The stellar panel of experts included: Francesco Oddone, Head of Operative Unit, IRCCS Fondazione G.B. Bietti, Rome, Italy
Ike Ahmed, Assistant Professor, University of Toronto, Canada
Keith Barton, Consultant Ophthalmic Surgeon, Moorfields Eye Hospital, London, UK
To establish whether a given procedure meets a medical need, we must define that need. In other words, what is the intervention’s desired endpoint? In glaucoma surgery, desired outcomes are often expressed as IOP measurements. The actual value of those targets, however, varies from patient to patient. Factors that determine IOP target, says Keith Barton, include two fundamentally different considerations: the likelihood of progression and the likely risk to vision loss should progression occur. “In patients with paracentral field defects, even a small risk of progression is undesirable because of the high risk to vision. And young patients, who can expect to live with glaucoma for decades, have a high cumulative risk of progression. Both groups therefore need low target IOPs.” But low IOPs may be challenging to achieve. What options do surgeons have?
“The idea that we should always aim for IOPs of less than 18 mmHg is misguided – many patients need much lower pressures.” – Keith Barton
Barton suggests that subconjunctival MIGS devices meet this need better than other procedures. “They reduce IOP to a greater extent than internal MIGS and, in comparison with trabeculectomy, they’re more straightforward and need less follow-up. For complex patients, surgery needs to be simple, predictable, safe, and effective.” Does PRESERFLO™ MicroShunt meet these criteria?
The data doesn’t lie
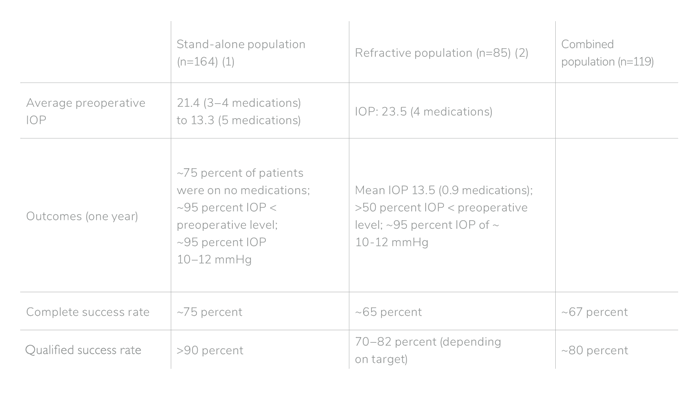
We can answer that question by referring to observed outcomes. Ike Ahmed’s dataset is the result of seven years (1,000 eyes) of experience with the PRESERFLO™ MicroShunt. His records include a retrospective cohort design study of 368 patients distributed among three categories (see box: “Key PRESERFLO™ MicroShunt Outcomes”): those suitable for a stand-alone PRESERFLO™ MicroShunt procedure, those with refractive glaucoma, and those for whom combined PRESERFLO™ MicroShunt-phacoemulsification procedures are indicated.
Ahmed’s experience is that the vast majority of PRESERFLO™ MicroShunt patients maintain target IOP throughout postoperative year one. “We observed remarkably consistent, durable IOP control – better than Xen or trabeculectomy over the first two months.” This, says Ahmed, may partly explain the faster and more complete visual recovery seen in PRESERFLO™ MicroShunt patients. Overall, the procedure gave a complete success rate of ~65–75 percent, and a qualified success rate of ~70–90 percent.
Ahmed also notes that PRESERFLO™ MicroShunt has very low rates of complications and postoperative interventions (1, 2, 3). “Hypotony is extremely rare – testament to PRESERFLO™ MicroShunt’s design.” He emphasises PRESERFLO™ MicroShunt’s low needling rates: 8.5 percent in standalone patients, 11.8 percent in refractory patients, and 24 percent in combined procedure patients (where phacoemulsification-associated inflammation results in a higher needling rate). But these enviable outcomes, says Ahmed, require surgeons to pay attention to best practice. “For example, we find that higher dose mitomycin (0.4–0.5 mg/mL) correlates with higher success rates, lower needling rates, and a more consistent postoperative IOP course.”
Francesco Oddone supports Ahmed’s endorsement of PRESERFLO™ MicroShunt safety, citing a small retrospective study (3) showing that PRESERFLO™ MicroShunt maintains lower IOP (~12 mmHg) than Xen, has a slightly higher success rate at both oneand two-year timepoints, and requires less postoperative bleb management. “Furthermore,” says Oddone, “comparing this study with Ahmed’s data on Xen versus trabeculectomy indicates that postoperative intervention rates were much lower with PRESERFLO™ MicroShunt at one year than with Xen or trabeculectomy at two years.” Because most postoperative intervention occurs soon after surgery, Oddone says it is likely that PRESERFLO™ MicroShunt will maintain its superior profile during postoperative year two.
The conclusion? Ahmed is clear: “We still need long-term data, but initial results indicate that PRESERFLO™ MicroShunt provides consistent IOP control, excellent bleb morphology, and a high degree of safety.”
“Patients appreciate the speed of recovery and the consistent, reliable outcomes achieved with PRESERFLO™ MicroShunt; these features differentiate the device from competitors.” – Ike Ahmed
How does PRESERFLO™ MicroShunt do it?
Why is PRESERFLO™ MicroShunt more consistent and reliable than competing surgical options? Part of the answer, says Oddone, is that other procedures are intrinsically variable and non-standardized. “For example, in trabeculectomies variable tension in scleral flap sutures influences outcomes and postoperative intervention rates.” Sources of variability in other procedures may include the need to open the anterior chamber and fill it with viscoelastic or uncertainty regarding the optimal device placement (subconjunctival or sub-Tenon’s).
In addition, PRESERFLO™ MicroShunt has intrinsic advantages. “In my practice, it requires only a 20-minute procedure,” says Oddone. “Scleral flap formation, sclerotomy, and iridectomy are unnecessary and cauterization is limited to the 1.5 mm2 needle entry site.” Furthermore, the conjunctiva is managed much as for trabeculectomy; many surgeons therefore already have the necessary skills. Similarly, the ab externo route is inherently more predictable in that it permits total control of device placement. “This reduces the risk of eventual failure,” says Oddone. Barton agrees: “Ab externo approaches such as PRESERFLO™ MicroShunt allow precise, sub-Tenon’s device placement; ab interno approaches such as Xen don’t allow that.” Similarly, the external permits controlled sub-Tenon’s mitomycin placement; this is important, says Ahmed, because posterior application of mitomycin – along with posterior positioning of the implant – helps achieve posterior flow, thereby contributing to the diffuse, lowlying blebs associated with PRESERFLO™ MicroShunt.
Conclusions
PRESERFLO™ MicroShunt’s predictable outcomes are probably related to i) improved safety and biocompatibility due to use of SIBS polymer; ii) controlled and standardized outflow due to lumen length and diameter; iii) reliance on standard ophthalmosurgical skills that make it simple to adopt; iv) use of the ab externo route to keep surgery simpler and safer; and v) the standardized kit provided with each device to support predictable outcomes. These advantages make surgeons more confident and outcomes more predictable and consistent.
“The standardized set of PRESERFLO™ MicroShunt instruments minimizes surgical variance.” – Francesco Oddone
Key PRESERFLO™ MicroShunt Outcomes from Ike Ahmed’s Clinic
• Patient population:
• POAG and secondary glaucomas (>50 percent with advanced disease)
• Recruitment during 2015–2019
• Diverse ethnicities
• Definitions:
• Complete success = IOP 6–14, no medications (1, 2) or IOP ≤18 at two consecutive follow ups after three months, no medications, surgery or other therapy (3)
• Qualified success = IOP 6–14 with medications (1, 2), IOP ≤18, with/without medications, no additional interventions (3)
• Refractive cases = patients who had failed at least one conjunctival surgery
PP-PMS-EMEA-0253 - Date of preparation: June 2021
References
- B Schlenker et al., Am J Ophthalmol, 215, 141 (2020). PMID: 32173344.
- G Durr et al., Br J Ophthalmol (2020). PMID: 33097520.
- L Scheres et al., Acta Ophthalmol, 99, e433 (2021). PMID: 32909682.
