Creation of the anterior capsulorhexis is a key stage in cataract surgery, and producing a precise rhexis is of paramount importance. The most commonly used technique to achieve this during phacoemulsification is continuous curvilinear capsulorhexis (CCC). CCC was first popularized by Gimbel, Neuhann and others (1-3) to make lens removal and IOL implantation in the capsular bag safer; it avoided the radial tears which occurred frequently in the can-opener capsulotomies that were performed at the time. We have come a long way in the intervening 25 years!
The technique requires a skilled surgeon to pay careful attention during the procedure. Historically, it was termed “continuous curvilinear capsulorhexis,” because the opening created did not have to be exactly circular to have all of the desired qualities at the time – a time before the advent of premium and aspheric IOLs. When viscoelastic use became routine in cataract surgery, the technique evolved into a full-circle tear, facilitated by capsular forceps designed by Peter Utrata (see figure 1). Today, obtaining a precise circular capsulorhexis pays big dividends, enabling the surgeon to achieve even the most demanding of refractive results. A correctly sized, and a well-centered capsulorhexis with a 360° overlapping capsular edge prevents IOL tilt, myopic shift, optic decentration, and posterior and anterior capsular opacification, partly due to a combination of the symmetric contractile forces of the capsular bag, and the shrinkwrap effect (4–10). However, “eccentric or irregularly shaped capsulorhexis with a diameter extending beyond the optic edge may lose these advantages” (11). Here’s how I perform CCCs today.
Today’s CCC
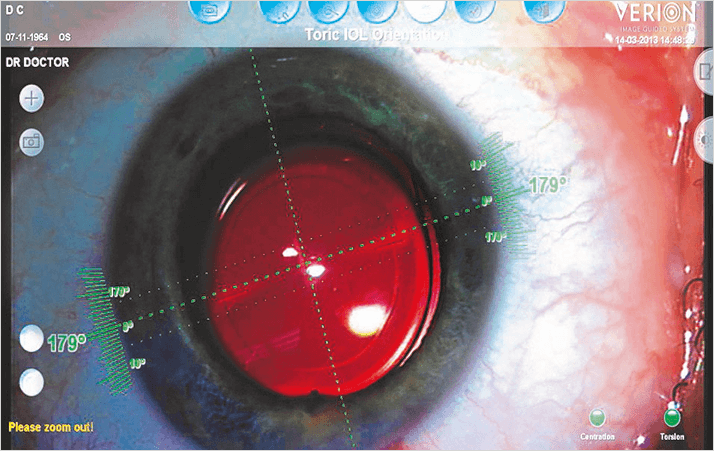
Before commencing the rhexis, the surgeon must place enough viscoelastic material (such as Viscoat) in the anterior chamber to counter the pressure of the vitreous. This flattens the anterior lenticular capsule, preventing a forward push of the lens by vitreous pressure, which can result in a radial tear. The manual CCC can be centered with the help of Purkinje images. A number of instruments can assist in this critical step, such as the VERION image guided system (See Figure 2) and the CALLISTO eye (Carl Zeiss Meditech, Jena, Germany), which enable an image of the ideal capsulorhexis to be displayed in one ocular of the microscope. If the surgeon matches this ideal circle with the anterior capsulorhexis, a CCC is formed around the visual axis.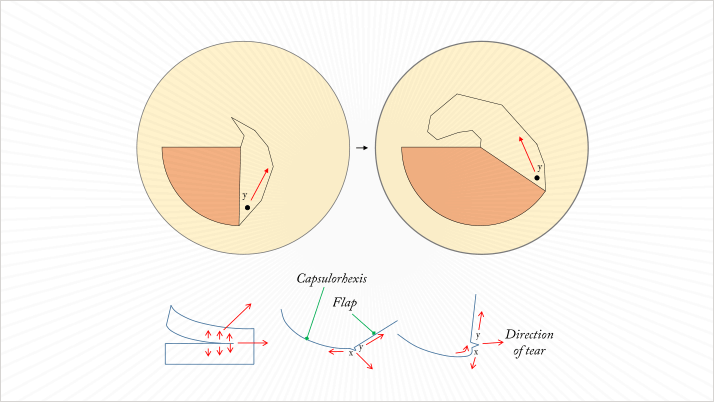
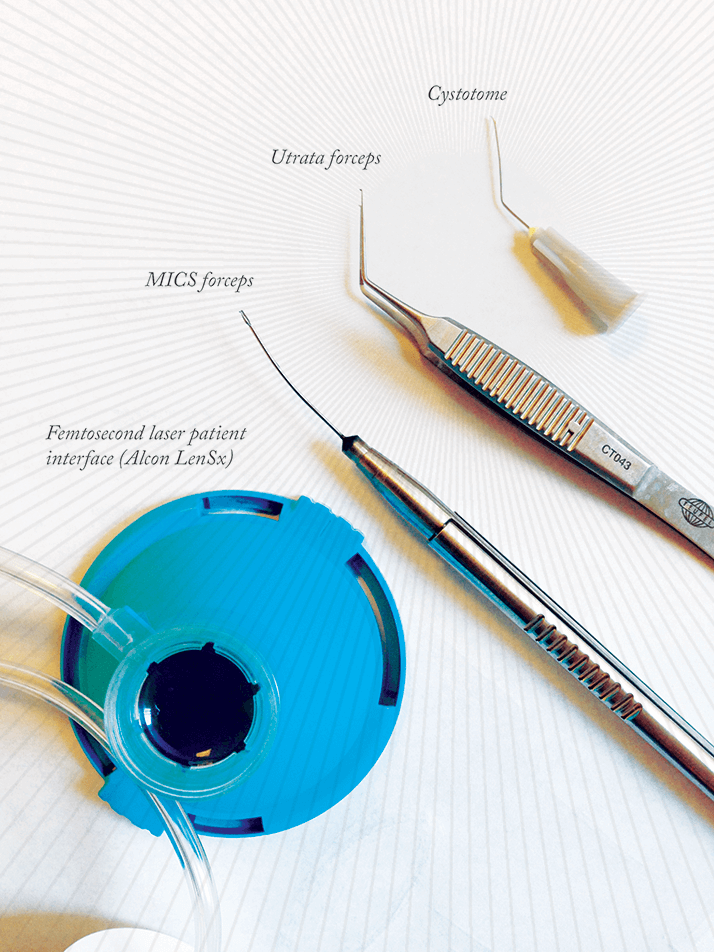
Many different instruments can be used to perform the CCC, with selection depending on the length of the incision that the surgeon chooses to make. For example, cystotome needles or Utrata forceps can be used to perform the CCC and 23-gauge vitrectomy-style forceps used for microincisional cataract surgery (MICS; Figure 1).
The size of the rhexis really does matter; ideally, there should be a small overlap with the intraocular lens optic. Tricks to assist in sizing the rhexis include:
- Making a corneal impression by pushing a ring caliper on the cornea – much like the centering of the radial keratotomy incisions around the visual axis in the old days. The marker does not need to be inked; the faint corneal impression is usually enough.
- Introducing the ring caliper (of the rhexis size you wish to achieve) into the anterior chamber and placing it around the visual axis. The cohesive viscoelastic gives enough pressure to push the caliper gently against the anterior capsule.
In manual CCCs, it is essential that capsule tear direction is controlled (Figure 3), as the overall direction of pulling forces on the capsule flap can cause different tearing direction patterns. There are no shortcuts here; this is a skill that has to be mastered to achieve the perfect CCC. When a tear does begin in a peripheral or radial direction, immediate action is needed. Usually, a viscoelastic cushion is placed in the zone towards the tear extension. The surgeon must grasp the capsule close to the tear and then pull to the exact center of the eye to recover the capsulorhexis – this works even if the tear propagated under the iris. Having said this, there are now alternative methods to performing a manual CCC: mechanical devices, such as the Fugo Plasma Blade (MediSURG, Norristown, PA, USA) and of course, femtosecond lasers. Helpfully, femtosecond lasers can rapidly and reproducibly create perfectly circular rhexis patterns – and in difficult cases, I find such instruments to be invaluable. The rhexis is performed without opening the anterior segment, and the sizing and the position of the rhexis can be controlled almost to perfection.
Johann Blanckaert is the Director of the Eye & Refractive Center in Iper, Belgium and a Consultant Ophthalmologist at UZ Leuven. He is the current President of BBO-UPBMO, the Belgian Professional Union of Medical Specialists in Ophthalmology and Ocular Surgery.
References
- T. Neuhann. “Theory and surgical technic of capsulorhexis”, Klin Monatsbl Augenheilkd., 190, 542–545 (1987). H.V. Gimbel, T. Neuhann. “Development, advantages, and methods of the continuous circular capsulorhexis technique”, J Cataract Refract Surg., 16, 31–37 (1987). H.V. Gimbel, T .Neuhann. “Continuous curvilinear capsulorhexis”, J Cataract Refract Surg., 17, 110–111 (1991). G. Ravalico et al., “Capsulorhexis size and posterior capsule opacification”, J Cataract Refract Surg., 22, 98–103. (1996). U. Aykan, A.H. Bilge, K. Karadayi. “The effect of capsulorhexis size on development of posterior capsule opacification: small (4.5 to 5.0 mm) versus large (6.0 to 7.0 mm)”, Eur J Ophthalmol., 13, 541–545 (2003). E.J. Hollick, D.J. Spalton, W.R. Meacock. “The effect of capsulorhexis size on posterior capsular opacification: one–year results of a randomized prospective trial”, Am J Ophthalmol., 128, 271–279 (1999). J. Ram et al., “Effect of in–the–bag intraocular lens fixation on the prevention of posterior capsule opacification”, J Cataract Refract Surg., 27, 367–370 (2001). D.F. Chang, et al., “Pearls for sizing the capsulorhexis”, Cataract & Refractive Surgery Today Europe., 3, 40–44 (2008). K. Hayashi et al., “Anterior capsule contraction and intraocular lens decentration and tilt after hydrogel lens implantation”, Br J Ophthalmol., 85, 1294–1297 (2001). K. Hayashi et al., “Anterior capsule contraction and intraocular lens dislocation in eyes with pseudo– exfoliation syndrome”, Br J Ophthalmol., 82, 1429–1432 (1998). K. Kránitz et al., “Femtosecond laser capsulotomy and manual continuous curvilinear capsulorhexis parameters and their effects on intraocular lens centration”, J Refract Surg., 27, 558–63 (2011). B.S. Seibel, “Phacodynamics: Mastering the Tools and Techniques of Phacoemulsification Surgery (Third Edition)” ISBN 1-55642-388-8, (1998).
