, we found no such correlation.
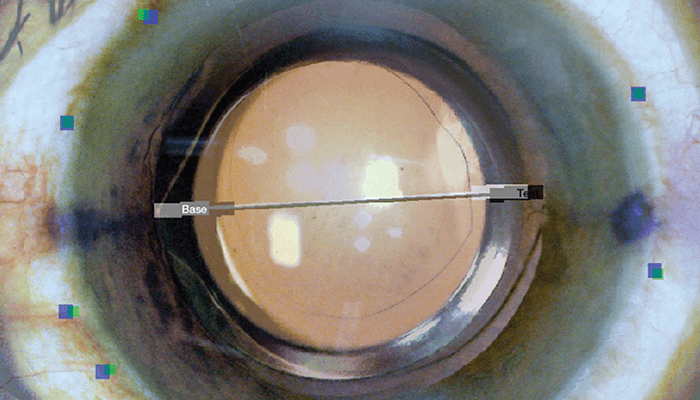
Table 1. IOL Rotation at 1 Week
Concluding thoughts
The TECNIS Toric II model in our study outperformed my expectations and significantly increased my comfort level in implanting toric IOLs. It is reassuring to know that, when a patient presents with corneal astigmatism, we have effective technologies to correct it – without introducing the potential headache of a malpositioned lens.
But let’s not forget the importance of practicing good surgery; excellent results with toric IOLs require precise power calculations using fourth-generation formulas, removal of all viscoelastic from behind the optic, and careful marking and alignment. That said, this particular toric lens has simplified troubleshooting in my practice. When a patient is unhappy or has unexpectedly poor vision postoperatively, we still have to diagnose the reason, but rotational concerns are now off the table for the TECNIS Toric II.
References
- T Kohnen et al., “ESCRS Clinical Trends Survey 2016-2021: 6-year assessment of practice patterns among society delegates,” Journal of Cataract & Refractive Surgery, 49, 133 (2023). PMID: 36700887.
- ASCRS Clinical Survey 2017. Accessed at https://www.facoelche.com/downloads/ascrs-clinical-survey-2017.pdf
- B S Lee, D F Chang, “Comparison of the Rotational Stability of Two Toric Intraocular Lenses in 1273 Consecutive Eyes,” Ophthalmology, 125, 1325 (2018). PMID: 29544960.
- J A Vukich et al., “Evaluation of Intraocular Lens Rotational Stability in a Multicenter Clinical Trial,” Clinical Ophthalmology, 15, 3001 (2021). PMID: 34285467.
- G A Quesada et al., “Reproducibility of the Magnitude of Lens Rotation Following Implantation of a Toric Intraocular Lens with Modified Haptics,” Clinical Ophthalmology, 16, 3213 (2022). PMID: 36199805.
- S Kasthurirangan et al., “Software-based evaluation of toric IOL orientation in a multicenter clinical study,” Journal of Refractive Surgery, 30, 820 (2014). PMID: 25437480.
- GO Waring IV et al., “Correlation of Intraoperative Optical Coherence Tomography of Crystalline Lens Diameter, Thickness, and Volume with Biometry and Age,” American Journal of Ophthalmology, 225, 147 (2021). PMID: 33385370.
