- Bag-in-the-lens (BIL) implants are becoming more advanced, but it’s equally important to expand the patient population able to receive them
- Bean-shaped rings allow even patients with loose zonules or damaged capsular bags to receive BIL implants
- The beans are implanted at the end of a BIL procedure to provide stability and centration while minimizing the need to suture
- Patients with chronic diseases, ocular trauma or simply aging eyes may benefit from bean-shaped rings
Fifteen years ago, the first intraocular lens (IOL) was implanted using the “bag-in-the-lens” (BIL) technique (1), and it has seen increased adoption since then. BIL implantation is of particular benefit in patients at risk of posterior capsule opacification (PCO), sandwiching the two layers of the capsule between the lens haptics, preventing the lenticular epithelial cells that cause opacification from entering the visual axis. Preventing PCO saves money by not only maintaining good vision after cataract surgery, but also by reducing the need for follow-up procedures such as YAG laser capsulotomy.
More recently, we have made further advancements to the BIL implant and how we place it into the eye. The BIL is already available in a toric form, and development is underway for a diffractive model that may reduce higher-order aberrations in some patients. But broadening the options for the implant itself is not enough; there are still many people for whom those choices don’t work well, and there’s still a strong need for ophthalmologists to select their patients very carefully. So in addition to developing new BIL implants, we hope to expand the population of patients who can receive them. One way we’re doing that is through the development of a new device – the bean-shaped ring – that can allow even patients whose capsular integrity is compromised to receive a BIL implant.
An area of unmet need
In patients who have a torn capsule, loose zonules, or any other situation where the capsular bag is incomplete or not fully reliable, it’s difficult to place and center a BIL appropriately. The bean-shaped rings are intended as a capsule enhancement device; they can take over the function of the capsular bag or of the zonules. For instance, if the bag has been damaged by trauma and is no longer complete, you can compensate for the missing portion by inserting a bean-shaped ring, which will allow you to center the lens properly in the eye. And those rings give really beautiful results. When I first started to work on the beans, I nearly said, “Let’s throw this idea away, it’s no good.” But every new device goes through a “teething” stage – and that’s true of the beans as well. In their case, they were difficult to implant, the sizes weren’t always good, and we had to rethink some aspects of their design. And you need the support of the manufacturer to do all of this early developmental work. If the manufacturer doesn’t want to continue, then of course you can’t proceed alone – but luckily, that didn’t happen to us. Our manufacturer, Morcher GmbH (Stuttgart, Germany), was very willing to start over again and again until we got things perfect – so we redid the drawings, and finally, the last set drawings turned out to be exactly what we needed.The bean-shaped ring is a kind of modified capsule tension ring, but it has the advantage of minimizing the suturing of the lens and haptics. When you suture a lens, that suture will resolve with time – unless you use Gore-Tex, which unfortunately is thick, bulky and inelegant. I would far rather have a PMMA structure in the eye, because we’ve been using it since the advent of the IOL after World War II, and we know that it’s still the least immunogenic material you can put in the eye. It’s also thin and flexible, without compromising on strength. So we chose to make the beans out of PMMA, which has given us some room to play with the design – there are several sizes, and you can use them in different combinations to achieve optimal centration of the lens. You can also position them differently; they can go inside the capsule, outside the capsule to be positioned in the sulcus, or it’s even possible to place one (or more) in each position. So far, the results have been excellent.
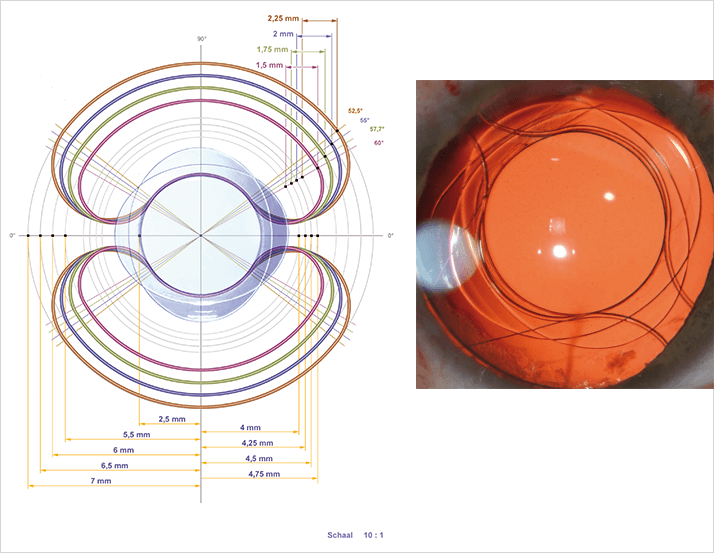
The bean-shaped ring is a kind of modified capsule tension ring, but it has the advantage of minimizing the suturing of the lens and haptics. When you suture a lens, that suture will resolve with time – unless you use Gore-Tex, which unfortunately is thick, bulky and inelegant. I would far rather have a PMMA structure in the eye, because we’ve been using it since the advent of the IOL after World War II, and we know that it’s still the least immunogenic material you can put in the eye. It’s also thin and flexible, without compromising on strength. So we chose to make the beans out of PMMA, which has given us some room to play with the design – there are several sizes, and you can use them in different combinations to achieve optimal centration of the lens. You can also position them differently; they can go inside the capsule, outside the capsule to be positioned in the sulcus, or it’s even possible to place one (or more) in each position. So far, the results have been excellent.
Implanting the rings
Because the rings are flexible, they can pass through an incision as small as 2.2 mm. Any smaller than that and they’ll be difficult to insert – but I haven’t found that to be a problem so far, because in cases where the rings are necessary, half a millimeter’s difference in the incision size doesn’t change much about the surgery or its outcomes. This is especially true if, like me, you make your incisions a little bit closer to the sclera and the limbus. If you know in advance that you’ll be dealing with a difficult case, you can plan ahead. Much of the time, you’ll find that even with a torn capsule, the zonules are not an issue. The capsule support is sufficient, so you can use a regular capsular tension ring. But that isn’t always the case. For example, in post-vitrectomy patients whose surgeons wanted to do a very complete vitrectomy, removing both the primary and secondary vitreous brings the irrigation and aspiration cannula very close to the zonular fibers; often, the zonular fibers are aspirated or cut, which compromises the stability of the lens. Those are the kinds of cases where the bean-shaped rings are required, and if you know the patient’s needs beforehand, you can plan for it.The stage at which you actually implant the ring is either prior to BIL implantation if the stability of the capsular bag is only slightly compromised, or at the end of the surgery. After the BIL has been implanted as far as possible, you can tell whether or not there will be a good, stable position, and whether or not there’s a risk of decentration of the complex due to zonular lysis. Then you can introduce the bean-shaped rings to ensure ongoing stability and centration. In one specific instance, I had a patient with megalocornea. These patients’ eyes have a very large anterior segment and extremely curved corneas; there is no regular lens that can be accommodated by the structure of their eyes. The only lens that could be implanted in the case of my patient was a BIL. But even with that implant, the capsule was so huge that I was afraid of wobbling, which would eventually cause problems at the level of the vitreous – ultimately even leading to breaks in the retina. So I knew I needed a way to stabilize the BIL, and bean-shaped rings were the perfect solution. I had to order custom-sized rings, because the eye was too big for the standard sizes. But the manufacturer made rings specifically for that patient, and they were a success! I’ve found that I actually have a lot of indications for using the beans. Of course, my cases tend to be exceptions to the rule, but those are exactly the patients we get at a referring center for complicated cases. And once you start using the bean-shaped rings, you discover that you can solve quite a lot of problems with them! I described the case of a cataract patient with previous trauma, who needed bean-shaped rings positioned within the capsular bag to stabilize and recenter the BIL (2). That works in many patients with trauma; if you know that only a small part of the capsule is damaged and the remaining zonules are fine, then you can use the beans within the capsular bag. In other cases, where you have chronic disease or simply loose zonules due to aging, you have to use the sulcus, otherwise everything will eventually drop down into the vitreous.
Germinating the idea
The beans came about because I wanted a device that could support an artificial iris as well, so that I could fix the iris in place along with the BIL. I initially tried another device that attached at the sclera, but I didn’t think it was appropriate; scleral fixation causes its own set of problems and complications, so I try to avoid it. The refractive outcomes aren’t as predictable, either, because the calculations don’t reflect the actual position of the lens in the anterior chamber. So I was trying to think of something else that we could use with the sulcus as a reference, and then, little by little, with the help of the think tank at Morcher, the idea for the bean-shaped rings emerged. We’ve been using them to meet various needs in our patient population, and we’re currently preparing a publication based on over 50 cases ranging from Marfan syndrome to trauma and IOL exchange – anything that compromises the quality of the zonules or the capsular bag. We need the publications so that we can commercialize the rings, and so that the Belgian social security system – and hopefully others, too – will provide our patients with reimbursements for the implantations. On behalf of the patients, I’m looking forward to that! I’m very happy with the beans’ results so far, and I would like to see more surgeons working with them. Once you know the trick, they’re easy to implant. And I’d like to see as many patients as possible gain access to them.Marie-José Tassignon is immediate past medical director and head of the ophthalmology department at the Antwerp University Hospital. She is also the developer of the bag-in-the-lens implantation technique to avoid PCO, the main complication of traditional lens-in-the-bag implantation.
References
- MJ Tassignon, “Bag-in-the-lens implantation of intraocular lenses”, J Cataract Refract Surg, 28, 1182–1188 (2002). PMID: 12106726. MJ Tassignon, SN Dhubhghaill, “Bean-shaped ring segment for capsule stretching and centration of bag-in-the-lens cataract surgery”, J Cataract Refract Surg, 40, 8–12 (2014). PMID: 24355717.
