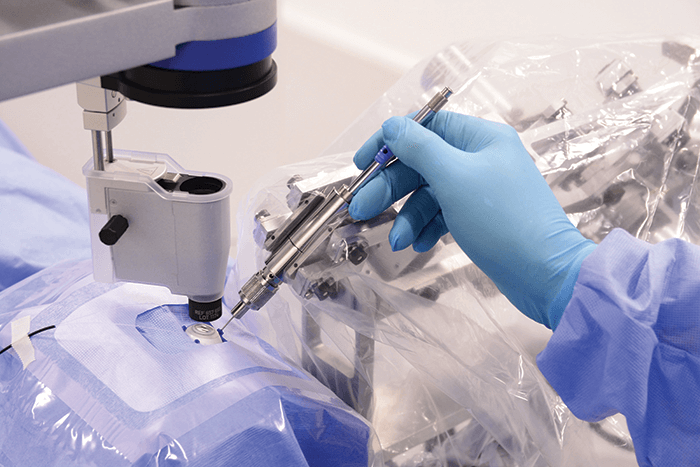
In theory, treating a recent retinal vein occlusion shouldn’t be too hard: cannulate the vein that’s been obstructed with a thrombus and administer a thrombolytic drug. The reality is very different. The cannulation needle needs to be inserted with great precision and held in place for the duration of drug injection – often minutes, given the miniscule lumen of the needle that’s required – making the task all but impossible, even for the most gifted (and daring) of surgeons. Hand tremor limits what can be done in terms of needle placement and the tiniest (unintentional) movements can damage the retina. With this in mind, a team of ophthalmologists and researchers at KU and UZ Leuven have spent the last seven years developing a robotic device that contains a microneedle and surgical stabilizer to help surgeons perform the procedure with micron-level precision (Figure 1).
“In essence, our system leaves low frequency motions of the surgeon unchanged while filtering out high frequency unintentional motions, such as hand tremor, allowing surgeons to make smooth motions that are free from any vibrations,” says Andy Gijbels, one of the engineers who developed the device. What distinguishes their robot from others is that the surgeon’s hand directly co-manipulates the instrument to control the attached microneedle and perform the surgery. “Most surgical robots use a joystick to enhance surgical precision with motion scaling, however this comes with its own problems: the surgeon needs to learn to operate differently because they no longer hold the instrument in their own hands, and the systems are more complex as well as costly,” comments Gijbels. “We found a clever vibration elimination method that enhances surgical precision over 10 times without the need for a joystick.”
As part of an ongoing Phase I trial (1), they used the device to inject ocriplasmin into a blocked retinal vein (0.1 mm in diameter) in a patient with retinal vein occlusion over a seven minute period – the first ever clinical use of a robotic assistance device for this procedure. The clot was successfully lysed and the patient is reported to be recovering well. Peter Stalmans, a vitreoretinal surgeon at UZ Leuven, says, “The robotic device enables us to treat the cause of thrombosis in the retina for the first time.” The team’s next steps include studying the clinical effects of the robotic-assisted procedure in a Phase II trial. The team is also hopeful that the robot will have other uses in the future. “In theory, any vitrectomy could be facilitated by this technology, as could membrane peeling or subretinal injections,” says Stalmans.
References
- Clinicaltrials.gov, “Phase I RVC With Ocriplasmin for CRVO (RVC_CRVO)”, NCT02747030. Available at: bit.ly/leuvenretina. Accessed February 2nd, 2017.
