Diabetes is a familiar disease to ophthalmologists – they make the first diagnosis in almost half of all cases. And on top of being the leading cause of new blindness in people aged 20 to 74 years in the USA, it’s a risk factor for a whole host of other problems, including cardiovascular disease, renal failure, neoplasms and neuropathies. And when it comes to diagnosing diabetic neurodegeneration, ophthalmic examination could once again come in useful: recent research indicates that an OCT examination could predict early signs of neuropathy.
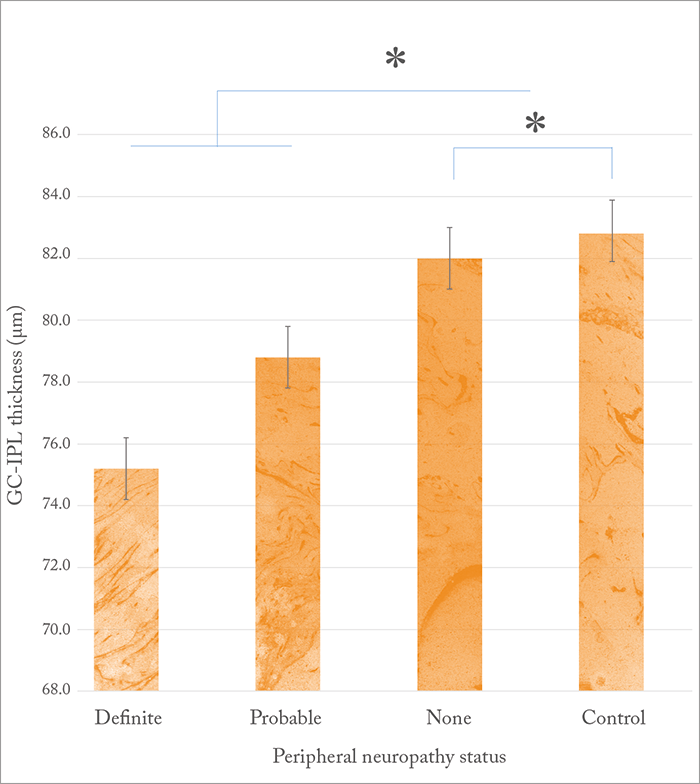
With that in mind, South Korean researchers used OCT to study the connection between retinal thickness, peripheral nerve conduction, and autonomic nerve function in diabetic patients, as retinal neurodegeneration and diabetic peripheral neuropathy are suspected to be initiated by similar hyperglycemia-activated pathways. The group studied consisted of 160 people aged 55 to 75 years, who had a diagnosis of type II diabetes but who did not have diabetic retinopathy or mild proliferative diabetic retinopathy, and 60 age-matched controls. Exclusion criteria included over 10 years’ duration of diabetes and a diagnosis of any peripheral neurologic disease except diabetes-related neuropathy. Parafoveal retinal thickness and ganglion cell-inner plexiform layer (GC-IPL) thickness were measured, and peripheral nerve involvement was assessed. When the study participants were divided into three groups (no neuropathy, probable neuropathy and definite neuropathy), the authors found that parafoveal retinal thickness did not appear to be related to neuropathy. But GC-IPL thickness was significantly lower in the group with neuropathy (75.2 ± 4.2 µm, p=0.002) compared with the probable (78.8 ± 5.0 µm) and no neuropathy (82.0 ± 5.8 µm) groups (Figure 1) – and both peripheral nerve conduction and autonomic nerve function were found to correlate to GC-IPL thickness using regression modeling. Diagnosis of diabetic neuropathy can be a challenge, as symptoms can be widely varied – but further study of the link between neurodegeneration of the retina and nerve degeneration could yield more insights. The authors note, “This study should prompt ophthalmic evaluation in patients with clinical or subclinical peripheral neuropathy or autonomic dysfunction. Also, a thinner retinal nerve fiber layer noted by the ophthalmologist should prompt more detailed questioning of peripheral nerve symptoms.”
References
- K Kim et al., “Retinal neurodegeneration associated with peripheral nerve conduction and autonomic nerve function in diabetic patients”, Am J Ophthalmol, 170, 15–24 (2016). PMID: 27381712.
