Most patients with retinal degeneration lose sight because of a gradual loss of photoreceptors, with the rest of the retina remaining largely functional. This fact is what enables retinal prostheses to work – they provide electrical stimulation of the surviving neurons and enable information to enter the visual system once more. There are two ways of stimulating the surviving neurons with retinal prostheses: epiretinally, targeting the retinal ganglion cells (the approach taken with Second Sight’s Argus II), or subretinally, targeting the inner retinal neurons (as per Retina Implant’s Alpha IMS). However, irrespective of the approach, the fact remains that the implantation of these prostheses and their transscleral cables is a long and challenging surgical procedure, and even after a successful procedure, visual acuity remains below 20/1,000 in most cases (1,2).
Now, a group of researchers have devised an alternative retinal prosthetic that they hope will overcome some of the alternatives’ shortcomings (3). The implant consists of 70 µm wide photovoltaic pixels (Figure 1). Those pixels receive bright pulsed light from image-projecting video goggles and convert it into electrical signals that stimulate the retinal neurons – entirely without wires. This translates to a far simpler surgical procedure, as each hexagonal pixel array is only 1–2 µm wide and can be placed through a small retinotomy, allowing the ophthalmologist to tile a large visual field with minimal impact on the patient. Upon testing their photovoltaic implants in rats, the researchers found that they elicited retinal responses with a spatial resolution of 64 ± 11 µm – slightly under half the visual acuity of healthy rats (27 ± 9 µm).
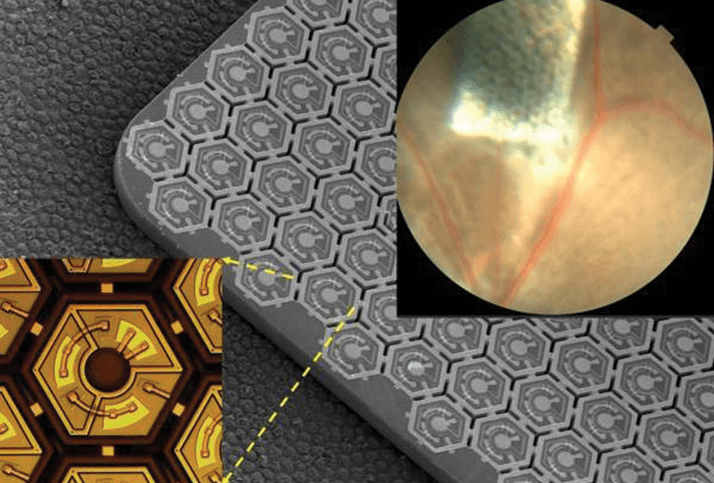
The current generation of retinal prostheses have a cortical activation threshold of 0.55 mW/mm², about four times lower than that of the previous generation. Lower stimulation thresholds allow the development of better video goggles to be used with the prosthesis, and also permit a reduction in pixel size (in this case, by approximately a factor of two), meaning that – as pixel size is the resolution-limiting factor in this type of implant – spatial resolution can be correspondingly increased. Following the success observed in animal models, the implant is set to enter clinical trials in France in 2016. “The performance we’re observing at the moment is very encouraging,” says the study’s corresponding author, Georges Goetz. “Based on our current results, we hope that human recipients of this implant will be able to recognize objects and move about.” The project’s joint supervisor, Daniel Palanker, adds, “Eventually, we hope this technology will restore vision of 20/120, and if it works that well, it will become relevant to patients with age-related macular degeneration.”
References
- MS Humayun, et al., “Interim results from the international trial of Second Sight’s visual prosthesis”, Ophthalmology, 119,779–788 (2012). PMID: 22244176. K Stingl, et al., “Artificial vision with wirelessly powered subretinal electronic implant alpha-IMS”, Proc Biol Sci, 280, 20130077 (2013). PMID: 23427175. H Lorach, et al., “Photovoltaic restoration of sight with high visual acuity”, Nat Med, 21, 476–482 (2015). PMID: 25915832.
