The unlimited potential for innovation remains one of ophthalmology’s most attractive features for applicants and practitioners alike. Technology has evolved tremendously since the days of couching and continues on its upward trajectory as new inventors and entrepreneurs realize their ideas.
Here, we review some of the highlights in ophthalmology over the past 100 years, discuss ways to bring new concepts to market, and cover some emerging technologies. This list is by no means comprehensive, but offers a glimpse into the problem-solving process that made ophthalmology as safe and consistent as it is today.
1949 – First implanted intraocular lenses (IOLs)
The first posterior chamber IOL was placed by Harold Ridley, who appreciated that the acrylic (PMMA) material of an aircraft windshield incited little inflammation in the eye. A 42-year-old woman was the first patient implanted with a PMMA lens; this initial attempt left the eye with a postoperative spherical equivalent error of -21.00 D (1). The first anterior chamber IOL was placed in France in 1952.
1961 – Fluorescein angiography (FA)
Harold R. Novotny and David L. Alvis were the first to describe the technique for retinal FA. John Donald Gass (yes, the same one who described macular hole staging) first published his experience with FA in 1967 (2). FA has revolutionized the evaluation of diabetic retinal disease, central serous chorioretinopathy, vasculitis, and many other conditions.
1964 – Argon and Nd:YAG lasers
William B. Bridges discovered the argon laser, which is capable of blue (488 nm) and green (514 nm) emissions with the property of rapid uptake by hemoglobin and melanin. By 1969, studies demonstrated its efficacy in the treatment of retinal disease and, in the 1970s, the laser gained popularity in iridotomies and argon laser trabeculoplasty (ALT) (3).
That same year, Joseph E. Geusic and Richard G. Smith invented the Nd:YAG laser, a 1064 nm laser that is also capable of producing green (532 nm) light. Daniele Aron-Rosa was the first to use this laser for posterior capsulotomy in the early 1980s (4); it continues to be one of the most common ophthalmology office procedures.
1966 – The Molteno glaucoma implant
In 1907, physicians described using horsehair through a paracentesis to relieve painful end-stage glaucoma (5). Almost half a century later, Anthony Molteno invented the first glaucoma drainage device to reduce intraocular pressure. Several other valves have come to market since but, 50 years and several iterations later, the Molteno remains a common tool in glaucoma treatment (6). The original implant consisted of a single polypropylene plate that created a reservoir for aqueous humor to drain into from a silicone tube placed in the anterior chamber.
1967 – Phacoemulsification
Cataract surgery historically required sutures and a large scleral wound to accommodate removal of the crystalline lens. Because of these large wounds, most cataract surgery took place in the hospital inpatient setting (7). Charles Kelman and Anton Banko solved one half of this problem with the introduction of phacoemulsification. Liquefying the crystalline lens using ultrasound energy meant that removal became as easy as aspirating it out (8). The wounds for the phacoemulsification needle, however, still needed to be enlarged to accommodate rigid IOLs.
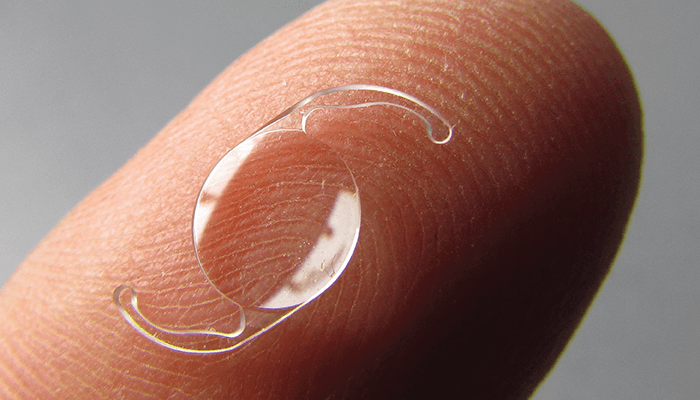
1978 – Foldable IOLs
Because PMMA is rigid and cannot be folded for insertion, the increasingly small phacoemulsification incisions had to be enlarged. The adoption of foldable silicon IOLs, first implanted in 1978, eliminated the need to enlarge the phacoemulsification incision and led to widespread adoption of the technique (9). Though now more commonly made from acrylic, foldable IOLs continue to dominate the market.
1980 – SRK
With just two relatively easy-to-obtain measurements, this formula developed by Donald Sanders, John Retzlaff, and Manus Kraff provided a new degree of accuracy for calculating IOL power (10). This equation remains essential for all ophthalmologists even today due to the important refractive principles it underscores.
Emmetropia = A constant - 0.8(average keratometry) - 2.5(axial length)
SRK is considered an empirical regression formula, which means it is the result of analyzing extensive refractive outcome data.
1993 – Optical coherence tomography (OCT)
The ability to take objective measurements of delicate ocular structures has revolutionized the treatment of many diseases. Based on the principle of low-coherence interferometry, a prototype machine was built and over 5,000 scans were taken at New England Eye Center Tufts Medical Center to create the first OCT atlas in 1996. Nowadays, it is difficult to imagine a time when OCT was not a regular part of the ophthalmology clinic workflow.
1994 – MSICS
Phacoemulsification machines are large, expensive, and can be difficult to move around, and the disposable products needed are not always readily available and affordable. The technology is therefore often unavailable in resource-limited settings. Manual small-incision cataract surgery (MSICS) uses alternative techniques to remove the crystalline lens through a smaller, usually self-sealing scleral incision that is about half the length of standard incisions (11). This technique has become a staple for global ophthalmology work.
1995/1999 – PRK/LASIK FDA approval
Introduced to the US in 1978, radial keratotomy (RK) offered a simple way to reduce moderate amounts of myopia, but is now known to be fraught with inaccuracy, fluctuation, and frustration (12). Photorefractive keratectomy (PRK) and laser in-situ keratomileusis (LASIK) were approved in the mid- to late 1990s and provided a safer, more reliable way to permanently correct refractive error (13).
1998 – STAAR silicone toric IOL FDA approval
Many surgical options existed in the late 1990s to address astigmatism, including arcuate keratotomy, limbal relaxing incisions, and the new PRK and LASIK. These techniques continued to evolve in reliability and accuracy, but it was not until nearly 50 years after the first IOL was implanted that astigmatism could be managed by the IOL itself. When STAAR introduced the first silicone toric IOL, astigmatism management changed forever (14).
2005 – Avastin and the eye
An anti-VEGF medication called AVASTIN (bevacizumab) was approved for use in advanced colon cancers – but the ability to prevent cancerous vascular growth also proved immensely useful in the treatment of neovascular eye diseases. Avastin has been used extensively off-label for intravitreal injection and an ocular form of a related drug, ranibizumab (Lucentis) was approved by the FDA specifically for this use in 2006 (15).
2010 – Barrett II
Improving the accuracy of IOL calculations relied on improving the predictability of effective lens position (ELP), or where the IOL sits postoperatively. The Barrett II formula uses several variables to predict ELP. This theoretical formula uses formal optics and model eye data. The data supported Barrett II as the most accurate IOL formula to date, and it held that title for many years after its development (16).
2016 – SMILE FDA approval
Postoperative ectasia has always represented a major concern in LASIK. Based on the knowledge that the anterior cornea plays the greatest role in structural stability, SMILE offered a solution: removal of the lenticule without the creation of a flap. Data so far seems to point to an even lower ectasia risk than PRK (17). SMILE, also sometimes called LALEX (laser-assisted lens extraction), does not use excimer laser technology; instead, it uses the femtosecond laser originally developed by Ronald Kurtz in the 1990s.
2010s – The MIGS Revolution
For many years, “trabs and tubes” represented the foundation of glaucoma surgery. Goniosynechialysis, endoscopic cyclophotocoagulation (ECP), and trabectome were early minimally invasive glaucoma strategies. Microinvasive glaucoma surgeries (MIGS) such as the iStent inject, Kahook Dual Blade, Hydrus Microstent, OMNI Surgical System, or XEN Gel Stent now allow surgeons to intervene in the treatment of glaucoma earlier than ever. The procedures are also safer and have better results than the simple application of pediatric angle surgery techniques (18). These procedures are microinvasive in that they can be performed at the time of cataract surgery through the incision. These newer innovations allow any anterior segment surgeon to contribute to the treatment of glaucoma.
2017 – The Kane formula and LAL FDA approval
2017 was a big year for advancements in refractive surgery. Jack Kane introduced the most accurate IOL formula to date (19). It uses regression, theoretical optics, and artificial intelligence to deliver supreme accuracy even at extremes of axial length where other equations struggle.
Another layer of accuracy was also introduced when the RxSight Light Adjustable Lens (LAL) achieved FDA approval. This lens has 3.5 D of “wiggle room” or astigmatism correction after surgery using UV light and is adjustable to the quarter diopter (20).
Becoming an innovator
Although these have been some of the most profound discoveries in ophthalmology, modest improvements to technology play a crucial role in innovation, too. The authors of this article have developed an iOS app and accompanying website called IOL Reference. Detailed IOL information is scattered across manufacturers and can be difficult to access; their solution was to catalog all the currently available options in one place with a search function, so that surgeons can quickly find the exact IOL to fit their patient’s needs. The success of IOL Reference demonstrates that finding a problem is the first step to innovation. If you encounter an unsolved problem, struggle with something, or recognize a possibility for optimization, it is likely that others do as well and would benefit from a solution. Without access to massive funding, even small-scale inventions can immediately and significantly improve the specialty.
On the horizon
Many new technologies will likely obtain FDA approval in the coming years. The Gemini refractive capsule maintains the open space of the capsular bag to improve ELP predictability and facilitate the addition of technology or refractive lens exchanges. Additionally, the PerfectLens and LicriEye are postoperatively adjustable IOL options similar to the LAL.
Deep learning is also playing a growing role in ophthalmology and technological advancements and has significant applications in detecting disease, establishing a diagnosis, and predicting outcomes. IDx-DR and EyeNuk have developed a fully autonomous, AI-based diabetic retinopathy diagnostic system. Meanwhile, image-based deep learning is helping to overcome the lack of real-world datasets due to proprietary and privacy concerns. Gurpal Virdi of EyeLabs AI is addressing this problem in glaucoma by using deep learning to generate large volumes of high-quality synthetic retinal ganglion cell apoptotic images. Similarly, Jimmy Chen, ophthalmology resident at UC San Diego’s Shiley Eye Institute, is synthesizing fundus images for the evaluation of retinal diseases. Using synthetic data to train AI algorithms will hasten the technology’s transit into the clinic to improve the detection of early glaucomatous and retinal changes.
Recognize a problem. Identify a solution. Execute a plan. Keep innovating.
The authors are actively working on revolutionizing surgical outcome tracking and anticipating major updates to the IOL Reference app in the coming months to address unmet needs.
References
- S Garg, DD Koch, Steinert’s Cataract Surgery, 4th edition. Elsevier: 2022.
- MF Marmor, JG Ravin, “Fluorescein angiography: Insight and serendipity a half century ago,” Arch Opthalmol, 7, 943 (2011). PMID: 21746986.
- DV Palanker et al., “Fifty years of ophthalmic laser therapy,” Arch Opthalmol, 12, 129 (2011). PMID: 21746986.
- DW Promieńska et al., “The evolution of the anterior capsulotomy,” Wideochir Inne Tech Maloinwazyjne, 14, 12 (2019). PMID: 30766624.
- M Rollet, M Moreau, “Le drainage au crin de la chambre anterieure contre l’hypertonie et la douleur,” Rev Gen Ophtalmol, 24, 289 (1907).
- KS Lim et al., “Glaucoma drainage devices; past, present, and future,” BMJ, 82, 1083 (1998). PMID: 9893602.
- PD Davies et al., “Outpatient cataract surgery 1982-1986,” Eye, 6, 728 (1987). PMID: 3454765.
- G Davis, “The evolution of cataract surgery,” Mo Med, 113, 58 (2016). PMID: 27039493.
- HC Seward, “Folding intraocular lenses: materials and methods,” Br J Opthalmol, 81, 340 (1997). PMID: 9227195.
- T Olsen, “Calculation of intraocular lens power: a review,” Acta Opthalmol Scand, 85, 472 (2007). PMID: 17403024.
- M Ang et al., “Manual small incision cataract surgery (MSICS) with posterior chamber intraocular lens versus extracapsular cataract extraction (ECCE) with posterior chamber intraocular lens for age-related cataract,” Cochrane Database Syst Rev, 18, CD008811 (2014). PMID: 25405603.
- GO Waring et al., “ Results of the Prospective Evaluation of Radial Keratotomy (PERK) study one year ffter surgery,” Ophthalmology, 92, 177 (1985). PMID: 3885128.
- R Ambrósio, S Wilson, “LASIK vs LASEK vs PRK: advantages and indications,” Semin Opthalmol, 18, 2 (2003). PMID: 12759854.
- C Novis, “Astigmatism and toric intraocular lenses,” Curr Opin Ophthalmol, 11, 47 (2000). PMID: 10724827.
- LA Kim, PA D’Amore, “A brief history of anti-VEGF for the treatment of ocular angiogenesis,” AM J Pathol, 181, 376 (2012). PMID: 22749677.
- RB Melles et al., “Accuracy of intraocular lens calculation formulas,” Ophthalmology, 125, 169 (2018). PMID: 28951074.
- M Moshirfar et al., “Ectasia after corneal refractive surgery: a systematic review,” Opthalmol Ther, 10, 753 (2021). PMID: 34417707.
- LE Pillunat et al., “Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents,” Clin Ophthalmol, 11, 1583 (2017). PMID: 28919702.
- RB Melles et al., “Update on intraocular lens calculation formulas,” Ophthalmology, 126, 1334 (2019). PMID: 30980854.
- DV Folden, JR Wong, “Visual outcomes of an enhanced uv protected light adjustable lens using a novel co-managed, open-access methodology,” Clin Ophthalmol, 16, 2413, PMID: 35957659.
