One of the many challenges associated with Alzheimer’s disease (AD) is timely identification and diagnosis – the earlier the disease can be caught, the higher the potential to prevent, or slow down, its progression with interventions like brain training or nootropic drugs. Retinal exams might be the answer, and already multiple research groups are investigating their diagnostic potential: a team from the University of Minnesota are evaluating retinal non-invasive hyperspectral endoscopy to look for signs of amyloidopathy in a mouse model of AD (1), and another group at the University of Waterloo in Ontario have shown that ß-amyloid deposits in neural retina can be detected non-invasively using their polarized light microscopes (2). But this isn’t the whole story: results from a large cohort study (3) have shown that retinal nerve fiber layer (RNFL) thinning is significantly associated with poor cognitive function, which immediately suggests that regular retinal thickness measurements could represent an important method of catching early signs of the disease.
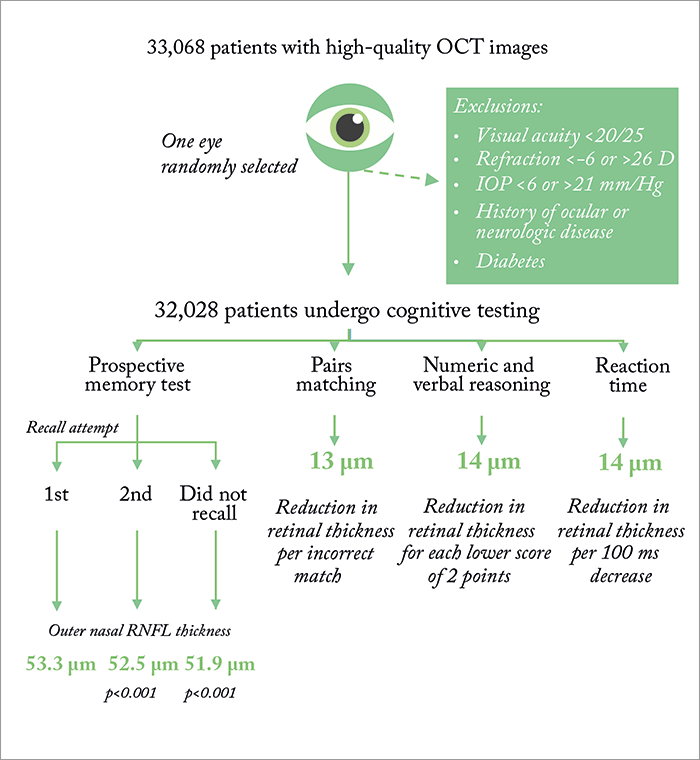
An international team of researchers are behind these findings. Using data from the UK Biobank study (a major ongoing health resource project which features over 500,000 volunteers) they identified over 30,000 participants with spectral domain (SD) OCT scans, and performed multivariable regression modeling to compare RNFL thickness data with results from cognitive measures (including tests for prospective memory, numerical and verbal reasoning, and reaction time). What they found was the RNFL was significantly thinner in participants who had “abnormal” cognitive test results (see Figure 1) – and thinner RNFLs were linked with poorer outcomes in prospective memory, pairs matching, numeric and verbal reasoning, and reaction time tests (p<0.001). They also found that, for each cognitive test failed, RNFL was significantly thinner by 1 µm. The researchers analyzed all macular subfields, and found that outer nasal RNFL thickness “appeared [to be] the most sensitive to changes to cognitive function” (1). So could we one day see ophthalmologists and optometrists play a leading role in identifying this debilitating disease in its early stages? We will be following this development very closely.
References
- R McGuigan, “Alzheimer’s Disease Peep Show”, The Ophthalmologist, 32, 10 (2016). Available at: top.txp.to/issues/0716/203. M Campbell et al., “Amyloid as a biomarker of Alzheimer’s disease in post-mortem retinas in human and the dog model of Alzheimer’s disease”, Presented at the Alzheimer’s Association International Conference; 2016, Toronto, Canada. Abstract: a10000. F Ko et al., “Retinal nerve fiber layer thinning associated with poor cognitive function among a large cohort, UK Biobank”, Presented at Alzheimer’s Association International Conference; 2016, Toronto, Canada. Abstract: a10202.
