When a tumor is discovered, determining whether it is malignant (and if not, the likelihood of future malignancy) is crucial. However, patients with melanocytic choroidal tumors can present a diagnostic and prognostic challenge. To help, consultant ophthalmologist Bertil Damato devised the MOLES acronym, which highlights the most informative clinical features of a tumor (1) – and here, he shares the process of developing this system and the benefits it could provide.
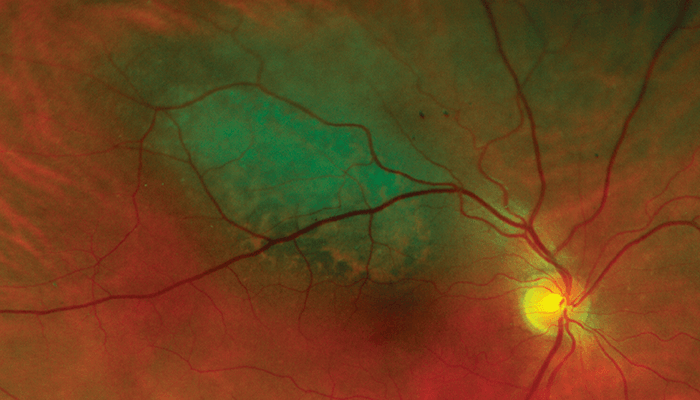
In 2018, when I joined the Nuffield Laboratory of Ophthalmology at the University of Oxford, UK, after five enjoyable and productive years at the University of California, San Francisco, USA, I set about tackling the “suspicious nevus problem.” Hospital eye clinics across the UK (and, no doubt, elsewhere) are inundated with patients with melanocytic choroidal tumors, very few of which will ever show malignant growth. But I have also seen too many patients with melanoma referred for specialist opinions only after months or years of observation. I knew I had to devise a simple acronym or mnemonic to remind non-experts of the suspicious features of ocular melanoma – collar-stud shape, lipofuscin, large size, documented growth, and retinal detachment.

After a number of weeks of deep thought, I came up with the MOLES acronym. The letters stand for Mushroom shape, Orange pigment, Large size, Enlargement, and Subretinal fluid – and “moles” also happens to be the lay term for “nevi.” I knew this acronym would be more useful if it formed the basis of a scoring system so, eventually, I developed a simple system whereby each indicator is scored between 0 and 2 according to whether it is absent or minimal [0], uncertain [1], or definite [2] – and then categorizing tumors as “common nevus,” “low-risk nevus,” “high-risk nevus,” or “probable melanoma,” according to whether the sum of these five scores is 0, 1, 2, or more than 2, respectively.
MOLES should help non-experts estimate the likelihood of malignancy in melanocytic choroidal tumors to expedite the treatment of patients with melanoma and avoid excessive surveillance of patients with nevi. I am confident that the MOLES acronym and scoring system will empower ophthalmologists to manage their patients more efficiently, saving time and money for patients and healthcare services while avoiding delays in the diagnosis of melanoma so that opportunities for preventing metastasis, loss of vision, or enucleation are enhanced.
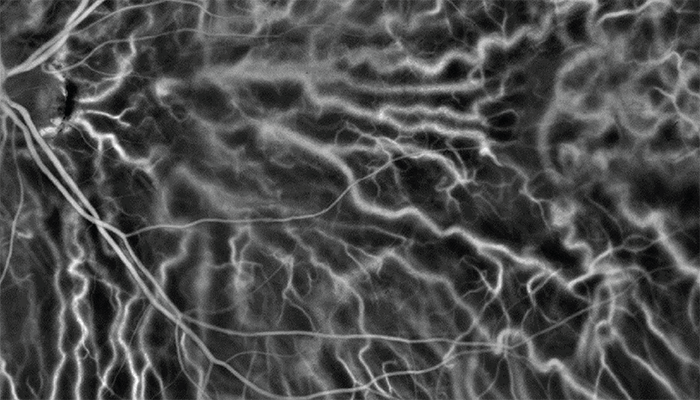
Unlike the helpful TFSOM-DIM system currently in use, MOLES does not include the internal acoustic reflectivity of the tumor. As a system, it can therefore be used when ultrasonography is not possible, either because the necessary skills and equipment are not available or because the tumor is being assessed remotely (through virtual clinics or when triaging referrals via color photographs, OCT scans, or fundus autofluorescence imaging without seeing the patient in person). TSFOM-DIM and MOLES are therefore complementary, providing different benefits in different environments.
Although MOLES performed well when evaluated by ocular oncologists at Moorfields Eye Hospital in London, UK, it must be assessed in a wide variety of real-world situations not only in the UK, but elsewhere as well. At St. Erik Eye Hospital in Stockholm, Sweden, where I now work, we have begun receiving referrals with a MOLES score. Further, there would seem to be scope for educational programs to improve the detection of orange pigment and subretinal fluid on which MOLES depends. I expect that MOLES will become more useful as fundus imaging improves and more ubiquitous as teleophthalmology becomes more widespread.
References
- BE Damato, Eye (Lond), [Online ahead of print] (2022). PMID: 35764877.
