Herpes simplex virus (HSV) can be the most difficult corneal infectious disease to diagnose and manage despite its prevalence: at least 90 percent of the world’s population is infected with latent HSV-1 by the age of 60 (1). Herpetic keratitis (HK) is surprisingly common – in fact, it is the leading cause of corneal disease and blindness in humans worldwide (1). HSV keratitis is recurrent and, if not treated effectively and in a timely manner, can result in corneal nerve damage, which could lead to neurotrophic keratopathy with persistent epithelial defects. Untreated HSV keratitis can also contribute to the development of corneal scarring, corneal melting, potential corneal perforation, and permanent vision loss (2).
Clinical diagnosis
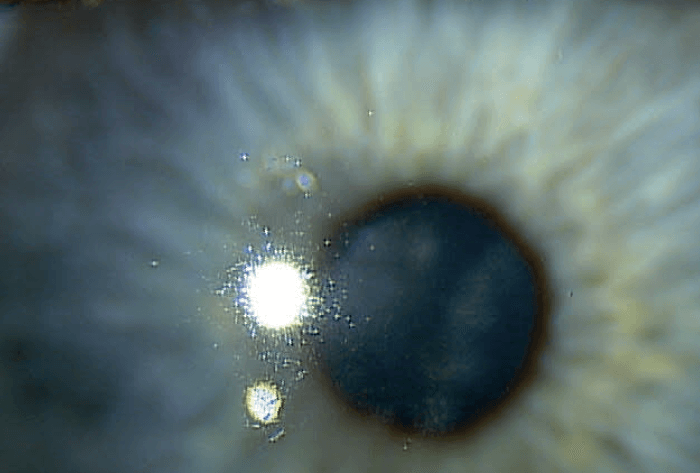
The HSV keratitis diagnosis is primarily based on characteristic features of the corneal lesion (3). We’re all familiar with the red flags, but a complete ocular history and a thorough slit lamp examination go a long way toward identifying and confirming a herpetic keratitis infection. Patients with epithelial herpetic keratitis may complain of pain, photophobia, blurred vision, tearing, and redness. The earliest sign of active disease is the development of small, raised, clear vesicular lesions on the cornea that will often stain with Rose Bengal. Dendritic ulcers are actually the most common presentation of herpetic keratitis. Prominent features of a dendritic ulcer include a linear branching pattern with terminal bulbs at the ends of the branches, swollen epithelial borders of the branches and central ulceration through the basement membrane. Fluorescein and Rose Bengal staining can aid in visualization of epithelial dendriform lesions with stippling of terminal endbulbs typical for HSV keratitis (4). Subbasal corneal nerves are also a telltale sign of HSV keratitis (5).
Recurrent disease
Though it’s true that most people have a herpes virus in their system at some point in their life, the number of those in whom it manifests and becomes symptomatic is much smaller. Those are the people we see coming in with recurrent herpetic keratitis of the eye. In a lot of these cases, when patients have their first ocular outbreak, they don’t know what’s happening. Often times they’ll present at optometry or general ophthalmology practices, but in cases where it becomes a recurrent issue for the patient, they often get referred to a cornea specialist. It’s a common enough occurrence that general ophthalmologists encounter it frequently; however, in a tertiary care referral cornea practice like mine, I always have a sizable percentage of patients who have herpetic keratitis.
There are patients who will have only one or two episodes of HSV keratitis throughout their life, but a large percentage of patients will have recurrent disease. During periods of stress, or if the eye undergoes surgical intervention, for instance, the virus might make a return appearance. Recurrent disease can cause scarring to settle in. Most cases resolve spontaneously within three weeks but, if not treated early, can go on to have irreversible subepithelial haze and scarring. In those that persist, the rationale for treatment is to minimize scarring and neovascularization, which are more common in recurrent disease.
Treatment options
Adequate prophylaxis and timely treatment are crucial to prevent corneal nerve damage, neurotrophic keratopathy, corneal scarring, corneal melting, corneal perforation, and vision loss (2). Gentle epithelial debridement may be performed to remove infectious virus and viral antigens that may induce stromal keratitis; antiviral therapy – topical or oral – can be effective treatments as well (6). The first effective drug used for HSV keratitis was idoxuridine (a pyrimidine analogue) way back in 1962 (7). Since then, the treatment options have primarily been a variety of nucleoside analogues and DNA-synthesis inhibitors (8).
The conventional drugs of choice for HK treatment tend to be acyclovir (ACV) and gancyclovir (GCV), which are nucleoside analogues and, less frequently, foscarnet (FOS) and cidofovir, which are DNA-synthesis inhibitors. These treatments, along with corticosteroids, have resulted in a significant reduction of HSV-induced corneal blindness (9).
The older, more traditional antiviral known as Viroptic (trifluridine) kills the active replication of the virus when it is on the surface of the eye, but it also wreaks havoc on the ocular surface, which can cause significant limbal stem cell deficiency. What’s more, preservatives in the drop can cause a significant epitheliopathy of the surface of the eye; in short, the cure is almost worse than the disease. Clinicians often start the patient on trifluridine and then continue it for too long, which is one of the reasons why we see a lot of the secondary side effects occur on the ocular surface.
Now we have better topical antivirals; for example, Zirgan (ganciclovir ophthalmic gel 0.15%, Bausch & Lomb), a gel used five times a day – but even that should be used for a limited time. It is effective at stopping viral replication on the surface of the cornea and is usually not needed any longer than two weeks. Beyond two weeks, it too can cause epitheliopathy, punctate keratitis, and ocular surface disease.
Conventional therapy includes treatment of the viral infection, which may be followed by topical steroids and other methods to heal the cornea. But there are limitations to this regimen; for instance, topical steroids may enhance viral replication and delay resolution in epithelial HK (10).
Infectious keratitis and CAM treatment pearls
- Many epithelial herpetic infectious keratitis patients are good candidates for CAM.
- Use CAM as soon as possible after identifying the infectious keratitis and initiating anti-microbial therapy, particularly when it is associated with significant inflammation.
- CAM can be used on an active viral infection because of its anti-microbial properties and because the infection can be monitored with fluorescein through the AM.
- CAM may warrant replacement if it turns from translucent to opaque or partially or completely dissolves in highly inflammatory cases.
- In patients with suspected protozoan or fungal keratitis, consider the use of CAM only after a diagnosis can be confirmed by culture, Gram stain, confocal microscopy, or after a response to topical therapy is observed.
Biological healing
Cryopreserved amniotic membrane (CAM) is an innovative solution that I’ve come to rely on with great success for many of my herpetic keratitis patients.
Several amniotic membrane options are available for ophthalmic purposes, including Prokera (BioTissue), AmbioDisk (Katena), and BioDOptix (Integra LifeSciences). AmbioDisk is a processed, dehydrated amniotic allograft intended for overlay use on the ocular surface. BioDOptix is also a dehydrated allograft, and its dehydration is facilitated via DryFlex, a proprietary process that preserves the amniotic tissue’s extracellular matrix, growth factors, and cytokines, all of which are instrumental in ocular tissue repair. Prokera is a cryopreserved amniotic tissue, and studies have shown that its preservation process, known as CryoTek, helps prevent, slow, or decrease scarring (11).
CAM has anti-inflammatory, anti-scarring, and anti-angiogenesis properties that are particularly important for this disease; they help improve epithelial healing; prevent perforation, scarring and irregular astigmatism; and regenerate corneal nerves (12, 13, 14). Data presented by Cooke and colleagues suggests that cryopreservation effectively preserves the structural and biochemical integrity of AM matrix components that are essential for the anti-inflammatory and anti-scarring effects that are observed clinically. Cooke’s study also showed that the absence of those components within dehydrated AM may contribute to the decreased effectiveness of the dehydrated tissue in reducing inflammation and fibrosis (15).
The CAM that I use for patients with HK is Prokera from BioTissue. Prokera is bound by a clear polymer ring and inserted into the eye in a manner similar to contact lens placement. CAM manages healing via the presence of collagen and growth factors. It also counteracts the potentially cytotoxic effects of topical antibiotics and provides antimicrobial effects over and above those of first-line antibiotics. Ultimately, CAM acts as both a bandage that protects the cornea and allows a microenvironment for healing. And, as a disease-modifying therapy that promotes regenerative wound-healing (12, 13, 14, 15), I find that post-herpetic scarring is reduced when I use CAM in these eyes.
How CAM works
CAM suppresses inflammation by facilitating neutrophil apoptosis, polarizing M1 to M2 macrophages and suppressing Th1 and Th17 lymphocyte activation. It inhibits scarring by preventing myofibroblast differentiation and reprogramming into progenitor cells, and promotes regenerative healing by supporting and augmenting stem cell function and maintaining stem cell quiescence (12).
The cryopreservation process allows CAM to retain heavy chain peptide (HC) covalently conjugated with high molecular weight hyaluronic acid (HA), which is noncovalently complexed with pentraxin-3 (PTX3). HC-HA/PTX3 is the biologic matrix that is responsible for CAM’s anti-inflammatory and regenerative healing properties. HA and PTX3 are involved in tissue repair and remodeling; and HC components of immunoglobulin form complexes with HA. Each component of CAM is found broadly in the human body but exist together as a complex in the amniotic membrane (12, 13, 14, 16, 17). This complex is what provides the regenerative healing that is maintained in cryopreservation, but lost in dehydration (15).
Therapeutic management
The two major visual sequelae of infectious keratitis, especially involving the visual axis, are scarring and ectasia; and both can be prevented, reduced or remediated with CAM (13, 17, 18, 19). It provides effective anti-inflammatory therapy with a better safety profile than topical steroids, which can delay healing, reactivate a viral infection, cause cataract formation, and elevate intraocular pressure (IOP) (20, 21).
A serious consequence of recurrent herpetic keratitis is the death of corneal nerves, resulting in neurotrophic keratitis. In fact, the most common cause of neurotrophic keratitis is herpetic eye disease. Neurotrophic keratitis is difficult to manage and often associated with non-healing and scar formation; CAM is especially effective for these cases. The cryopreserved membrane provides a milieu of anti-inflammatory substrates and regenerative cytokines to help heal the corneal surface when it is neurotrophic, and it has been shown in the literature and anecdotally to actually help regenerate nerves in the cornea (14).
Speedy resolution
CAM is a valuable adjunct in the acute phase of active herpetic disease, as well as in the neurotrophic phase. In the acute phase of an active viral replication, CAM along with oral antivirals will help speed up the time to resolution. It also helps heal the underlying scarring and haze that we typically see during the resolution of the virus.
In conclusion, I continue to use oral therapy or topical drops in many cases of herpetic keratitis in an effort to eliminate active disease and prevent disease recurrence. However, if the patient has had underlying dry eye or ocular surface disease, I veer away from topical therapeutics because they will further irritate the ocular surface. For those patients, CAM can be a first line treatment, and I do not necessarily need to add a topical antiviral to the oral regimen. Of course, each case needs to be assessed and treated based on the best clinical judgement for that patient.
Case 1
- Patient: 32-year-old woman
- History: Recurrent herpes simplex virus on her right cornea. Responds to topical Zirgan and oral ACV, but is having significant punctate keratitis and epitheliopathy from the topical toxicity of Zirgan. The cornea is also starting to develop visually significant subepithelial haze.
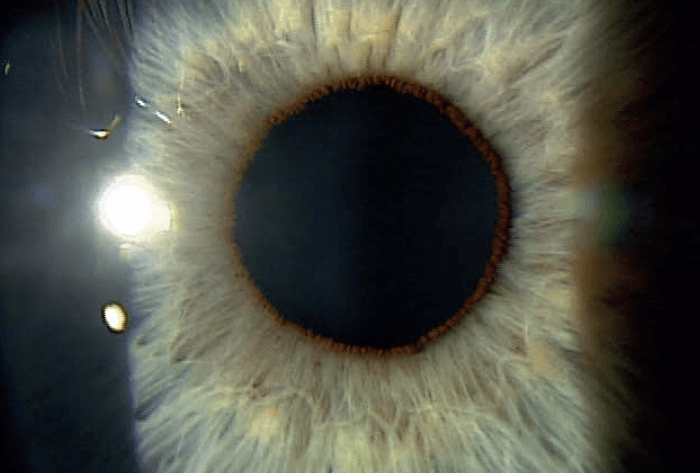
- Examination: Central corneal haze and severe 3-4+ punctate keratitis.
- Diagnosis: Resolved post herpetic disease with early scarring and epithelial toxicity
- Treatment: Prokera CAM slim placed on the right eye. Instructed to stop Zirgan and continue oral ACV. Prokera remained in place for 5 days.
- Follow-Up: Superficial punctate keratitis completely resolved after five days of Prokera. No active viral disease seen and significant reduction of the subeithelial haze/scarring. The patient’s best-uncorrected visual acuity improved while avoiding previously ineffective or irritating medications. The regenerative and anti-inflammatory effects of CAM produced desirable surface healing while avoiding topical steroid toxicity or risk of reactivating the herpetic disease.
References
- L Remeijer et al., “Human herpes simplex virus keratitis: the pathogenesis revisited,” Ocul Immunol Inflamm, 12, 255 (2004). PMID: 15621867.
- AJ Chucair-Elliott et al., “Degeneration and regeneration of corneal nerves in response to HSV-1 infection,” Invest Ophthalmol Vis Sci, 56, 1097 (2015). PMID: 25587055.
- K Wilhelmus, “Diagnosis and management of herpes simplex stromal keratitis,” Cornea, 6, 286 (1987). PMID: 3319411.
- M White et al., AAO (2014). “Herpes Simplex Virus Keratitis: A Treatment Guideline 2014”. Available at: https://bit.ly/33yvYeD.
- P Hamrah et al., “Corneal sensation and subbasal nerve alterations in patients with herpes simplex keratitis: an in vivo confocal microscopy study,” Ophthalmology, 117, 1930 (2010). PMID: 20810171.
- KF Tabbara, “Treatment of herpetic keratitis,” Ophthalmology, 112, 1640 (2005). PMID: 16139674.
- H Kaufman et al., “Use of 5-iodo-2’-deoxyuridine (IDU) in treatment of herpes simplex keratitis,” Arch Ophthalmol, 68, 235 (1962). PMID: 14454436.
- R Duan et al., “Acyclovir-resistant corneal HSV-1 isolates from patients with herpetic keratitis,” J Infect Dis, 198, 659 (2008). PMID: 18627246.
- Herpetic Eye Disease Study Group, “Oral acyclovir for herpes simplex virus eye disease: effect on prevention of epithelial keratitis and stromal keratitis,” Arch Ophthalmol, 118, 1030 (2000). PMID: 10922194.
- RM Shtein et al., “Herpes simplex keratitis after intravitreal triamcinolone acetonide,” Cornea, 26, 641 (2007). PMID: 17525670.
- K Jirsova, GLA Jones, “Amniotic membrane in ophthalmology: properties, preparation, storage and indications for grafting – a review,” Cell Tissue Bank, 18, 193 (2017). PMID: 28255771.
- SCG Tseng, “HC-HA/PTX3 Purified from amniotic membrane as novel regenerative matrix: insight into relationship between inflammation and regeneration,” Invest Ophthalmol Vis Sci, 57 (2016). PMID: 27116665.
- T Röck et al., “Amniotic membrane transplantation in 97. Reconstructive and regenerative ophthalmology,” Ann Transplant, 23, 160 (2018). PMID: 29507278.
- T John et al., “Corneal nerve regeneration after self-retained cryopreserved amniotic membrane in dry eye disease,” J Ophthalmol (2017). PMID: 28894606.
- M Cooke et al., “Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/chorion tissue,” J Wound Care, 23, 465 (2014). PMID: 25296347.
- CT Watson, F Breden, “The immunoglobulin heavy chain locus: genetic variation, missing data, and implications for human disease,” Genes Immun, 13, 363 (2012). PMID: 22551722.
- DR Lazzaro et al., “Idiopathic superior keratectasia with spontaneous perforation treated with amniotic membrane transplantation,” Eye Contact Lens, 34, 242 (2008). PMID: 18787434.
- A Al-Mujaini et al., “Bacterial keratitis: perspective on epidemiology, clinico- pathogenesis, diagnosis and treatment,” Sultan Qaboos Univ Med J, 9, 184 (2009). PMID: 21509299.
- A Lin et al, “Bacterial Keratitis Preferred Practice Pattern®,” Ophthalmology, 126, P1 (2019). PMID: 30366799.
- M Srinivasan et al., “Steroids for Corneal Ulcers Trial Group. The steroids for corneal ulcers trial (SCUT): secondary 12-month clinical outcomes of a randomized controlled trial,” Am J Ophthalmol, 157, 327 (2014). PMID: 24315294.
- H Sheha et al. “Amniotic Membrane Transplantation”, Expert Techniques in Ophthalmic Surgery, 1st edition, 167. JAYPEE: 2015.
