- Corneal crosslinking (CXL)is traditionally used to stabilize corneal ectasia and keratoconus progression
- Photoactivated chromophore for infectious keratitis-crosslinking (PACK-CXL) is currently being studied as a potential treatment modality for infectious keratitis
- Here, we overview current PACK-CXL research for bacterial keratitis, and consider the future potential for managing the disease.
Corneal crosslinking (CXL) initially came to prominence over three decades ago as a potential treatment modality to stabilize corneal ectasia and halt the progression of keratoconus. Its components – a photoactivated chromophore (riboflavin) and ultraviolet (UV) light – act on the corneal stroma, the collagen-rich central layer that comprises 90 percent of corneal thickness and contributes the bulk of corneal biomechanical stability. Effective stromal crosslinking strengthens corneal biomechanics by facilitating the formation of corneal fibrillar covalent bonds, which alters the biochemical structure of corneal collagen fibers and increases stromal resistance to enzymatic degradation or keratolysis. As researchers investigate ways to further improve the CXL procedure, newer potential applications of crosslinking are also under investigation. Transfusion medicine has harnessed the antimicrobial properties of crosslinking, and treats blood concentrates with crosslinking procedures to inactivate any existing microbial pathogens and decrease pathogen load. This advance has spurred the concept of using crosslinking in the management of infections, specifically corneal infections – namely, photoactivated chromophore for infectious keratitis-crosslinking (PACK-CXL) (a term that has been coined to differentiate from conventional CXL). Here, we will review what is currently known about PACK-CXL, and discuss the future therapeutic possibilities for the procedure.
Infectious keratitis
Infectious keratitis is a leading cause of blindness, ocular morbidity and permanent visual impairment worldwide, with prolonged contact lens wear in developed countries and poor access to ophthalmic healthcare services in developing countries representing major sources of complex infections. Onset and progression of the disease can be rapid, leading to clinical manifestations, such as corneal infiltration (stromal abscess formation, corneal edema, corneal ulceration, corneal melting) and anterior chamber inflammation. Current management strategies range from conservative measures with antibiotics to aggressive surgical management with corneal transplantation. Treatment can, however, be challenging because of the intensive medication regimen required to combat infection, as well as the associated risks of antibiotic resistance and the invasiveness of corneal transplantation with subsequent risks of rejection. As such, many research groups are looking to crosslinking as a potential adjunctive therapy to standard antibiotic treatment for the following reasons:- to shorten duration and modify clinical course of the disease, reducing risks of corneal melting and corneal scarring
- to improve visual outcomes
- to prevent the need for corneal transplantation
- to minimize antibiotic resistance
- to reduce financial burden of medications
- to minimize reinfection rates.
Reported techniques
PACK-CXL exerts its disinfectant, anti-microbial and bactericidal properties via the following biochemical mechanisms (2):- inhibition of pathogen replication by the chromophore’s chemical alteration of pathogen’s nucleic acids; the chromophore intercalates between the pathogen’s DNA and RNA bases, causing oxidation and inactivation.
- alteration of tertiary structure of collagen fibers, increasing resistance to collagenases and other degradative enzymes.
- reduction of inflammatory and immune cells, corneal nociceptive signaling, and inflammatory neovascularization.
- Induction – application of riboflavin solution (0.1% riboflavin-5-phosphate and 20% dextran T-500) to the corneal surface for 20–30 minutes at intervals of 2–3 minutes; hypotonic riboflavin was used in cases of thinner corneas (less than 400 µm). Some studies experimented with iso-osmolar riboflavin drops (4).
- Irradiance – 30 minute exposure of 365–370 nm wavelength of UV-A light source at an irradiance of 3 MW/cm2; riboflavin drops continued at 5 minute intervals.
- Post-treatment – soft contact lens with good oxygen transmissibility removed 5–7 days post-procedure; topical antibiotics for at least one week following treatment.
Reported outcomes
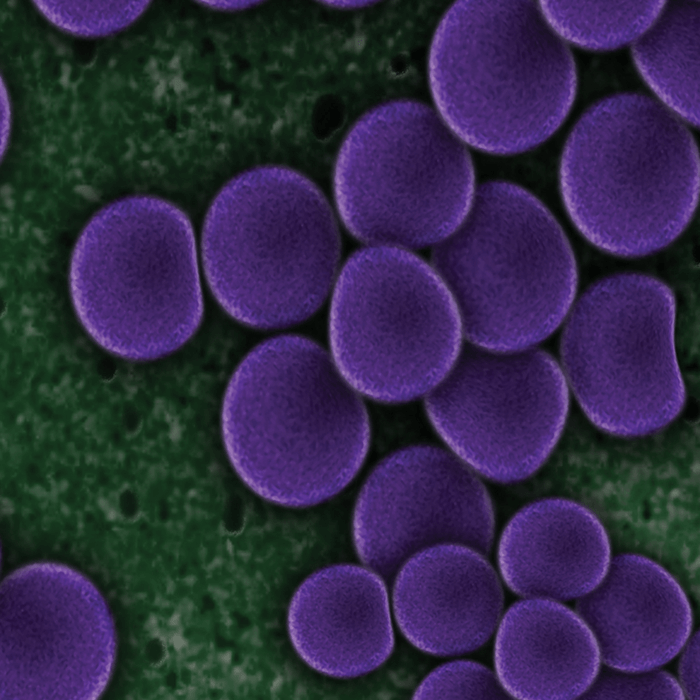
Published studies discuss the use of PACK-CXL in cases where the infection fails to respond to medical therapy, or to delay emergency keratoplasty which has a greater rejection rate than standard keratoplasties: both are listed as common inclusion criteria in the literature. The first case series was performed in 2008 by Iseli and colleagues in five patients unresponsive to medical treatment, and concluded that crosslinking was effective in arresting the progression of corneal melt and reducing size of infiltration in four of the patients (6). Most of the published literature on this topic consists of isolated case reports and case studies, with only a handful of prospective (only one which is randomized), and retrospective clinical studies. In a meta-analysis of 210 eyes of 209 patients with infectious keratitis, 96 eyes had keratitis of bacterial etiology. The proportion of eyes that healed with CXL was 85.7 percent (95 percent confidence interval, 78.5–91.7) (3). Makdoumi and colleagues reported one of the few studies that used CXL as a first-line therapy for bacterial keratitis with initial presentation of corneal ulcer: initially, all patients responded to CXL, with 12.5 percent needing adjunctive treatment with systemic and topical antibiotics (7). In a prospective study of 40 eyes – 21 undergoing PACK-CXL and 19 undergoing conventional antimicrobial therapy – the complication rate in the control group was found to be 21 percent, whereas there were no complications (corneal perforation or recurrent infection) in the PACK-CXL group (8). However, no significant difference in corneal healing time (epithelization) and final visual outcomes were noted between the two groups. Numerous other cases have reported the use of crosslinking to reduce the risk of perforation by strengthening the cornea, promoting epithelization and corneal healing, and reducing pain/inflammation as well as shortening the course of treatment (9–11). In a meta-analysis of 12 articles and 104 eyes, faster epithelization was reported in gram-positive bacterial keratitis versus gram-negative bacterial keratitis (1). Furthermore, lower transplantation rates were reported in bacterial keratitis versus fungal or amoebic keratitis (1). Fungal and amoebic infections penetrate deeper into the cornea, and it is known that the risk of endothelial cell loss related the procedure is increased if the infection penetrates to more than 250 µm depth. As such, the depth of infiltration has been noted as an important exclusion criterion in literature. In cases of deep infiltration, some have proposed the use of a longer duration of irradiance coupled with hypo-osmolar riboflavin. Few complications have been reported post-procedure. Those reported include initial worsening of hypopyon (<40 percent), corneal edema (<5 percent), and dendritic lesions (<5 percent). Shetty and colleagues described a case series of nine patients with bacterial keratitis, who were treated with antibiotics two weeks prior to CXL (12). Although 6 out of the 9 cases resolved, cases with deep stromal keratitis or endothelial plaque did not respond to the treatment leading the authors to conclude that CXL was effective in microbial keratitis with superficial stromal involvement.Common organisms that cause bacterial keratitis include Staphylococcus Aureus, Pseudomonas aeruginosa, Staphylococcus epidermidis, Streptococcus Pneumoniae and Escherichia coli. Patients are typically started on broad-spectrum quinolones (for example, ofloxacin) until confirmatory cultures to select a specific antibiotic regimen are obtained.
Challenges and controversies
Despite a wealth of published studies, it is difficult to delineate clear clinical outcomes due to (13):- variability in reported visual outcomes
- variability in grades of infiltrate, size of epithelial defects, and severity of infections
- non-homogeneity of infectious organisms; variability in etiology of infections
- absence of control groups
- lack of defined, uniform inclusion/exclusion criteria and safety/efficacy endpoints
- lack of standardization in the use of PACK-CXL; limited single first-line therapy studies with majority of studies reporting varying antibacterial drugs prior to, during, and after CXL treatment.
PACK-CXL – a new application?
Crosslinking seems to have a beneficial effect for treatment of bacterial keratitis and possibly for fungal keratitis, especially if the infective lesions are shallow (less than 50 percent depth in the cornea). It would seem to be contraindicated in viral or amoebic disease, and less likely to be effective in deep ulcers. Crosslinking would be a welcome addition to the present armamentarium for keratitis, especially in cases of microbial keratitis, which touts the highest numbers of drug-resistant organisms, and advanced or progressed keratitis either as a temporizing measure or a long-term option for high-risk surgical patients. Studies are diverse and lack standardization, making it difficult to derive clinical utility at the present time. The general consensus, however, advocates crosslinking as a potential therapeutic agent to promote epithelialization and arrest corneal melting in infectious keratitis. In short, PACK-CXL is a new application that the ophthalmic community should continue to pursue. Sneha Konda is a fourth year medical student at Texas A&M College of Medicine, College Station, TX, USA. Bala Ambati is Professor of Ophthalmology, Moran Eye Center, University of Utah, UT, USA.References
- JL Alio et al., “Corneal cross linking and infectious keratitis: a systematic review with a meta-analysis of reported cases”, J Ophthalmic Inflamm Infect, 3, 47 (2013). PMID: 23718849. A Panda et al., “Photo-activated riboflavin therapy of refractory corneal ulcers”, Cornea, 31, 1210–1213 (2012). PMID: 27710492. L Papaioannou et al., “Corneal collagen cross-linking for infectious keratitis: a systematic review and meta-analysis”, Cornea, 35, 62–71 (2016). PMID: 26509768. K Makdoumi et al., “Infectious keratitis treated with corneal crosslinking”, Cornea, 29, 1353-1358 (2010). PMID: 21102196. B Knyazer et al., “Accelerated corneal cross-linking with photoactivated chromophore for moderate therapy-resistant infectious keratitis”, Cornea, 528–531 (2018). PMID: 29300262. HP Iseli et al., “Ultraviolet A/riboflavin corneal cross-linking for infectious keratitis associated with corneal melts”, Cornea, 27, 590–594 (2008). PMID: 18520510. K Makdoumi et al., “UVA-riboflavin photochemical therapy of bacterial keratitis: a pilot study”, Graefes Arch Clin Exp Ophthalmol, 250, 95–102 (2012). PMID: 21874347. DG Said et al., “Collagen cross-linking with photoactivated riboflavin (PACK-CXL) for the treatment of advanced infectious keratitis with corneal melting”, Ophthalmology, 121, 1377–1382 (2-15). PMID: 24576886. A Bozkurt et al., “Corneal collagen crosslinking treatment in a case with pneumococcal keratitis”, Turk J Ophthalmol, 47, 161-164 (2017). PMID: 28630792. S Bamdad et al., “Ultraviolet A/riboflavin collagen cross-linking for treatment of moderate bacterial corneal ulcers”, Cornea, 34, 402–406 (2015). PMID: 25710507. C Bonzano et al., “Collagen cross-linking in the management of microbial keratitis”, Ocul Immunol Inflamm, 1–6 (2018). PMID: 29308960. R Shetty et al., “Collagen crosslinking in the management of advanced non-resolving microbial keratitis”, Br J Ophthalmol, 98, 1033–1035 (2014). PMID: 24711659. P Garg et al., “Collagen cross-linking for microbial keratitis”, Middle East Afr J Ophthalmol, 24, 18–23 (2-17). PMID: 28546688. CB Evangelista and KM Hatch. “Corneal collagen cross-linking complications”, Semin Ophthalmol, 33, 29–35 (2018). PMID: 28876968. M Rana et al., “Severe microbial keratitis and associated perforation after corneal crosslinking for keratoconus”, Cont Lens Anterior Eye, 38, 134–137 (2-15). PMID: 25435381.
