Most of my patients are presbyopes in their late 40s and older; they require either a clear lens exchange or cataract surgery. The remainder – about 20 percent – are candidates for LASIK and implantable contact lenses.
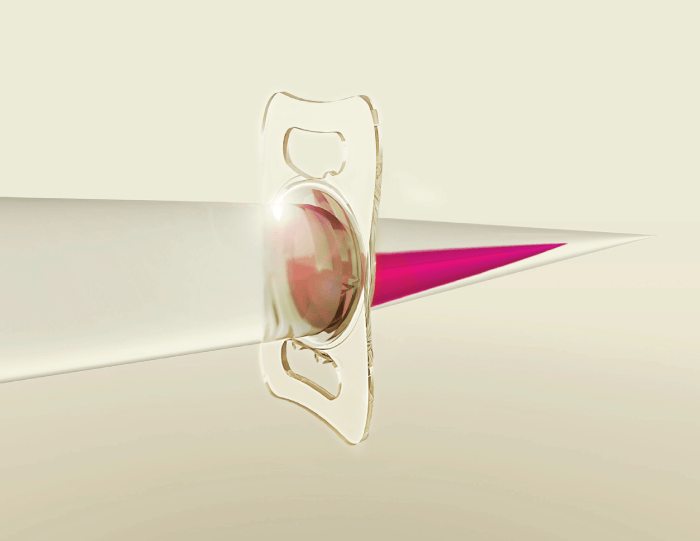
I’ve been using Teleon Surgical’s Lentis MPlus Toric IOLs for 10 years, and Lentis Comfort Toric for around six years. In this time, I have found that I prefer the Lentis multifocal implants over competitor lenses. In brief, they give me fewer problems with inadequate reading power, glare, and halos.
In my experience, patients up to their late 60s do better with multifocal IOLs. In older patients, outcomes may be compromised by poor ocular surface or poor eye health in general. Another factor is attitude: generally, patients are expected to accept that they may have a tougher first year while acclimating to the majority of multifocal lenses, and they will need to be patient with some glare and halos over the first few months – with Teleon lenses, photic phenomena are not so much of an issue. Also, patients must be willing to commit time and effort to eyelid hygiene: lubricant application and removal of Meibomian gland secretions. They must also accept the small but finite chance that the multifocal IOL may require fine adjustment after implantation; this involves LASIK or YAG laser capsulotomy surgery, which may be inconvenient and, of course, is not free.
Key advantages of Lentis IOLs
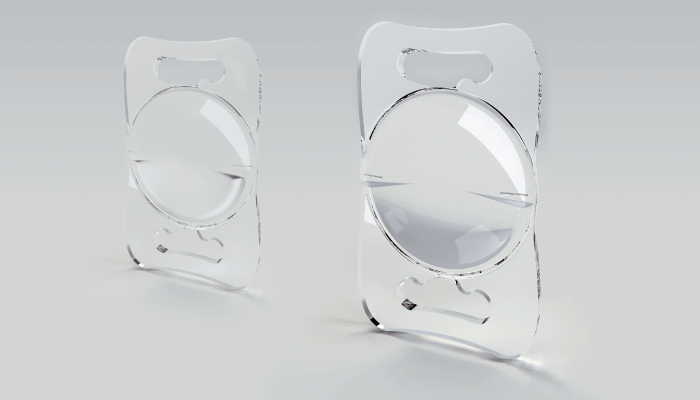
The unique advantage of Teleon’s Lentis lenses is that they can be customized, enabling us to eliminate astigmatism to the fullest extent possible in each patient. By contrast, competitor lenses – which cannot be customized – always have some residual astigmatism.
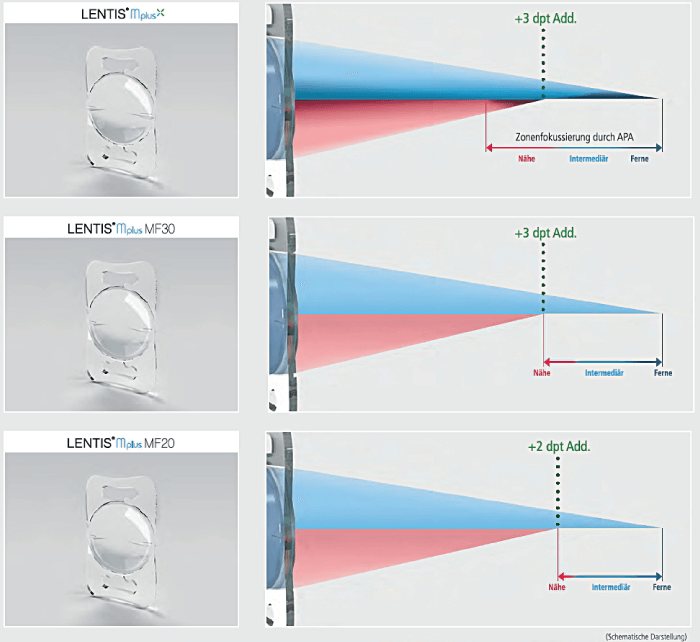
Furthermore, by using different Lentis IOLs in combination – the Comfort in one eye and the MPlus in the other – patients achieve optimal outcomes over all three zones of vision. Why? Because the Comfort excels in intermediate and distance vision, while MPlus provides good near vision; the combination has obvious advantages. I know that other trifocal lenses claim to provide good outcomes over all three zones of vision, but, by combining two customized Teleon lenses, nearly all of our patients achieve spectacle freedom for all three zones of vision.
Additionally, while dysphotopsia remains a real problem for many widely available multifocal lenses, it is much less of a concern in Teleon lenses. Certainly, in my experience, glare photopsias are more severe in competitors than in Lentis lenses.
These clear advantages differentiate Teleon lenses from other multifocals, which do not provide the powerful reading vision that we can achieve with the MF30T – especially in younger, highly myopic (more than -5dpt) patients. With the Comfort lens we can confidently achieve good intermediate vision as well.
Customized lenses – customized patient outcomes
I have heard surgeons proudly report multifocal outcomes of 6/9 unaided postoperative vision, but I would be horrified with that result!
After a Comfort/MPlus combination, 95 percent of my patients get 6/6 vision in both eyes for distance – Lentis lenses are that reliable. In the Comfort eye, they are N8 to N10 for reading, and in the MPlus eye they are typically N4 or 5. This lens combination also enables patients to work with computer screens – a distance of about 65-70 cm – which is important for many people. More specifically, I usually achieve emmetropia with the MPlus by following the recommended emmetropia index provided with every biometry read-out. With the MF15, I use the Haigis formula and aim for plano.
Additionally, Lentis lenses perform excellently in post-LASIK eyes – I haven’t come across a better multifocal IOL for this patient group. Perhaps this is a consequence of its design; it’s a segmental reading lens, not a concentric ring IOL, which may better suit the post-aberration cornea.
In summary, 95 percent of my multifocal IOL patients never need glasses at all. The remainder may occasionally use reading glasses; for example, when reading challenging fine print. But that really depends on the individual and what they do. I am highly satisfied with Lentis lenses – and, even more importantly, so are my patients!
For surgeons starting to use the Teleon Surgical lenses
If you’d like to start using these IOLs, get advice from surgeons who are experienced with them; ask them what kind of patients you should start with. Understand how these surgeons target their approach with biometry, and what they target for each and every lens. Select your first few patients according to that advice and understanding, and don’t neglect preoperative counselling: it is important to manage patient expectations regarding the postoperative experience, including any side effects that they might encounter.
Assessing patients for suitability
I always do a Schirmer’s test and assess the ocular surface with fluorescein and a slit lamp – severe dry eye or very severe Meibomian gland dysfunction are contraindications for multifocal IOL. I’ve seen a handful of young patients who – despite perfect IOL implantations – ended up with only 6/12 postoperative vision due to Meibomian gland dysfunction producing a sebaceous layer over the cornea. Even after treating their ocular surface disease, they only reach 6/9 or 6/7.5.
I also examine the corneal surface with a Pentacam; assessment of corneal thickness and curvature is essential to establish if it can support LASIK or other adjustments, if required post-operatively; this is also known as Bioptics. This is important, because about 5 percent of patients require minor post-surgical refractive adjustment to optimize visual outcomes, and it helps to know what the options are in such cases.
Generally, I prefer not to use multifocal IOLs in cases of macular dysfunction, retinal disease, epiretinal membranes, or glaucoma.