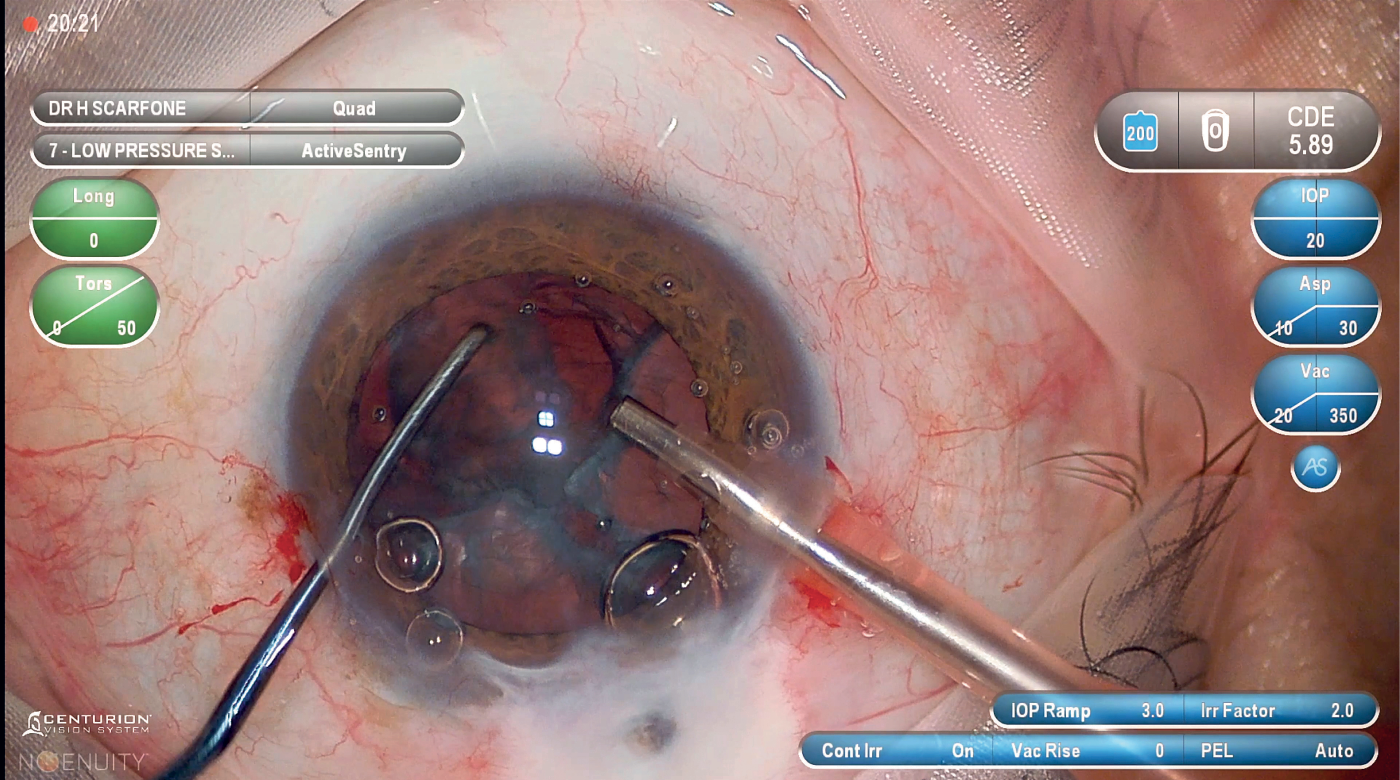
Figure 1: Real-Life Experience with Centurion® with Active Sentry® at More Physiologic IOP
Since its launch in 2019, use of Centurion® with Active Sentry® at more physiologic IOP has been adopted by surgeons globally. Dr. David M. Lubeck (US), Dr. Gàbor B. Scharioth (Germany), Dr. Zaina Al-Mohtaseb (US), and Dr. Hugo Scarfone (Argentina) have each been using Centurion® with Active Sentry® for 2-4 years and are operating at 20-30 mmHg IOP or moving towards those levels. These surgeons were interviewed to discuss their experiences and stated that operating at more physiologic IOP may improve intra- and postoperative outcomes,(1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18) enhance patient satisfaction,(4, 7) have positive effects on surgeon confidence and knowledge transfer, and may reduce procedure time.(5)
Using Centurion® with Active Sentry® at more physiologic IOP improves patient outcomes and provides procedural benefits.
Q: In your experience, what are the advantages in terms of outcomes when performing cataract surgery at more physiologic IOP using Centurion® with Active Sentry®?
Intraoperative outcomes
Dr. Lubeck: Using Centurion® with Active Sentry® at more physiologic IOP has made a positive impact on irrigation solution usage, aspiration and total case time, and has enhanced patient comfort due to mitigation of reverse pupillary block (RPB).(1, 5, 6, 9)
Dr. Scharioth: A study comparing 102 eyes each at infusion pressures of 20 or 60 mmHg using Centurion® with Active Sentry® for phacoemulsification showed benefits in case and aspiration time, and irrigation solution usage for the 20 mmHg group with no differences between groups in ultrasound time.(5) Additionally, even with very small incisions, the anterior chamber remains stable during phacoemulsification at more physiologic IOP.(19) Lastly, RPB is mitigated at more physiologic IOPs,(1) such as around 20 mmHg, which can reduce associated patient pain/discomfort,(6, 9, 20) and stress on the posterior capsule anterior hyaloid membrane.(8)
Dr. Al-Mohtaseb: While the amount of irrigation solution used depends on the patient’s nuclear density,(4) RPB is typically associated with patient discomfort and can be mitigated with fewer IOP fluctuations.(6) I am excited to see the benefits from using Centurion® with Active Sentry® as I move towards operating at 30 mmHg.
Dr Scarfone: Our study evaluated 40 patients each at infusion pressures of 80 or 30 mmHg with comparable nuclear densities who were operated on with Centurion® with Active Sentry®.(9) We found no differences in ultrasound time or use of irrigation solution between the two groups. However, we did find a higher prevalence of anterior vitreous detachment in the 80 mmHg infusion pressure group.(9) Our findings suggest that targeting a more physiological IOP may help control the severity and discomfort of RPB in high-risk patients, such as those who are young, myopic, or have previously undergone vitrectomy.(1, 3, 6)
Abbreviations: IOP = intraocular pressure; MD = Doctor of Medicine; mmHg = mm of mercury; PhD = Doctor of Philosophy; US = United States.
Postoperative outcomes
Dr. Lubeck: Operating at more physiologic IOP reduces corneal swelling and anterior segment inflammation in the early post-operative period, enhances endothelial cell protection, and results in clearer corneas post-operatively.(10, 11, 12, 13, 14) Patients with clearer corneas commonly report improved vision.(21)
Dr. Scharioth: Phacoemulsification at more physiologic IOP alleviates stress on the posterior capsule anterior hyaloid membrane barrier, potentially decreasing lens dust in the anterior vitreous and reducing postoperative inflammation.(8, 9, 15, 22)
Dr. Al-Mohtaseb: As a cornea specialist implanting premium IOLs, I’ve observed less corneal edema and anterior segment inflammation within one day post-surgery when I perform phacoemulsification moving towards a more physiologic IOP.(13) However, nuclear density and probe to cornea proximity also influence postoperative outcomes.(23) Lastly, operating at lower IOP may lead to less change in size of the foveal avascular zone.(16, 17, 18)
“My patients are thrilled when they can see clearly one day after surgery!” - Dr. Al-Mohtaseb
Dr. Scarfone: Our study found no differences in corneal swelling, endothelial cell loss, or postoperative inflammation among 40 patients each, with similar nuclear densities, who were operated on using Centurion® with Active Sentry® at 80 or 30 mmHg.(9) However, only the high infusion pressure group experienced an increase in macular thickness compared to baseline.(9)
Surgeons agree that using Centurion® with Active Sentry® at more physiologic IOP does not impact the anterior chamber volume/depth during surgery.
Post-occlusion surge
Q: Can you describe your experience with post-occlusion surge events when using Centurion® with Active Sentry® at more physiologic IOP?
Dr. Lubeck: The frequency and magnitude of post-occlusion surges are indistinguishable when operating at more physiologic versus higher IOP levels. This ensures minimal impact on the surgery’s flow and efficiency.
Dr. Scharioth: In 102 eyes operated on with Centurion® with Active Sentry® at 20 mmHg, Active Sentry® engaged less during nucleus removal than in the 102 eyes operated on at 60 mmHg.(5)
“Since post-occlusion surge represents the moment of highest risk for complications during the procedure, such as posterior capsule rupture (PCR), the ability to minimize such events using Centurion® with Active Sentry® is valuable.” – Dr. Scharioth
Dr. Al-Mohtaseb: I can’t remember the last time I encountered a detectable post-occlusion surge event using Centurion® with Active Sentry® at more physiologic IOP.
Dr. Scarfone: Suzuki et al.’s study in pig eyes mirrors my clinical experience where Centurion® with Active Sentry® reduces surge volume and enhances anterior chamber stability.(19) I don’t worry about surge events during surgery since the compensatory mechanism kicks in automatically!(5, 19)
Both typical and complex cases can be completed satisfactorily when using Centurion® with Active Sentry® at more physiologic IOP.
Surgeons agree that subgroups of patients, such as those who are high axial myopes, have pseudoexfoliation, have low endothelial cell density, or have denser nucleii, can benefit from the enhanced anterior chamber stability of using Centurion® with Active Sentry® at more physiologic IOP. (20, 24, 25)
Patient satisfaction
Q: How would you describe the level of patient pain, discomfort, and satisfaction when using Centurion® with Active Sentry® at more physiologic IOP?
Dr. Lubeck: Patients are comfortable while operating at more physiologic IOP which allows them to converse with me and position the eye as requested.(20) I find that patients feel empowered and have a sense of pride in contributing to their successful outcomes and sense of well-being.
Dr. Scharioth: Patients rarely complain of discomfort when phacoemulsification is performed with Centurion® with Active Sentry® at more physiologic IOP,(7, 9, 20) are often surprised at how quick the procedure is, and are satisfied post-surgery.
Dr. Al-Mohtaseb: Our patients report they are more comfor table when phacoemulsification is performed at more physiologic IOP.(9, 20)
Dr. Scarfone: My patients feel minimal pain or discomfort when the infusion pressure remains low.(9) In our study, the 30 mmHg pressure group had better subjective perception (measured with the Wong-Baker FACES Pain Rating Scale) than the 80 mmHg infusion pressure group (P=0.0001).(9)
Performing phacoemulsification with Centurion® with Active Sentry® at more physiologic IOP enhances confidence and training.
Surgeon confidence and training
Q: How has using Centurion® with Active Sentry® at more physiologic IOP influenced your confidence and the confidence and learning curve of surgeons adapting to operating at this IOP level?
Dr. Lubeck: Using Centurion® with Active Sentry® at more physiologic IOP is an intuitive experience, bringing me immense satisfaction with outcomes at the end of each day. Initially I was skeptical, like most surgeons, however, I found that adopting these parameters was straightforward and did not require significant changes to my surgical technique.
Dr. Scharioth: I feel safe and confident using Centurion® with Active Sentry® for phacoemulsification at infusion pressures below 30 mmHg, I have even gone below 25 mmHg. Experienced surgeons adapt comfortably to lowering their infusion pressure.
Dr. Al-Mohtaseb: Centurion® with Active Sentry® ensures anterior chamber stability and prevents post occlusion surge,(5) aiding in trainee surgeon education.
Dr. Scarfone: Operating at more physiologic IOP boosts my confidence in both routine and challenging cases and benefits patients. I recommend starting at 50 mmHg and gradually lowering to 30 mmHg as confidence and proficiency develop.
Centurion® with Active Sentry® at more physiologic IOP offers numerous practice benefits, improving efficiency.
Economics
Q: How has using Centurion® with Active Sentry® at more physiologic IOP affected the procedure volume of your practice?
Dr. Lubeck: Performing cataract surgery with Centurion® with Active Sentry® at a more physiologic IOP has yielded intraoperative efficiencies that reduce procedure time.(5)
Dr. Scharioth: Centurion® with Active Sentry® at more physiologic IOP reduces treatment costs of RPB due to its mitigation,(1) lowers case time,(5) and ultimately enhances surgical capacity amidst rising expenses.
Dr. Al-Mohtaseb: In my experience, I perceive that I am more efficient using Centurion® with Active Sentry® moving towards a more physiologic IOP due to lower case time and reduced irrigation solution usage than when operating at higher IOP.(5)
Dr. Scarfone: Centurion® with Active Sentry® at more physiologic IOP reduces anterior vitreous detachment.(9) Recently, the number of surgeries I perform has increased, and my practice is thriving! Efficiencies gained with Centurion® with Active Sentry® as well as the use of premium IOLs leave my patients feeling satisfied and prompts more referrals.
“My patients are very satisfied with their results which I believe has contributed to the practice’s growth. Working alongside my team, we’ve gained confidence and are happier with the work we do, which has led to even better results.” – Dr. Scarfone
Real life experience
Dr. Lubeck: My favorite days are in the OR performing cataract surgery using Centurion® with Active Sentry® at more physiologic IOP. My second favorite days are the first day after surgery where I relive the patients surgical experience and outcomes with them.
Dr. Scharioth: I find satisfaction in performing phacoemulsification using Centurion® with Active Sentry®, especially in complex patients such as those with a hard nucleus, weak zonules, and small pupils, or those with intraoperative floppy iris syndrome.(24, 25)
Dr. Al-Mohtaseb: Every day I perform complex cases with comfort and confidence knowing that the surgery will go smoothly.
Dr. Scarfone: The optic nerve of glaucoma patients is less resilient to hypoxia, often caused by high and fluctuating IOP.(26) I operated on a 68- year old patient with severe glaucoma, perforated filtration bleb, and cornea guttata (Figure 1). Operating with Centurion® with Active Sentry® at 20 mmHg allowed for a fluctuation-free environment and offered protection towards the optic nerve. In these situations, I am confident that I am providing the best care possible for my patients.
CENTURION® VISION SYSTEM IMPORTANT PRODUCT INFORMATION
Caution: Federal (USA) law restricts this device to sale by, or on the order of, a physician.
As part of a properly maintained surgical environment, it is recommended that a backup IOL Injector be made available in the event the AutoSert® IOL Injector Handpiece does not perform as expected.
Indication: The Centurion® Vision System is indicated for emulsification, separation, irrigation, and aspiration of cataracts, residual cortical material and lens epithelial cells, vitreous aspiration and cutting associated with anterior vitrectomy, bipolar coagulation, and intraocular lens injection. The AutoSert® IOL Injector Handpiece is intended to deliver qualified AcrySof® intraocular lenses into the eye following cataract removal.
The AutoSert® IOL Injector Handpiece achieves the functionality of injection of intraocular lenses. The AutoSert® IOL Injector Handpiece is indicated for use with the AcrySof® lenses SN6OWF, SN6AD1, SN6AT3 through SN6AT9, as well as approved AcrySof® lenses that are specifically indicated for use with this inserter, as indicated in the approved labeling of those lenses.
Warnings: Appropriate use of Centurion® Vision System parameters and accessories is impor tant for successful procedures. Use of low vacuum limits, low flow rates, low bottle heights, high power settings, extended power usage, power usage during occlusion conditions (beeping tones), failure to sufficiently aspirate viscoelastic prior to using power, excessively tight incisions, and combinations of the above actions may result in significant temperature increases at incision site and inside the eye, and lead to severe thermal eye tissue damage.
Good clinical practice dictates the testing for adequate irrigation and aspiration flow prior to entering the eye. Ensure that tubings are not occluded or pinched during any phase of operation.
The consumables used in conjunction with ALCON® instrument products constitute a complete surgical system. Use of consumables and handpieces other than those manufactured by Alcon may affect system performance and create potential hazards.
AEs/Complications: Inadver tent actuation of Prime or Tune while a handpiece is in the eye can create a hazardous condition that may result in patient injury. During any ultrasonic procedure, metal particles may result from inadvertent touching of the ultrasonic tip with a second instrument.
Another potential source of metal particles resulting from any ultrasonic handpiece may be the result of ultrasonic energy causing micro abrasion of the ultrasonic tip.
ATTENTION: Refer to the Directions for Use and Operator’s Manual for a complete listing of indications, warnings, cautions and notes.
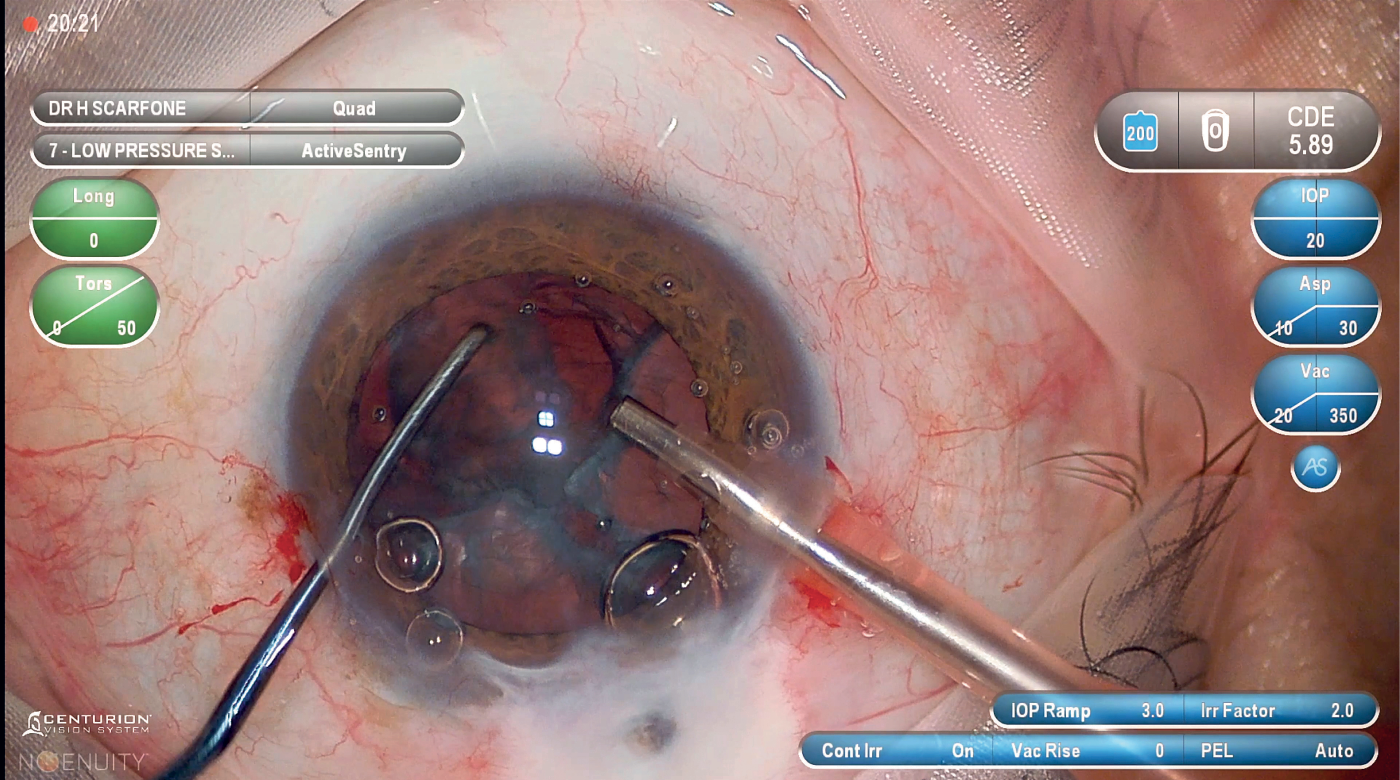
Figure 1: Real-Life Experience with Centurion® with Active Sentry® at More Physiologic IOP
(GLB/IMG-CNT-2400002)
References
- Cionni RJ, Barros MG, Osher RH (2004) Management of lens-iris diaphragm retropulsion syndrome during phacoemulsif ication. J Cataract Refract Surg 30 (5): 953-956.
- Zeppieri M, Tripathy K (2023) Pigment Dispersion Glaucoma. eds). StatPearls Publishing: StatPearls [Internet].
- Bang SP, Joo CK, Jun JH (2017) Reverse pupillary block after implantation of a scleral-sutured posterior chamber intraocular lens: a retrospective, open study. BMC Ophthalmol 17 (1): 35.
- Scarfone HA, Rodriguez ECC (2023) Evalutaion of Early Changes of the Anterior Vitreous Interface After Cataract Surgery, Using Low Pressure Settings Determined by OCT. American Association of Cataract and Refractive Surgery (ASCRS). San Diego, California. May 6, 2023.
- Beres H, de Ortueta D, Buehner B, Scharioth GB (2022) Does low infusion pressure microincision cataract surgery (LIPMICS) reduce frequency of postocclusion breaks? Rom J Ophthalmol 66 (2): 135-139.
- Kang YK, Kim MJ, Kim HK, Chun BY (2017) Clinical Analysis of Ocular Parameters Contributing to Intraoperative Pain during Standard Phacoemulsif ication. J Ophthalmol 2017 9463871.
- Ashkenazy S, DeKeyser Ganz F (2019) The Differentiation Between Pain and Discomfort: A Concept Analysis of Discomfort. Pain Manag Nurs 20 (6): 556-562.
- Kawasaki S, Tasaka Y, Suzuki T, Zheng X, Shiraishi A et al. (2011) Inf luence of elevated intraocular pressure on the posterior chamber-anterior hyaloid membrane barrier during cataract operations. Arch Ophthalmol 129 (6): 751-757.
- Scarfone HA, Rodriguez EC, Ruf iner MG, Riera JJ, Fanego SE et al. (2024) Vitreous lens interface changes after cataract surgery using active f luidics and active sentry with high and low infusion pressure settings. J Cataract Refract Surg 50 (4): 333-338.
- Kokubun TT, Yabana, T, Maekawa S, Yokoyama Y,Kunikata, H, Nakazawa, T (2022) The protective effect of normal-IOP cataract surgery on the corneal endothelium. Japanese Ophthalmological Society. Osaka, Japan. April/May 2021.
- Rauen M (2023) Phacoemulsif ication at high IOP and physiologic IOP: Impact on posterior segment physiology. Association of Cataract and Refractive Surgery (ASCRS) San Diego, California. May 7, 2023.
- Suzuki H, Oki K, Shiwa T, Oharazawa H, Takahashi H (2009) Effect of bottle height on the corneal endothelium during phacoemulsification. J Cataract Refract Surg 35 (11): 2014-2017.
- Vasavada AR, Praveen MR, Vasavada VA, Vasavada VA, Raj SM et al. (2010) Impact of high and low aspiration parameters on postoperative outcomes of phacoemulsification: randomized clinical trial. J Cataract Refract Surg 36 (4): 588-593.
- Vasavada V, Raj SM, Praveen MR, Vasavada AR, Henderson BA et al. (2014) Real-time dynamic intraocular pressure f luctuations during microcoaxial phacoemulsif ication using different aspiration f low rates and their impact on early postoperative outcomes: a randomized clinical trial. J Refract Surg 30 (8): 534-540.
- Núñez-Álvarez C, del Olmo Aguado S, Merayo-Lloves J, Osborne N (2015) Damage to the corneal endothelial cell in situ is attenuated by long wave red light. ARVO Annual Meeting Abstract. Denver, Colorado. June.
- Zhao Z, Wen W, Jiang C, Lu Y (2018) Changes in macular vasculature after uncomplicated phacoemulsif ication surgery: Optical coherence tomography angiography study. J Cataract Refract Surg 44 (4): 453-458.
- Liu J, Liu Q, Yu H, Xia Y, Zhang H et al. (2021) Microvascular Changes in Macular Area After Phacoemulsif ication and Its Inf luencing Factors Assessed by Optical Coherence Tomography Angiography. Ther Clin Risk Manag 17 405-414.
- Nourinia R, Kiani A, Hassanpour K, Nikkhah H, Faramarzi A et al. (2023) Optical coherence tomography angiography parameters after cataract surgery. Int Ophthalmol 43 (8): 2679-2686.
- Suzuki H, Igarashi T, Takahashi H (2023) Effect of a new phacoemulsification and aspiration handpiece on anterior chamber stability. J Cataract Refract Surg 49 (1): 91-96.
- Liu Y, Hong J, Chen X (2023) Comparisons of the clinical outcomes of Centurion(®) active f luidics system with a low IOP setting and gravity f luidics system with a normal IOP setting for cataract patients with low corneal endothelial cell density. Front Med (Lausanne) 10 1294808.
- Mayo Clinic (Web Page) Fuch’s dystrophy. Updated March 5, 2022. Available online at: https://www.mayoclinic.org/diseasesconditions/ fuchs-dystrophy/symptomscauses/ syc-20352727. Accessed: January 18, 2024.
- Sridhar U, Tripathy K (2023) Lens-Induced Inflammation. eds). StatPearls Publishing: StatPearls [Internet].
- Kausar A, Farooq S, Akhter W, Akhtar N (2015) Transient Corneal Edema After Phacoemulsification. Journal of the College of Physicians and Surgeons Pakistan 25 (7): 505-509.
- Jirásková N, Stepanov A (2021) OUR EXPERIENCE WITH ACTIVE SENTRY AND CENTURION OZIL HANDPIECES. Cesk Slov Oftalmol 77 (1): 18-21.
- Kim HW, Kim I, Kim HS, Kim EC (2023) The comparison of handpiece anti-surge system and main body in cataract surgery. medRxiv
-
Luo Y, Xu G, Li H, Ma T, Ye Z et al. (2023) Application of the Active-Fluidics System in Phacoemulsification: A Review. J Clin Med 12 (2): 611.
